New Ostomy Patient Guide 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Continent Urostomy Guide
$POUJOFOU6SPTUPNZ(VJEF "QVCMJDBUJPOPGUIF6OJUFE0TUPNZ"TTPDJBUJPOTPG"NFSJDB *OD i4FJ[FUIF 0QQPSUVOJUZw CONTINENT UROSTOMY GUIDE Ilene Fleischer, MSN, RN, CWOCN, Author Patti Wise, BSN, RN, CWOCN, Author Reviewed by: Authors and Victoria A.Weaver, RN, MSN, CETN Revised 2009 by Barbara J. Hocevar, BSN,RN,CWOCN, Manager, ET/WOC Nursing, Cleveland Clinic © 1985 Ilene Fleischer and Patti Wise This guidebook is available for free, in electronic form, from United Ostomy Associations of America (UOAA). UOAA may be contacted at: www.ostomy.org • [email protected] • 800-826-0826 CONTENTS INTRODUCTION . 3 WHAT IS A CONTINENT UROSTOMY? . 4 THE URINARY TRACT . 4 BEFORE THE SURGERY . .5 THE SURGERY . .5 THE STOMA . 7 AFTER THE SURGERY . 7 Irrigation of the catheter(s) 8 Care of the drainage receptacles 9 Care of the stoma 9 Other important information 10 ROUTINE CARE AT HOME . 10 Catheterization schedule 11 How to catheterize your pouch 11 Special considerations when catheterizing 11 Care of the catheter 12 Other routine care 12 HELPFUL HINTS . .13 SUPPLIES FOR YOUR CONTINENT UROSTOMY . 14 LIFE WITH YOUR CONTINENT UROSTOMY . 15 Clothing 15 Diet 15 Activity and exercise 15 Work 16 Travel 16 Telling others 17 Social relationships 17 Sexual relations and intimacy 17 RESOURCES . .19 GLOSSARY OF TERMS . 20 BIBLIOGRAPHY . .21 1 INTRODUCTION Many people have ostomies and lead full and active lives. Ostomy surgery is the main treatment for bypassing or replacing intestinal or urinary organs that have become diseased or dysfunctional. “Ostomy” means opening. It refers to a number of ways that bodily wastes are re-routed from your body. A urostomy specifi cally redirects urine. -
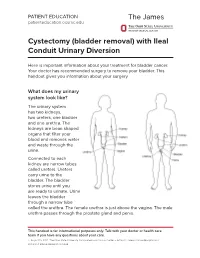
Cystectomy (Bladder Removal) with Ileal Conduit Urinary Diversion
PATIENT EDUCATION patienteducation.osumc.edu Cystectomy (bladder removal) with Ileal Conduit Urinary Diversion Here is important information about your treatment for bladder cancer. Your doctor has recommended surgery to remove your bladder. This handout gives you information about your surgery. What does my urinary system look like? The urinary system has two kidneys, two ureters, one bladder and one urethra. The kidneys are bean shaped organs that filter your blood and removes water and waste through the urine. Connected to each kidney are narrow tubes called ureters. Ureters carry urine to the bladder. The bladder stores urine until you are ready to urinate. Urine leaves the bladder through a narrow tube called the urethra. The female urethra is just above the vagina. The male urethra passes through the prostate gland and penis. This handout is for informational purposes only. Talk with your doctor or health care team if you have any questions about your care. © August 19, 2021. The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. Cystectomy (bladder removal) with Ileal Conduit Urinary Diversion A cystectomy is surgery to remove the bladder. In men, the prostate, seminal vesicles and lymph nodes may also be removed. In women, the ovaries, fallopian tubes, uterus, cervix, vagina, urethra and lymph nodes may be removed. Your doctor will talk with you about the surgery and what is best for you. After the bladder is removed, your doctor will make a new urinary system. One option is an ileal conduit, also called a urostomy. This will direct your urine to drain through a small opening in your abdomen (belly) called a “stoma”. -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -

Strategic Approach for Prioritising Local and Regional Sanitation Interventions for Reducing Global Antibiotic Resistance
