Cellular Processes 7 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Blueprint Genetics Comprehensive Growth Disorders / Skeletal
Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel Test code: MA4301 Is a 374 gene panel that includes assessment of non-coding variants. This panel covers the majority of the genes listed in the Nosology 2015 (PMID: 26394607) and all genes in our Malformation category that cause growth retardation, short stature or skeletal dysplasia and is therefore a powerful diagnostic tool. It is ideal for patients suspected to have a syndromic or an isolated growth disorder or a skeletal dysplasia. About Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders This panel covers a broad spectrum of diseases associated with growth retardation, short stature or skeletal dysplasia. Many of these conditions have overlapping features which can make clinical diagnosis a challenge. Genetic diagnostics is therefore the most efficient way to subtype the diseases and enable individualized treatment and management decisions. Moreover, detection of causative mutations establishes the mode of inheritance in the family which is essential for informed genetic counseling. For additional information regarding the conditions tested on this panel, please refer to the National Organization for Rare Disorders and / or GeneReviews. Availability 4 weeks Gene Set Description Genes in the Comprehensive Growth Disorders / Skeletal Dysplasias and Disorders Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ACAN# Spondyloepimetaphyseal dysplasia, aggrecan type, AD/AR 20 56 Spondyloepiphyseal dysplasia, Kimberley -

Prenatalscreen® Standard Technical Report
About PrenatalScreen® Prenatal Test PrenatalScreen® Prenatal Test is a genetic test that analyses fetal DNA, obtained from CVS or amniotic fluid following an invasive prenatal diagnosis, to screen for monogenic disorders in the fetus. Using the latest technologies, including Next Generation Sequencing (NGS), PrenatalScreen® Prenatal Test screen 744 genes for mutations causing over 1.000 severe genetic disorders in the fetus. PrenatalScreen® Prenatal Test allows for a comprehensive care and enables patients to make more informed reproductive decisions. Offering PrenatalScreen® Prenatal Test to a patient during pregnancy allows her to gain more knowledge about the potential to pass along a condition to the fetus. Aim of the test PrenatalScreen® Prenatal Test analyses DNA extracted from fetal cells in the amniotic fluid, collected through amniocentesis, or in the chorionic villi through villocentesis (CVS). The aim of this diagnositc test is to assess severe genetic diseases in the fetus, including the most common diseases in the European population. Genes listed in Table 1 were selected according to the incidence in the population of the disease caused by mutations in such genes, the severity of the clinical phenotype at birth and the importance of the related pathogenetic picture, in accordance with the indications of the American College of Medical Genetics (ACMG)(Grody et al., Genet Med 2013:15:482–483). PrenatalScreen®: Indication for testing PrenatalScreen® Prenatal Test is intended for patients who meet any of the following criteria: • Personal/familial anamnesis of hereditary genetic diseases; • For expectant mothers wishing to reduce the risk of a genetic diseases in the fetus; • For natural or in vitro fertilization (IVF)-derived pregnancies: • For couples using heterologus IVF procedures (egg/sperm donors). -

Blueprint Genetics Comprehensive Skeletal Dysplasias and Disorders
Comprehensive Skeletal Dysplasias and Disorders Panel Test code: MA3301 Is a 251 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of disorders involving the skeletal system. About Comprehensive Skeletal Dysplasias and Disorders This panel covers a broad spectrum of skeletal disorders including common and rare skeletal dysplasias (eg. achondroplasia, COL2A1 related dysplasias, diastrophic dysplasia, various types of spondylo-metaphyseal dysplasias), various ciliopathies with skeletal involvement (eg. short rib-polydactylies, asphyxiating thoracic dysplasia dysplasias and Ellis-van Creveld syndrome), various subtypes of osteogenesis imperfecta, campomelic dysplasia, slender bone dysplasias, dysplasias with multiple joint dislocations, chondrodysplasia punctata group of disorders, neonatal osteosclerotic dysplasias, osteopetrosis and related disorders, abnormal mineralization group of disorders (eg hypopohosphatasia), osteolysis group of disorders, disorders with disorganized development of skeletal components, overgrowth syndromes with skeletal involvement, craniosynostosis syndromes, dysostoses with predominant craniofacial involvement, dysostoses with predominant vertebral involvement, patellar dysostoses, brachydactylies, some disorders with limb hypoplasia-reduction defects, ectrodactyly with and without other manifestations, polydactyly-syndactyly-triphalangism group of disorders, and disorders with defects in joint formation and synostoses. Availability 4 weeks Gene Set Description -

