One Vision2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Whole Exome Sequencing Gene Package Vision Disorders, Version 6.1, 31-1-2020
Whole Exome Sequencing Gene package Vision disorders, version 6.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x ABCA4 Cone-rod dystrophy 3, 604116 601691 94 100 100 97 Fundus flavimaculatus, 248200 {Macular degeneration, age-related, 2}, 153800 Retinal dystrophy, early-onset severe, 248200 Retinitis pigmentosa 19, 601718 Stargardt disease -

Ophthalmology
Ophthalmology Information for health professionals MEDICAL GENETIC TESTING FOR OPHTHALMOLOGY Recent technologies, in particularly Next Generation Sequencing (NGS), allows fast, accurate and valuable diagnostic tests. For Ophthalmology, CGC Genetics has an extensive list of medical genetic tests with clinical integration of results by our Medical Geneticists. 1. EXOME SEQUENCING: Exome Sequencing is a very efficient strategy to study most exons of a patient’s genome, unraveling mutations associated with specific disorders or phenotypes. With this diagnostic strategy, patients can be studied with a significantly reduced turnaround time and cost. CGC Genetics has available 2 options for Exome Sequencing: • Whole Exome Sequencing (WES), which analyzes the entire exome (about 20 000 genes); • Disease Exome by CGC Genetics, which analyzes about 6 000 clinically-relevant genes. Any of these can be performed in the index case or in a Trio. 2. NGS PANELS For NGS panels, several genes associated with the same phenotype are simultaneously sequenced. These panels provide increased diagnostic capability with a significantly reduced turnaround time and cost. CGC Genetics has several NGS panels for Ophthalmology that are constantly updated (www.cgcgenetics.com). Any gene studied in exome or NGS panel can also be individually sequenced and analyzed for deletion/duplication events. 3. EXPERTISE IN MEDICAL GENETICS CGC Genetics has Medical Geneticists specialized in genetic counseling for ophthalmological diseases who may advice in choosing the most appropriate -

Basement Membranes in Diseases Affecting the Eye, Kidney
Van Agtmael, T. and Bruckner-Tuderman, L. (2010) Basement membranes and human disease. Cell and Tissue Research, 339 (1). pp. 167-188. ISSN 0302-766X http://eprints.gla.ac.uk/35275/ Deposited on: 30 August 2010 Enlighten – Research publications by members of the University of Glasgow http://eprints.gla.ac.uk Basement membranes and human disease Tom van Agtmael§ and Leena Bruckner-Tuderman* § Faculty of Biomedical and Life Sciences, University of Glasgow, Glasgow, U.K. and * Dept. of Dermatology, University Medical Center Freiburg and Freiburg Institute for Advanced Studies, Freiburg, Germany Corresponding authors: Tom Van Agtmael Faculty of Biomedical and Life Sciences, Davidson Building, University of Glasgow, University Avenue, Glasgow UK, [email protected],. Leena Bruckner-Tuderman Department of Dermatology, University Medical Center Freiburg, Hauptstr. 7, 79104 Freiburg, Germany. E-mail: [email protected] Keywords: basement membrane, laminin, collagen, laminin, nidogen Abbreviations BM: basement membrane, NMJ neuromuscular junction, DEJ dermo epidermal junction, SJS Schwartz Jampel syndrome, DDSH Dyssegmental dysplasia silverman handmaker type, EB epidermolysis bullosa, GBM glomerular basement membrane 1 Abstract In 1990 the role of basement membranes in human disease was established by the identification of COL4A5 mutations in Alport’s syndrome. Since then the number of diseases caused by mutations in basement membrane components has steadily increased as has our understanding of the roles of basement membranes in organ development and function. However, many questions remain as to the molecular and cellular consequences of these mutations and how they lead to the observed disease phenotypes. Despite this, exciting progress has recently been made with potential treatment options for some of these so far incurable diseases. -

Inherited Connective Tissue Disorders of Collagens: Lessons from Targeted Mutagenesis
13 Inherited Connective Tissue Disorders of Collagens: Lessons from Targeted Mutagenesis Christelle Bonod-Bidaud and Florence Ruggiero Institut de Génomique Fonctionnelle de Lyon, ENS de Lyon, UMR CNRS 5242, University Lyon 1, France 1. Introduction The extracellular matrix (ECM) is the cell structural environment in tissues and organs. The ECM is a dynamic structure that it is constantly remodelled. It contributes to tissue integrity and mechanical properties. It is also essential for maintaining tissue homeostasis, morphogenesis and differentiation, which it does, through specific interactions with cells. The ECM is composed of a mixture of water and macromolecules classified into four main categories: collagens, proteoglycans, elastic proteins, and non-collagenous glycoproteins (also called adhesive glycoproteins). The nature, concentration and ratio of the different ECM components are all important factors in the regulation of the assembly of complex tissue-specific networks tuned to meet mechanical and biological requirements of tissues. Collagens form a superfamily of 28 trimeric proteins, distinguishable from the other ECM components by their particular abundance in tissues (collagens represent up to 80-90% of total proteins in skin, tendon and bones) and their capacity to self-assemble into supramolecular organized structures (the best known being the banded fibers). The collagen superfamily is highly complex and shows a remarkable diversity in structure, tissue distribution and function (Ricard-Blum and Ruggiero, 2005). The importance -