water Article Strategic Approach for Prioritising Local and Regional Sanitation Interventions for Reducing Global Antibiotic Resistance David W. Graham *, Myra J. Giesen and Joshua T. Bunce School of Engineering, Newcastle University, Newcastle upon Tyne NE1 7RU, UK; [email protected] (M.J.G.); [email protected] (J.T.B.) * Correspondence: [email protected]; Tel.: +44-191-208-7930 Received: 23 November 2018; Accepted: 18 December 2018; Published: 24 December 2018 Abstract: Globally increasing antibiotic resistance (AR) will only be reversed through a suite of multidisciplinary actions (One Health), including more prudent antibiotic use and improved sanitation on international scales. Relative to sanitation, advanced technologies exist that reduce AR in waste releases, but such technologies are expensive, and a strategic approach is needed to prioritize more affordable mitigation options, especially for Low- and Middle-Income Countries (LMICs). Such an approach is proposed here, which overlays the incremental cost of different sanitation options and their relative benefit in reducing AR, ultimately suggesting the “next-most-economic” options for different locations. When considering AR gene fate versus intervention costs, reducing open defecation (OD) and increasing decentralized secondary wastewater treatment, with condominial sewers, will probably have the greatest impact on reducing AR, for the least expense. However, the best option for a given country depends on the existing sewerage infrastructure. Using Southeast Asia as a case study and World Bank/WHO/UNICEF data, the approach suggests that Cambodia and East Timor should target reducing OD as a national priority. In contrast, increasing decentralized secondary treatment is well suited to Thailand, Vietnam and rural Malaysia. -
Jessica Grossman an Advocacy and Awareness Pioneer
Summer/June 2016 $9.95 Jessica Grossman An advocacy and awareness pioneer Publisher Ian Settlemire [email protected] 800-750-9311 Summer/June 2016 • Volume 11, Issue 3 FAX 678-960-1231 P.O. Box 3605 Mission Viejo, CA 92690 Medical Advisors Jessica Grossman David Beck, MD Janice Rafferty, MD Catching up with an advocacy Joseph Basler, MD and awareness pioneer © The Phoenix 2016 (USPS page 42 024-352) is the official publication of the United Ostomy Associations of America, Inc. and published quar- Photograph by Angela McConnell© terly (March, June, Sept. and Dec.) by Ian Settlemire. To subscribe: $29.95 (one year U.S.) $49.95 (two years U.S.) 48 – Ordering Supplies www.phoenixuoaa.org Taking the guesswork out of this essential routine 1-800-750-9311 By Cliff Kalibjian The Phoenix P.O. Box 3605 52 – Local Leaders Mission Viejo, CA, 92690 Aiming a spotlight on three support group leaders No part of this publication may be By Charles Redner reproduced without the prior written permission of the publisher. Printed in the U.S.A. Opinions expressed by authors are their own and not necessarily 55 – Kindred Spirits those of the United Ostomy Associations of America Inc., the publisher, the edito- Finding more than expected at a support groupp rial consultants or advisors. The publisher makes no representa- By Charles Redner tion concerning the accuracy or truth of any matter or statement in any advertise- ment contained herein and disclaims all liability relating thereto. Advertising rates 56 – Continent Urinary Diversions and requirements sent on request. The Phoenix Magazine welcomes unsolicited editorial materials including Living with this procedure stories, new product releases, comments, photos, letters, etc. -

Complications of Urinary Diversion
Complications of Urinary Diversion Jennifer L. Dodson, M.D. Department of Urology Johns Hopkins University Types of Diversion Conduit Diversions Ileal conduit Colon conduit Continent Diversions Continent catheterizable reservoir Continent rectal pouch 1 Overview of Complications Mechanical Stoma problems Bowel obstruction Ureteral obstruction Reservoir perforation Metabolic Altered absorption Altered bone metabolism Growth delay Stones Cancer Conduit Diversions Ileal Conduit: Technically simplest Segment of choice Colon Conduit: Transverse or sigmoid Used when ileum not appropriate (eg: concomitant colon resection, abdominal radiation, short bowel syndrome, IBD) Early complications (< 30 days): 20-56% Late complications : 28-81% Risks: abdominal radiation abdominal surgery poor nutrition chronic steroids Farnham & Cookson, World J Urol, 2004 2 Complications of Ileal Conduit Campbell’s Urology, 8th Edition, 2002 Conduit: Bowel Complications Paralytic ileus 18-20% Conservative management vs NGT Consider TPN Bowel obstruction 5-10% Causes: Adhesions, internal hernia Evaluation: CT scan, Upper GI series Anastomotic leak 1-5 % Risk factors: bowel ischemia, radiation, steroids, IBD, technical error Prevention: Pre-operative bowel prep Attention to technical detail Stapled small-bowel Anastomosis (Campbell’s Blood supply, tension-free anastomosis, Urology, 8th Ed, 2004) realignment of mesentery Farnham & Cookson, World J Urol, 2004 3 Conduit Complications Conduit necrosis: Acute ischemia to bowel -