Sema4 Cardiac Information Sheet
CARDIAC NEXT-GENERATION SEQUENCING PANELS Mail: One Gustave L. Levy Place, Box 1497 1 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com 0 3 8 Mail: One Gustave L. Levy Place, Box 1497 2 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com Mail: One Gustave L. Levy Place, Box 1497 3 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com Mail: One Gustave L. Levy Place, Box 1497 4 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com TABLE OF CONTENTS GENETIC TESTING FOR INHERITED CARDIOVASCULAR CONDITIONS 6 GENETICS AND INDICATIONS 6 TESTING METHODS, SENSITIVITY, AND LIMITATIONS 7 TURNAROUND TIME 9 SPECIMEN AND SHIPPING REQUIREMENTS 9 CUSTOMER SERVICES AND GENETIC COUNSELING 10 THE COMPREHENSIVE CARDIOMYOPATHY PANEL 11 DILATED CARDIOMYOPATHY (DCM) SUBPANEL 23 ARRHYTHMOGENIC RIGHT VENTRICULAR CARDIOMYOPATHY (ARVC) SUBPANEL 28 HYPERTROPHIC CARDIOMYOPATHY (HCM) SUBPANEL 30 LEFT VENTRICULAR NON-COMPACTION CARDIOMYOPATHY (LVNC) SUBPANEL 33 THE COMPREHENSIVE ARRHYTHMIAS PANEL 35 BRUGADA SYNDROME (BRS) SUBPANEL 40 CATECHOLAMINERGIC POLYMORPHIC VENTRICULAR TACHYCARDIA (CPVT) SUBPANEL 42 LONG / SHORT QT SYNDROME (LQTS / SQTS) SUBPANEL 44 AORTOPATHIES PANEL 46 CONGENITAL HEART DISEASE (CHD) PANEL 49 FAMILIAL HYPERCHOLESTEROLEMIA (FH) PANEL 52 PULMONARY HYPERTENSION (PAH) PANEL 54 METABOLIC CARDIOMYOPATHY PANEL 55 NOONAN SPECTRUM DISORDERS PANEL 57 HEREDITARY HEMORRHAGIC TELANGIECTASIA PANEL 59 REFERENCES 60 DISCLAIMER 69 Mail: One Gustave L. -

The Phenotype/Genotype Relation and the Current QT
110 Heart 1997;78:1 10-116 REVIEW The phenotype/genotype relation and the current status of genetic screening in hypertrophic cardiomyopathy, Marfan syndrome, and the long QT syndrome J Burn, J Camm, M J Davies, L Peltonen, P J Schwartz, H Watkins Hypertrophic cardiomyopathy, Marfan syn- encode amino acids, but within the gene there drome, and the long QT syndrome are all are also non-functional sequences (introns). autosomal disorders inherited in a dominant The simplest single gene abnormality is a manner; affected individuals are heterozygous, point mutation in which one base pair is that is they have one normal and one mutant replaced by another. Because of the redun- copy of the gene but not all the gene carriers dancy in the genetic code, point mutations are symptomatic. This failure to express fully may be silent polymorphisms that do not the expected phenotype is traditionally known change the amino acid or they may be mis- as incomplete penetrance. sense mutations that change a single amino acid. Missense mutations can be regarded as analogous to simple spelling errors in one let- Vocabulary and technology ter of a word. For example "the fish is on the In the human genome (consisting of 22 pairs dish" becomes "the fish is on the fish". of autosomes and the X and Y chromosomes) Because each gene exists in a maternal and a there are between 50 000 and 100 000 indi- paternal copy the ultimate product of the gene vidual genes coding for a wide range of prod- is a combination of normal (wild type) and ucts including enzymes and structural abnormal (mutant type). -

Marfan Syndrome Precision Panel Overview Indications Clinical Utility
Marfan Syndrome Precision Panel Overview Marfan Syndrome (MFS) is a spectrum of disorders caused by a genetic defect of the connective tissue and it is inherited in an autosomal dominant pattern. Since the connective tissue is the tissue that helps body growth as well as serving as a scaffold for cells and organs, Marfan Syndrome is a pleiotropic syndrome affecting mainly musculoskeletal, cardiac and ocular systems. The most severe of these manifestations include aortic root dilation and dissection, which are responsible for early patient demise. Pregnancy is a time of increased cardiovascular risk for women with Marfan syndrome, so an early diagnosis is key in pregnancy management. The Igenomix Marfan Syndrome Precision Panel can be used to make an accurate and directed diagnosis as well as a differential diagnosis of connective tissue disorders due to their overlapping phenotypic features ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Marfan Syndrome Precision Panel is indicated for those patients with a clinical suspicion or diagnosis with or without the following manifestations: - Subluxation of lenses - Cardiovascular findings: mitral valve prolapse, aortic regurgitation, mitral regurgitation, aortic dilation, dissection or aneurysm - Tall and thin stature - Long fingers and toes - Pectus carinatum or excavatum - Scoliosis - Hypermobile joints - Severe hindfoot valgus Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. Understanding global and molecular functions of fibrillin containing microfibrils for the development of a comprehensive theory of pathogenesis. -

