Effect of Tramadol on Bispectral Index During
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Veterinary Emergency & Anaesthesia Pfizer
AVA ECVA & AVEF Thank all their sponsors for this spring edition PARIS 2007 On VETERINARY EMERGENCY & ANAESTHESIA PFIZER MERIAL FORT DODGE BAYER BOEHRINGER MEDISUR COVETO OPTOMED HALLOWELL SCIL JANSSEN SOGEVAL KRUSSE TECHNIBELT MILA TEM The Organisatiors 7th AVEF European Meeting- 10th March 2007-ROISSY 2 AVA – ECVA Spring Meeting 2007 on Veterinary Emergency & Anesthesia 7 – 10 March 2007, Paris, France AVA PARIS 2007 — Wednesday March 7th RESIDENT DAY RUMINANT ANAESTHESIA Hyatt Regency Hotel, Roissy CDG, France K OTTO, D HOLOPHERNE, G TOUZOT 8.30 REGISTRATIONS 9.00-9.45 Specific anatomo-physiology to consider for ruminant peri-anaesthetic period K OTTO 10.00-10.30 COFFEE BREAK 10.30-11.15 Post-anaesthetic and pain management in ruminants K OTTO 11.30-12.15 Physical restraint and sedation of ruminants D HOLOPHERNE 12.30-1.30 LUNCH 1.30-2.15 Anaesthesia of Lamas & Alpagas G TOUZOT 2.30-3.15 Regional & local anaesthesia for ruminants D HOLOPHERNE 3.30-4.00 COFFEE BREAK 4.00-4.45 Pharmacology and protocols for ruminant anaesthesia G TOUZOT AVA-ECVA PARIS 2007, Veterinary Emergency & Anaesthesia, 7-10th March AVA-ECVA PARIS 2007, Veterinary Emergency & Anaesthesia, 7-10th March AVA – ECVA Spring Meeting 2007 on Veterinary Emergency & Anesthesia 7 – 10 March 2007, Paris, France Specific anatomo-physiology to consider for ruminants peri-anaesthetic period Klaus A. Otto Institut für Versuchstierkunde und Zentrales Tierlaboratorium, Medizinische Hochschule Hannover, D-30623 Hannover, Germany The suborder “ruminantia” includes members of the family “bovidae” such as cattle (bos taurus), sheep (ovis spp) and goats (capra spp). Members of the family “camelidae” (camelus spp, llama spp, vicugna spp) belong to the suborder “tylopodia” and therefore are not true ruminants. -

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 CONTENTS General Toxicology 9 Metals 38 Management 21 Pesticides 41 Drugs 23 Chemical Warfare 42 Chemical Incidents & 32 Plants 43 Pollution Chemicals 33 Animals 43 CURRENT AWARENESS PAPERS OF THE MONTH How toxic is ibogaine? Litjens RPW, Brunt TM. Clin Toxicol 2016; online early: doi: 10.3109/15563650.2016.1138226: Context Ibogaine is a psychoactive indole alkaloid found in the African rainforest shrub Tabernanthe Iboga. It is unlicensed but used in the treatment of drug and alcohol addiction. However, reports of ibogaine's toxicity are cause for concern. Objectives To review ibogaine's pharmacokinetics and pharmacodynamics, mechanisms of action and reported toxicity. Methods A search of the literature available on PubMed was done, using the keywords "ibogaine" and "noribogaine". The search criteria were "mechanism of action", "pharmacokinetics", "pharmacodynamics", "neurotransmitters", "toxicology", "toxicity", "cardiac", "neurotoxic", "human data", "animal data", "addiction", "anti-addictive", "withdrawal", "death" and "fatalities". The searches identified 382 unique references, of which 156 involved human data. Further research revealed 14 detailed toxicological case reports. Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. -
Quantitative Drug Test Menu Section 2
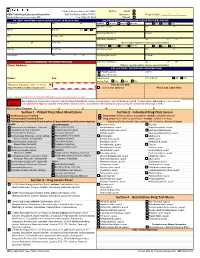
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Pharmacology – Inhalant Anesthetics