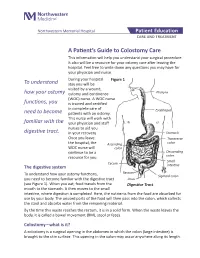
A Patient's Guide to Colostomy Care
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -

42 CFR Ch. IV (10–1–12 Edition) § 410.35
§ 410.35 42 CFR Ch. IV (10–1–12 Edition) the last screening mammography was (1) Colorectal cancer screening tests performed. means any of the following procedures furnished to an individual for the pur- [59 FR 49833, Sept. 30, 1994, as amended at 60 FR 14224, Mar. 16, 1995; 60 FR 63176, Dec. 8, pose of early detection of colorectal 1995; 62 FR 59100, Oct. 31, 1997; 63 FR 4596, cancer: Jan. 30, 1998] (i) Screening fecal-occult blood tests. (ii) Screening flexible § 410.35 X-ray therapy and other radi- sigmoidoscopies. ation therapy services: Scope. (iii) In the case of an individual at Medicare Part B pays for X-ray ther- high risk for colorectal cancer, screen- apy and other radiation therapy serv- ing colonoscopies. ices, including radium therapy and ra- (iv) Screening barium enemas. dioactive isotope therapy, and mate- (v) Other tests or procedures estab- rials and the services of technicians ad- lished by a national coverage deter- ministering the treatment. mination, and modifications to tests [51 FR 41339, Nov. 14, 1986. Redesignated at 55 under this paragraph, with such fre- FR 53522, Dec. 31, 1990] quency and payment limits as CMS de- termines appropriate, in consultation § 410.36 Medical supplies, appliances, with appropriate organizations and devices: Scope. (2) Screening fecal-occult blood test (a) Medicare Part B pays for the fol- means— lowing medical supplies, appliances (i) A guaiac-based test for peroxidase and devices: activity, testing two samples from (1) Surgical dressings, and splints, each of three consecutive stools, or, casts, and other devices used for reduc- (ii) Other tests as determined by the tion of fractures and dislocations. -

Double Barrel Wet Colostomy for Urinary and Fecal Diversion
Open Access Clinical Image J Urol Nephrol November 2017 Vol.:4, Issue:2 © All rights are reserved by Kang,et al. Journal of Double Barrel Wet Colostomy for Urology & Urinary and Fecal Diversion Nephrology Yu-Hao Xue and Chih-Hsiung Kang* Keywords: Double barrel wet colostomy; Urinary diversion; Fecal Department of Urology, Chang Gung Memorial Hospital-Kaohsiung diversion Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan, Republic of China Abstract Address for Correspondence A 60-year-old male who had a history of spinal cord injury received Chih-Hsiung Kang, Department of Urology, Chang Gung Memorial loop colostomy for fecal diversion and cystostomy for urinary diversion. Hospital - Kaohsiung Medical Center, Chang Gung University College Because he was diagnosed with muscle invasive bladder cancer, of Medicine, Taiwan, E- mail: [email protected] radical cystectomy and double barrel wet colostomy was conducted. Submission: 30 October, 2017 Computed tomography showed simultaneous urinary and fecal Accepted: 06 November, 2017 diversion and stone formation in the distal segment of colon conduit Published: 10 November, 2017 with urinary diversion. Copyright: © 2017 Kang CH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, Introduction provided the original work is properly cited. In patients with an advanced primary or recurrent carcinoma, double-barreled wet colostomy can be used for pelvic exenteration Bilateral hydroureters and mild hydronephrosis were noted and and urinary tract reconstruction. It is a technique that separate we suspected the calculi impacted in bilateral ureteto-colostomy urinary and fecal diversion with a single abdominal stoma. -

EAU Guidelines on Bladder Stones 2019