Marfan Syndrome
Marfan Syndrome Marfan syndrome (MFS) is a connective tissue disorder that exhibits a high degree of clinical variability. Clinical symptoms typically involve the cardiovascular, ocular, and skeletal systems. Early diagnosis is crucial for treatment of skeletal, orthopedic, and Tests to Consider cardiovascular abnormalities. The diagnosis of MFS can be made or suspected based on established clinical criteria (see below). MFS is caused by pathogenic variants in the FBN1 Marfan Syndrome (FBN1) Sequencing and gene; however, there is signicant overlap of the clinical features with syndromes caused by Deletion/Duplication 2005584 pathogenic variants in other genes. Method: Polymerase Chain Reaction/Sequencing/Multiplex Ligation-dependent Probe Amplication Preferred test to conrm diagnosis when MFS is Disease Overview strongly suspected by consensus criteria Marfan Syndrome, FBN1 Sequencing Prevalence 2005589 Method: Polymerase Chain Reaction/Sequencing 1/5,000-10,000 Acceptable test to conrm diagnosis for individuals with clinical phenotype of MFS Symptoms Related Tests A clinical diagnosis of MFS in an individual without a family history of MFS (when Shprintzen-Goldberg syndrome [SGS], Loeys-Dietz syndrome [LDS], and Ehlers-Danlos Aortopathy Panel, Sequencing and Deletion/Duplication 2006540 syndrome type IV [EDS IV] have been excluded) is based on the presence of any of the Method: Massively Parallel Sequencing/Exonic following: Oligonucleotide-based CGH Microarray Aortic root dilatation or dissection and ectopia lentis Aortic root dilatation -

Whole Exome Sequencing Gene Package Skeletal Dysplasia, Version 2.1, 31-1-2020
Whole Exome Sequencing Gene package Skeletal Dysplasia, Version 2.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCC9 Atrial fibrillation, familial, 12, 614050 601439 65 100 100 95 Cardiomyopathy, dilated, 1O, 608569 Hypertrichotic osteochondrodysplasia, 239850 ACAN Short stature and advanced bone age, with or without early-onset osteoarthritis -
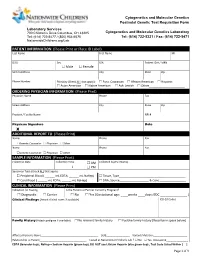
PATIENT INFORMATION (Please Print Or Place ID Label) Last Name First Name MI
Cytogenetics and Molecular Genetics Postnatal Genetic Test Requisition Form Laboratory Services 700 Children’s Drive Columbus, OH 43205 Cytogenetics and Molecular Genetics Laboratory Tel: (614) 722-5477 / (800) 934-6575 Tel: (614) 722-5321 / Fax: (614) 722-5471 NationwideChildrens.org/Lab PATIENT INFORMATION (Please Print or Place ID Label) Last Name First Name MI DOB Sex SSN Patient ID # / MRN Male Female Street Address City State Zip Phone Number Ethnicity (Check ALL that apply): Euro. Caucasian African American Hispanic Asian American Native American Ash. Jewish Other______________________ ORDERING PHYSICIAN INFORMATION (Please Print) Physician Name Phone Fax Street Address City State Zip Practice / Facility Name NPI # Physican Signature Date X ADDITIONAL REPORT TO (Please Print) Name Phone Fax Genetic Counselor Physician Other Name Phone Fax Genetic Counselor Physician Other SAMPLE INFORMATION (Please Print) Collection Date Collection Time AM Collected by (Full Name) : PM Specimen Type (Check ALL that apply): Peripheral Blood ( ______ mL EDTA; ______ mL NaHep) Tissue, Type_________________________________________ Cord Blood ( ______ mL EDTA; ______ mL NaHep) DNA, Source__________________ & Conc.________________ CLINICAL INFORMATION (Please Print) Indication for Testing Is the Patient or Partner Currently Pregnant? Diagnostic Carrier No Yes (Gestational age: ____weeks ____days; EDC _______________ ) Clinical Findings (Attach clinical notes if available) ICD-10 Codes Family History (Attach pedigree if available) -