Blueprint Genetics Vitreoretinopathy Panel
Vitreoretinopathy Panel Test code: OP0701 Is a 24 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion / diagnosis of vitreoretinopathy. The genes on this panel are included in the Retinal Dystropy Panel. About Vitreoretinopathy Vitreoretinal diseases are characterised by the degeneration of the vitreous and retina of the eye. Several types of vitreoretinopathies exist giving rise to a spectrum of phenotypic presentations such as retinal detachment, optically empty vitreous, fibrillary condensation, cataract, and neovascularization. The condition includes familial exudative vitreoretinopathy, snowflake vitreoretinal degeneration, Norrie disease, Wagner syndrome, Stickler syndrome and Knobloch syndrome. The vitreoretinopathies may be inherited in an autosomal dominant, autosomal recessive, or X-linked manner. For instance, autosomal dominant familial exudative vitreoretinopathy (FEVR) is caused by mutations in FZD4; LRP5 has been associated with both autosomal dominant and recessive cases and NDP with X-linked FEVR. The clinical presentation and the disease course can be highly variable. The prevalence of FEVR is unknown, but it is a rare disorder. Availability 4 weeks Gene Set Description Genes in the Vitreoretinopathy Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ATOH7 Persistent hyperplastic primary vitreous, autosomal recessive AR 4 9 BEST1 Vitreoretinochoroidopathy, Microcornea, Rod-cone dystrophy, Posterior AD/AR 62 318 staphyloma, Bestrophinopathy, -
Knobloch Syndrome Associated with Polymicrogyria and Early Onset of Retinal Detachment: Two Case Reports Robert J
White et al. BMC Ophthalmology (2017) 17:214 DOI 10.1186/s12886-017-0615-z CASE REPORT Open Access Knobloch syndrome associated with Polymicrogyria and early onset of retinal detachment: two case reports Robert J. White, Yao Wang, Peter Tang and Sandra R. Montezuma* Abstract Background: Knobloch Syndrome (KS) is a rare congenital syndrome characterized by occipital skull defects and vitreoretinal degeneration. Retinal detachment (RD) often occurs at the end of the first decade of life or later. Aside from occipital skull defects, central nervous system abnormalities are uncommon. Case presentations: We report on two siblings with KS. The first, a seven month old male, presented with nystagmus and was found to have a serous RD and a tessellated retinal appearance. His sister had a history of multiple visual abnormalities and had a similar retinal appearance although no signs of RD, but retina staphylomas. Genetic testing performed on both siblings showed a mutation in COL18A1, diagnostic of KS. MRI of both siblings demonstrated polymicrogyria but did not show occipital defects. Conclusions: Although several families with KS have been described previously, our case is noteworthy for several reasons. The RD observed in our first patient occurred at an early age, and we find evidence of only one patient with KS who had an RD identified at an earlier age. The findings of polymicrogyria are not characteristic of KS, and we found only a few previous reports of this association. Additionally, we review potential treatment options for this condition. Keywords: Knobloch syndrome, COL18A1, Retinal detachment, Polymicrogyria, Case report Background including pachygyria, polymicrogyria and cerebellar Knobloch Syndrome (KS) is a rare autosomal recessive atrophy among other findings [2]. -
Test Requisition Form (Dna & Genetic Tests)
TEST REQUISITION FORM (DNA & GENETIC TESTS) INCLUDE THE FIRST 3 PAGES OF THIS FORM WITH SPECIMEN. Before sending specimens, please contact us for pre-authorization procedures. Samples received without billing pre-authorization cannot be processed. REPORTING INFORMATION ADDITIONAL REPORTS Ordering Physician or Genetic Counselor Copy of report should be sent to Name: Name: Email: Email: Institution: Fax: ( ) Address: City, State, Zip: Name: Phone: ( ) Email: Fax: ( ) Fax: ( ) PATIENT INFORMATION Patient's Last Name, First Name, MI Birthdate (mm/dd/yyyy) Gender M F Indication or reason for testing (check all that apply) Diagnosis Asymptomatic family member Confirm recorded mutation: High risk population (state Ancestry or Ethnic background below) Prenatal screening Ongoing pregnancy Other: Ancestry or Ethnic Background (check all that apply) Patient's country of origin Ethnic Background Hispanic Jewish Asian Middle-East Americas Europe Africa Australia Hospital or Clinic Patient ID Specimen ID Diagnosis (ICD9 codes) SPECIMEN INFORMATION (REQUIRED) Specimen Date/Time Collected Collected by (initial) Specimen Type (If other, please contact us before shipping) / / _____:_____ AM/PM Buccal Blood Other: Specimen may be submitted as whole blood or buccal epithelial cells (2 swabs / patient). Transport at room temperature. For other specimens and more details, see page labeled "Specimen Requirements". TESTS REQUESTED (Ask us to customize the requisition form for your practice) Test No. Test Name 1. Stat 2. Stat 3. Stat Test Names are found on the list at the end of this form. The tests will be performed in the order listed. Turnaround times are usually less than 5 weeks following receipt of specimen. Sequential panels of several large genes will take longer depending on which gene positive results are found. -