EAU Guidelines on Bladder Stones C. Türk (Chair), A. Skolarikos (Vice-chair), J.F. Donaldson, A. Neisius, A. Petrik, C. Seitz, K. Thomas Guidelines Associate: Y. Ruhayel © European Association of Urology 2019 TABLE OF CONTENTS PAGE 1. INTRODUCTION 3 1.1 Aims and Scope 3 1.2 Panel Composition 3 1.3 Available Publications 3 1.4 Publication History and Summary of Changes 3 1.4.1 Publication History 3 2. METHODS 3 2.1 Data Identification 3 2.2 Review 4 3. GUIDELINES 4 3.1 Prevalence, aetiology and risk factors 4 3.2 Diagnostic evaluation 4 3.2.1 Diagnostic investigations 5 3.3 Disease Management 5 3.3.1 Conservative treatment and Indications for active stone removal 5 3.3.2 Medical management of bladder stones 5 3.3.3 Bladder stone interventions 5 3.3.3.1 Suprapubic cystolithotomy 5 3.3.3.2 Transurethral cystolithotripsy 5 3.3.3.2.1 Transurethral cystolithotripsy in adults: 5 3.3.3.2.2 Transurethral cystolithotripsy in children: 6 3.3.3.3 Percutaneous cystolithotripsy 6 3.3.3.3.1 Percutaneous cystolithotripsy in adults: 6 3.3.3.3.2 Percutaneous cystolithotripsy in children: 6 3.3.3.4 Extracorporeal shock wave lithotripsy (SWL) 6 3.3.3.4.1 SWL in Adults 6 3.3.3.4.2 SWL in Children 6 3.3.4 Treatment for bladder stones secondary to bladder outlet obstruction (BOO) in adult men 7 3.3.5 Urinary tract reconstructions and special situations 7 3.3.5.1 Neurogenic bladder 7 3.3.5.2 Bladder augmentation 7 3.3.5.3 Urinary diversions 7 4. -

Bangor University MASTERS by RESEARCH Born to Throw, Climb
Bangor University MASTERS BY RESEARCH Born to throw, climb, squat AND run. Biomechanical evolution within the human lineage and its inference for health and fitness Gurnett, Scott Award date: 2020 Awarding institution: Bangor University Link to publication General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal ? Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 10. Oct. 2021 Born to throw, climb, squat AND run. Biomechanical evolution within the human lineage and its inference for health and fitness Masters by research thesis- Bangor University Candidate: Scott Gurnett Project supervisor: Dr Isabelle Winder Author’s declaration I hereby declare that this thesis is the results of my own investigations, except where otherwise stated. All other sources are acknowledged by bibliographic references. This work has not previously been accepted in substance for any degree and is not being concurrently submitted in candidature for any degree unless, as agreed by the University, for approved dual awards. -
Urinary Sample Collection Methods in Ileal Conduit Urinary Diversion Patients a Randomized Control Trial Markku H
Ostomy Care Ostomy Care J Wound Ostomy Continence Nurs. 2018;45(1):59-62. Published by Lippincott Williams & Wilkins Urinary Sample Collection Methods in Ileal Conduit Urinary Diversion Patients A Randomized Control Trial Markku H. Vaarala ABSTRACT PURPOSE: The purpose of this study was to compare bacteriological urinalysis findings using 3 urinary sample collection methods (clean stoma catheterization, urine dripping from the stoma, urine collected from the clean urostomy pouch) in ileal conduit urinary diversion patients. DESIGN: Randomized controlled trial. SAMPLE AND SETTING: Twenty-seven patients with ileal conduit urinary diversion from an outpatient urology clinic were enrolled; 9 patients were seen twice, for a total of 36 subjects and comparisons. METHODS: Data were collected during a clinic visit by a trained research nurse. Patients were randomized into 2 groups: group A had the first urine sample collected by clean stoma catheterization, followed by sample collection by urine dripping from the stoma; group B had the first urine sample collection by urine dripping from the stoma, followed by sample collected by clean stoma catheterization. All patients had a third urine sample collected from a factory-clean urostomy pouch. Bacteriological urinalysis findings were compared among methods. Descriptive analyses were summarized using mean, percentage, and frequency. The mean ages of the patients between the groups were compared with the t test. Other between-group comparisons were performed using the Fisher exact test. Urinary culture finding differences among the same patients were evaluated using the McNemar test. Sensitivity and specificity of the different urine sample collection methods were calculated assuming urine sample collection by catheterization as a reference method.