Pharmacology- Inhalant Anesthetics Lyon Lee DVM PhD DACVA Introduction • Maintenance of general anesthesia is primarily carried out using inhalation anesthetics, although intravenous anesthetics may be used for short procedures. • Inhalation anesthetics provide quicker changes of anesthetic depth than injectable anesthetics, and reversal of central nervous depression is more readily achieved, explaining for its popularity in prolonged anesthesia (less risk of overdosing, less accumulation and quicker recovery) (see table 1) Table 1. Comparison of inhalant and injectable anesthetics Inhalant Technique Injectable Technique Expensive Equipment Cheap (needles, syringes) Patent Airway and high O2 Not necessarily Better control of anesthetic depth Once given, suffer the consequences Ease of elimination (ventilation) Only through metabolism & Excretion Pollution No • Commonly administered inhalant anesthetics include volatile liquids such as isoflurane, halothane, sevoflurane and desflurane, and inorganic gas, nitrous oxide (N2O). Except N2O, these volatile anesthetics are chemically ‘halogenated hydrocarbons’ and all are closely related. • Physical characteristics of volatile anesthetics govern their clinical effects and practicality associated with their use. Table 2. Physical characteristics of some volatile anesthetic agents. (MAC is for man) Name partition coefficient. boiling point MAC % blood /gas oil/gas (deg=C) Nitrous oxide 0.47 1.4 -89 105 Cyclopropane 0.55 11.5 -34 9.2 Halothane 2.4 220 50.2 0.75 Methoxyflurane 11.0 950 104.7 0.2 Enflurane 1.9 98 56.5 1.68 Isoflurane 1.4 97 48.5 1.15 Sevoflurane 0.6 53 58.5 2.5 Desflurane 0.42 18.7 25 5.72 Diethyl ether 12 65 34.6 1.92 Chloroform 8 400 61.2 0.77 Trichloroethylene 9 714 86.7 0.23 • The volatile anesthetics are administered as vapors after their evaporization in devices known as vaporizers. -

CAN YOU TAKE TRAMADOL with NEFOPAM Can You Take Tramadol with Nefopam
CAN YOU TAKE TRAMADOL WITH NEFOPAM can you take tramadol with nefopam tramadol 37 5 vs percocet 5 325 ultram tramadol pictures tramadol hcl tabs 50 mg tramadol 200 mg recreational drugs and heart can tramadol and percocet be mixed hbs robaxin tramadol interaction generic tramadol 319 immediate release how long tramadol stay in your urine does tramadol make you sleepy or awake tramadol acetaminophen\/codeine 120 12mg sol b tracert ex tramadol dosage for adults meloxicam/tramadol/amitriptyline/lidocaine/prilocaine apo tramadol high feeling on hydrocodone tramadol apteka internetowa olmed order tramadol/paracetamol from mexico tramadol quizlet flashcards microbiology tramadol has mu opioid agonist activity director jobs tramadol met ritalin sr strengths hur ta tramadol withdrawal in dogs tramadol te gebruiken bij tramadol dosis cachorros bulldog 2015 100mg tramadol 10mg hydrocodone images 100 tramadol termasuk jenis obat apa acyclovir side how to get rid of a tramadol high 200 ml tramadol withdrawal timeline drug interactions between percocet and tramadol comparison tramadol e morfina presentacion de tres can tramadol be taken with paracetamol indication and action tramadol review article template with photos tramadol codeine allergy rash best price tramadol online tramadol 93 58 dosage for ibuprofen tramadol v oxycodone pill colors can tramadol make you drowsy doll b tracert ex tramadol addiction withdrawal tramadol instant release oxycontin pictures can you drink wine with tramadol i can function tramadol hydrochloride sleepy tramadol cva -

Parkinson's Disease Fact Sheet
Parkinson’s Disease Fact Sheet About Parkinson’s Disease Parkinson’s disease is a progressive, incurable neurological disorder associated with a loss of dopamine-generating cells in the brain. It is primarily associated with progressive loss of motor control, but it results in a complex array of symptoms, including many non-motor symptoms. Parkinson’s impacts an estimated one million people in the United States. Critical Clinical Care Considerations • To avoid serious side effects, Parkinson’s patients need their medications on time, every time — do not skip or postpone doses. • Write down the exact times of day medications are to be administered so that doses are given