Mass Phenotype
MASS PHENOTYPE MASS Phenotype is a connective tissue disorder that is similar to Marfan syndrome in that people with the condition have the similar Mitral valve, Aorta, Skin, and Skeletal features. People with MASS phenotype do not have lens dislocation and do not show progressive and dangerous aortic root enlargement, hallmark features of Marfan syndrome. MASS phenotype is similar to Marfan syndrome, but does not have dangerous aortic root enlargement. What other names do people use for MASS phenotype? MASS phenotype is also known as MASS syndrome. How prevalent is MASS phenotype? There aren’t any good estimates regarding the prevalence of MASS phenotype. What are the characteristics of MASS phenotype? The features of MASS phenotype are: • Mitral valve prolapse (MVP), a condition in which the mitral valve of the heart closes properly, but then flops backward, which allows blood to leak into the chamber from which it came instead of moving forward. This leaking is called regurgitation • Aortic root diameter may be at the upper limits of normal for the person’s body size, but it does not worsen over time. In addition, it does not increase the risk of aortic dissection. MARFAN.ORG | 800-8-MARFAN EXT. 126 | [email protected] MASS PHENOTYPE page 2 • Skin stretch marks unrelated to weight change (striae). • Skeletal (bone and joint) features of Marfan syndrome (including scoliosis, chest wall deformities , and joint hypermobility). What causes MASS phenotype? MASS phenotype can be caused by a change in the FBN1 (fibrillin-1) gene, the same gene that causes Marfan syndrome. It can be inherited within families (passed down through generations). -

Étude Rétrospective Portant Sur 4 Ans De Diagnostic Moléculaire Dans Le Cadre De Syndromes D’Origine Génétique Avec Vieillissement Prématuré Maude Grelet
Étude rétrospective portant sur 4 ans de diagnostic moléculaire dans le cadre de syndromes d’origine génétique avec vieillissement prématuré Maude Grelet To cite this version: Maude Grelet. Étude rétrospective portant sur 4 ans de diagnostic moléculaire dans le cadre de syn- dromes d’origine génétique avec vieillissement prématuré. Sciences du Vivant [q-bio]. 2019. dumas- 02359875 HAL Id: dumas-02359875 https://dumas.ccsd.cnrs.fr/dumas-02359875 Submitted on 12 Nov 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Etude rétrospective portant sur 4 ans de diagnostic moléculaire dans le cadre de syndromes d'origine génétique avec vieillissement prématuré T H È S E A R T I C L E Présentée et publiquement soutenue devant LA FACULTÉ DES SCIENCES MEDICALES ET PARAMEDICALES DE MARSEILLE Le 7 Juin 2019 Par Madame Maude GRELET Née le 3 janvier 1989 à Angers (49) Pour obtenir le grade de Docteur en Médecine D.E.S. de GÉNÉTIQUE MÉDICALE, CLINIQUE, CHROMOSOMIQUE ET MOLÉCULAIRE Membres du Jury de la Thèse : Monsieur le Professeur LEVY Nicolas Président Madame -

Skeletal Dysplasia Panel Versie V1 (345 Genen) Centrum Voor Medische Genetica Gent
H9.1-OP2-B40: Genpanel Skeletal dysplasia, V1, in voege op 14/02/2020 Skeletal_dysplasia panel versie V1 (345 genen) Centrum voor Medische Genetica Gent Associated phenotype, OMIM phenotype ID, phenotype Gene OMIM gene ID mapping key and inheritance pattern Atrial fibrillation, familial, 12, 614050 (3), Autosomal dominant; ABCC9 601439 Cardiomyopathy, dilated, 1O, 608569 (3); Hypertrichotic osteochondrodysplasia, 239850 (3), Autosomal dominant Congenital heart defects and skeletal malformations syndrome, 617602 (3), Autosomal dominant; Leukemia, Philadelphia ABL1 189980 chromosome-positive, resistant to imatinib, 608232 (3), Somatic mutation Short stature and advanced bone age, with or without early-onset osteoarthritis and/or osteochondritis dissecans, 165800 (3), ACAN 155760 Autosomal dominant; Spondyloepimetaphyseal dysplasia, aggrecan type, 612813 (3), Autosomal recessive; ?Spondyloepiphyseal dysplasia, Kimberley type, 608361 (3), Autosomal dominant Spondyloenchondrodysplasia with immune dysregulation, 607944 ACP5 171640 (3), Autosomal recessive Fibrodysplasia ossificans progressiva, 135100 (3), Autosomal ACVR1 102576 dominant Weill-Marchesani syndrome 1, recessive, 277600 (3), Autosomal ADAMTS10 608990 recessive Weill-Marchesani 4 syndrome, recessive, 613195 (3), Autosomal ADAMTS17 607511 recessive ADAMTSL2 612277 Geleophysic dysplasia 1, 231050 (3), Autosomal recessive AFF4 604417 CHOPS syndrome, 616368 (3), Autosomal dominant AGA 613228 Aspartylglucosaminuria, 208400 (3), Autosomal recessive Rhizomelic chondrodysplasia punctata,