Collagen VI), Multiplexin (E.G
Essays in Biochemistry (2019) 63 297–312 https://doi.org/10.1042/EBC20180071 Review Article Basement membrane collagens and disease mechanisms Anna Gatseva1, Yuan Yan Sin1, Gaia Brezzo1,2 and Tom Van Agtmael1 1Institute of Cardiovascular and Medical Sciences, University of Glasgow, University Avenue, Glasgow G12 8QQ, United Kingdom; 2Centre for Discovery Brain Sciences, Medical Downloaded from https://portlandpress.com/essaysbiochem/article-pdf/63/3/297/844117/ebc-2018-0071c.pdf by University of Glasgow user on 14 October 2019 School, University of Edinburgh, Edinburgh EH16 4SB, United Kingdom Correspondence: Tom Van Agtmael ([email protected]) Basement membranes (BMs) are specialised extracellular matrix (ECM) structures and col- lagens are a key component required for BM function. While collagen IV is the major BM collagen, collagens VI, VII, XV, XVII and XVIII are also present. Mutations in these collagens cause rare multi-systemic diseases but these collagens have also been associated with major common diseases including stroke. Developing treatments for these conditions will require a collective effort to increase our fundamental understanding of the biology of these collagens and the mechanisms by which mutations therein cause disease. Novel insights into pathomolecular disease mechanisms and cellular responses to these mutations has been exploited to develop proof-of-concept treatment strategies in animal models. Com- bined, these studies have also highlighted the complexity of the disease mechanisms and the need to obtain a more complete understanding of these mechanisms. The identification of pathomolecular mechanisms of collagen mutations shared between different disorders represent an attractive prospect for treatments that may be effective across phenotypically distinct disorders. -

Three Cases of Molecularly Confirmed Knobloch Syndrome
Ophthalmic Genetics ISSN: 1381-6810 (Print) 1744-5094 (Online) Journal homepage: https://www.tandfonline.com/loi/iopg20 Three cases of molecularly confirmed Knobloch syndrome Irina Balikova, Nuri Serdal Sanak, Depasse Fanny, Guillaume Smits, Julie Soblet, Elfride de Baere & Monique Cordonnier To cite this article: Irina Balikova, Nuri Serdal Sanak, Depasse Fanny, Guillaume Smits, Julie Soblet, Elfride de Baere & Monique Cordonnier (2020) Three cases of molecularly confirmed Knobloch syndrome, Ophthalmic Genetics, 41:1, 83-87, DOI: 10.1080/13816810.2020.1737948 To link to this article: https://doi.org/10.1080/13816810.2020.1737948 © 2020 The Author(s). Published with license by Taylor & Francis Group, LLC. Published online: 17 Mar 2020. Submit your article to this journal Article views: 269 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=iopg20 OPHTHALMIC GENETICS 2020, VOL. 41, NO. 1, 83–87 https://doi.org/10.1080/13816810.2020.1737948 CASE REPORT Three cases of molecularly confirmed Knobloch syndrome Irina Balikovaa,b, Nuri Serdal Sanakc, Depasse Fannyd, Guillaume Smitse, Julie Soblete, Elfride de Baeref, and Monique Cordonnierc aDepartment of Ophthalmology, University Hospital Leuven, Leuven, Belgium; bDepartment of Ophthalmology, Children Hospital Queen Fabiola, Brussels, Belgium; cDepartment of Ophthalmology, University Hospital Erasme, Brussels, Belgium; dOphthalmology Service, University Hospital Charleroi, Charleroi, Belgium; eDepartment of Genetics, University Hospital Erasme, Brussels, Belgium; fCenter for Medical Genetics, University Hospital Ghent, Ghent, Belgium ABSTRACT ARTICLE HISTORY Background: Knobloch syndrome (OMIM 267750) is a rare autosomal recessive disorder due to genetic Received October 21, 2019 defects in the COL18A1 gene. -