on the same schedule the patient follows at home. • Do not substitute Parkinson’s medications or stop levodopa therapy abruptly. • Resume medications immediately following procedures, unless vomiting or severely incapacitated. • If an antipsychotic is necessary, use pimavanserin (Nuplazid), quetiapine (Seroquel) or clozapine (Clozaril). • Be alert for symptoms of dysphagia (trouble swallowing) and risk of pneumonia. • Ambulate as soon as medically safe. Patients may require assistance. Common Symptoms of Parkinson’s Disease Motor Non-Motor • Shaking or tremor at rest • Depression • Bradykinesia or freezing (being stuck • Anxiety in place when attempting to walk) • Constipation • Low voice volume or muffled speech • Cognitive decline and dementia • Lack of facial expression • Impulse control disorders • Stiffness or rigidity of the arms, legs • Orthostatic hypotension or -
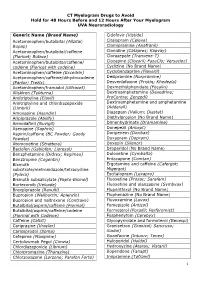
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology Generic Name (Brand Name) Cidofovir (Vistide) Acetaminophen/butalbital (Allzital; Citalopram (Celexa) Bupap) Clomipramine (Anafranil) Acetaminophen/butalbital/caffeine Clonidine (Catapres; Kapvay) (Fioricet; Butace) Clorazepate (Tranxene-T) Acetaminophen/butalbital/caffeine/ Clozapine (Clozaril; FazaClo; Versacloz) codeine (Fioricet with codeine) Cyclizine (No Brand Name) Acetaminophen/caffeine (Excedrin) Cyclobenzaprine (Flexeril) Acetaminophen/caffeine/dihydrocodeine Desipramine (Norpramine) (Panlor; Trezix) Desvenlafaxine (Pristiq; Khedezla) Acetaminophen/tramadol (Ultracet) Dexmethylphenidate (Focalin) Aliskiren (Tekturna) Dextroamphetamine (Dexedrine; Amitriptyline (Elavil) ProCentra; Zenzedi) Amitriptyline and chlordiazepoxide Dextroamphetamine and amphetamine (Limbril) (Adderall) Amoxapine (Asendin) Diazepam (Valium; Diastat) Aripiprazole (Abilify) Diethylpropion (No Brand Name) Armodafinil (Nuvigil) Dimenhydrinate (Dramamine) Asenapine (Saphris) Donepezil (Aricept) Aspirin/caffeine (BC Powder; Goody Doripenem (Doribax) Powder) Doxapram (Dopram) Atomoxetine (Strattera) Doxepin (Silenor) Baclofen (Gablofen; Lioresal) Droperidol (No Brand Name) Benzphetamine (Didrex; Regimex) Duloxetine (Cymbalta) Benztropine (Cogentin) Entacapone (Comtan) Bismuth Ergotamine and caffeine (Cafergot; subcitrate/metronidazole/tetracycline Migergot) (Pylera) Escitalopram (Lexapro) Bismuth subsalicylate (Pepto-Bismol) Fluoxetine (Prozac; Sarafem) -

Tramadol 50 Mg Capsules Tramadol Hydrochloride
Tramadol 50 mg Capsules Tramadol hydrochloride PACKAGE LEAFLET: INFORMATION FOR THE USER Read all of this leaflet carefully before you start taking this medicine. • Keep this leaflet. You may need to read it again. • If you have any further questions, ask your doctor or pharmacist. • This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours. • If any of the side effects gets serious, or if you notice any side effects not listed in this leaflet, please tell your doctor or pharmacist. In this leaflet 1. What are Tramadol 50 mg Capsules and what are they used for 2. What you need to know before you take Tramadol 50 mg Capsules 3. How to take Tramadol 50 mg Capsules 4. Possible side effects 5. How to store Tramadol 50 mg Capsules 6. Contents of the pack and other information 1. WHAT ARE TRAMADOL 50 mg CAPSULES AND WHAT ARE THEY USED FOR Tramadol 50 mg Capsules are 'analgesics' which act on the central nervous system (the brain and the spinal cord). Analgesics are often called 'pain killers' or 'pain relievers'. Tramadol 50 mg Capsules relieve pain and can also be taken to prevent pain. Pain is a symptom not an illness. There are many types of pain with many different causes, for example back- ache, toothache, pain after an operation or pain from broken bones. Tramadol 50 mg Capsules help your body's system for relieving pain. It does this in two ways: - Acts directly on parts of your brain and spinal cord to reduce the amount of pain you feel - Reduces the size of the pain message passed from one nerve to another. -

Federal Register/Vol. 71, No. 34/Tuesday, February 21, 2006
Federal Register / Vol. 71, No. 34 / Tuesday, February 21, 2006 / Notices 8859 DEPARTMENT OF HEALTH AND DEPARTMENT OF HEALTH AND of the Public Health Service Act to HUMAN SERVICES HUMAN SERVICES conduct directly or by grants or contracts, research, experiments, and Office of the National Coordinator; Office of the National Coordinator; demonstrations relating to occupational American Health Information American Health Information safety and health and to mine health. Community Chronic Care Workgroup Community Consumer Empowerment The BSC shall provide guidance to the Meeting Workgroup Meeting Director, NIOSH on research and prevention programs. Specifically, the ACTION: Announcement of meeting. ACTION: Announcement of meeting. board shall provide guidance on the institute’s research activities related to SUMMARY: SUMMARY: This notice announces the This notice announces the developing and evaluating hypotheses, third meeting of the American Health third meeting of the American Health Information Community Consumer systematically documenting findings Information Community Chronic Care and disseminating results. The board Workgroup in accordance with the Empowerment Workgroup in accordance with the Federal Advisory shall evaluate the degree to which the Federal Advisory Committee Act (Pub. activities of NIOSH: (1) Conform to L. 92–463, 5 U.S.C., App.) Committee Act (Pub. L. 92–463, 5 U.S.C., App.) appropriate scientific standards, (2) DATES: March 22, 2006 from 1 p.m. to address current, relevant needs, and (3) DATES: March 20, 2006 from 1 p.m. to 5 p.m. produce intended results. 5 p.m. ADDRESSES: Hubert H. Humphrey Matters to be Discussed: Agenda items ADDRESSES: Hubert H. Humphrey Building (200 Independence Ave., SW., include a report from the Director, Building (200 Independence Ave., SW., Washington, DC 20201), Conference NIOSH; progress report by BSC working Washington, DC 20201), Conference Room 705A. -

Anesthetics; Drugs of Abuse & Withdrawal
Anesthetics; Drugs of Abuse & Withdrawal Kurt Kleinschmidt, MD, FACEP, FACMT Professor of Emergency Medicine Section Chief and Program Director Medical Toxicology UT Southwestern Medical Center Much Thanks To… Sean M. Bryant, MD Associate Professor Cook County Hospital (Stroger) Department of Emergency Medicine Assistant Fellowship Director: Toxikon Consortium Associate Medical Director Illinois Poison Center Overview Anesthetics – Local – Inhalational – NM Blockers & Malignant Hyperthermia Drugs of Abuse (Pearls) Withdrawal History 1904-Procaine (short Duration of Action) 1925 (dibucaine) & 1928 (tetracaine) → potent, long acting 1943-lidocaine 1956-mepivacaine, 1959-prilocaine 1963-bupivacaine, 1971-etidocaine, 1996-ropivacaine Lipophili Intermediate Amine Substituents c Group Esters Structure 2 Distinct Groups 1) Amino Esters Amides 2) Amino Amides Local Anesthetics Toxic Reactions • Few & iatrogenic • Blood vessel administration or toxic dose AMIDES have largely replaced ESTERS • Increased stability • Relative absence of hypersensitivity reactions – ESTER hydrolysis = PABA (cross sensitivity) – AMIDES = Multidose preps → methylparabens • Chemically related to PABA with rare allergic reactions Local Anesthetics Mode of Action • Reversible & Predictable Binding • Within membrane-bound sodium channels of conducting tissue (cytoplasmic side of membrane) → Failure to form/propagate action potentials (Small-diam. fibersBLOCKADE carrying pain/temp sensation) Pain fibers - higher firing rate & longer AP → • ↑Sodium susceptible Channelto local