Optical Coherence Tomography Imaging of the Vitreoretinal Interface in Type II Stickler Syndrome
Optical Coherence Tomography Imaging of the Vitreoretinal Interface in Type II Stickler Syndrome Abstract Stickler syndrome was previously characterized post-enucleation by incarcerated vitreous collagen within glial tissue of patients with retinal detachments.1 This study demonstrates similar vitreoretinal interfaces in vivo using OCT imaging of three siblings with Stickler Syndrome. I. Case History Patient A: 1. Demographics: 38 YOWM 2. Chief Complaint: None 3. Ocular, medical history: Type II Stickler Syndrome, diagnosed age 7 4. Medications: None 5. Other salient information: Mild myopia 6. Family History a. Six Retinal detachments and two flap tears among first-degree relatives b. Twelve Retinal detachments among second-degree relatives c. Fourteen Retinal detachments among third-degree relatives Patient B: 1. Demographics: 36 YOWM 2. Chief Complaint: None 3. Ocular, medical history: a. Type II Stickler Syndrome, diagnosed age 5 b. Flap tear OD, age 17, treated with retinopexy c. Flap tear OS, age 20, treated with retinopexy d. Vitreal tuft with photopsias OD, age 22, treated with retinopexy e. Central Serous Retinopathy OD, age 23, resolved 4. Medications: None 5. Other salient information: Mild myopia 6. Family History a. Six Retinal detachments among first-degree relatives b. Twelve Retinal detachments among second-degree relatives c. Fourteen Retinal detachments among third-degree relatives Patient C: 1. Demographics: 34 YOWF 2. Chief Complaint: None 3. Ocular, medical history: a. Type II Stickler Syndrome, diagnosed age 3 b. Congenital cataracts OU 4. Medications: None 5. Other salient information: Mild myopia and moderate astigmatism 6. Family History a. Six Retinal detachments and two flap tears among first-degree relatives b. -

MASARYKOVA UNIVERZITA Lékařská Fakulta
MASARYKOVA UNIVERZITA Léka řská fakulta Biologický ústav Sanatorium REPROMEDA Dizerta ční práce - přílohy Preimplanta ční genetická diagnostika chromozomálních abnormit a screening aneuploidií časných embryí v terapii sterilních a infertilních pár ů metodou fertilizace in vitro Vědní obor: Léka řská biologie 5103V023 Brno, 2009 MUDr. Kate řina Veselá SEZNAM P ŘÍLOH Příloha 1 Autosomální dominantní Mendelovsky d ědi čné choroby (4 strany) Příloha 2 Autosomální recesívní Mendelovsky d ědi čné choroby (8 stran) Příloha 3 X - vázané Mendelovsky d ědi čné choroby (2 strany) Sperm and embryo analysis in a carrier of supernumerary inv Příloha 4 (21 stran) dup(15) marker chromosome Hybridization of the 18 alpha–satellite probe to chromosome 1 Příloha 5 (4 strany) revealed in PGD Příloha 6 What next for preimplantation genetic screening? (3 strany) ESHRE PGD Consortium data collection VI: cycles from January Příloha 7 (4 strany) to December 2003 with pregnancy follow-up to October 2004 ESHRE PGD Consortium data collection V: Cycles from January Příloha 8 (19 stran) to December 2002 with pregnancy follow-up to October 2003 Příloha 9 Central data collection on PGD and screening (1 strana) Příloha 1 Autosomální dominantní Mendelovsky dědičné choroby (odkazuje na www.diseasesdatabase.com) 4-hydroxyphenylpyruvate hydroxylase deficiency Blue color blindness Acatalasia Blue rubber bleb nevus syndrome Achondroplasia Boomerang dysplasia Acro-dermato-ungual-lacrimal-tooth syndrome Branchio-oculo-facial syndrome Acrodysostosis syndrome Brugada syndrome Acrokerato-elastoidosis -
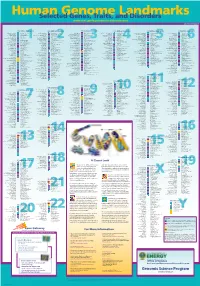
Genomeposter2009.Pdf
Fold HumanSelected Genome Genes, Traits, and Landmarks Disorders www.ornl.gov/hgmis/posters/chromosome genomics.energy.