Improving Clinical Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Sciences Alumni
Health Sciences Alumni Updated: 11/15/17 Allison Stickney 2018 High school science teaching Teach for America, Dallas-Fort Worth Sophia Sugar 2018 Research Assistant Nationwide Children’s Hosp., Columbus, OH Wanying Zhang 2017 Accelerated BSN, Nursing MGH Institute for Health Professions Kelly Ashnault 2017 Pharmacy Technician CVS Health Ian Grape 2017 Middle School Science Teacher Teach Kentucky Madeline Hobbs 2017 Medical Assistant Frederick Foot & Ankle, Urbana, MD Ryan Kennelly 2017 Physical Therapy Aide Professional Physical Therapy, Ridgewood, NJ Leah Pinckney 2017 Research Assistant UConn Health Keenan Siciliano 2017 Associate Lab Manager Medrobotics Corporation, Raynham, MA Ari Snaevarsson 2017 Nutrition Coach True Fitness & Nutrition, McLean VA Ellis Bloom 2017 Pre-medical fellowship Cumberland Valley Retina Consultants Elizabeth Broske 2017 AmeriCorps St. Bernard Project, New Orleans, LA Ben Crookshank 2017 Medical School Penn State College of Medicine Veronica Bridges 2017 Athletic Training UT Chattanooga, Texas A&M, Seton Hall Samantha Day 2017 Medical School University of Maryland School of Medicine Alexandra Fraley 2017 Epidemiology Research Assistant Department of Health and Human Services Genie Lavanant 2017 Athletic Training Seton Hall University Taylor Tims 2017 Nursing Drexel University, Johns Hopkins University Chase Stopyra 2017 Physical Therapy Rutgers School of Health Professions Madison Tulp 2017 Special education Teach for America Joe Vegso 2017 Nursing UPenn, Villanova University Nicholas DellaVecchia 2017 Physical -

Nominations Of: Ronald Sims, Fred P. Hochberg, Helen R
S. HRG. 111–173 NOMINATIONS OF: RONALD SIMS, FRED P. HOCHBERG, HELEN R. KANOVSKY, DAVID H. STEVENS, PETER KOVAR, JOHN D. TRASVIN˜A, AND DAVID S. COHEN HEARING BEFORE THE COMMITTEE ON BANKING, HOUSING, AND URBAN AFFAIRS UNITED STATES SENATE ONE HUNDRED ELEVENTH CONGRESS FIRST SESSION ON NOMINATIONS OF: RONALD SIMS, OF WASHINGTON, TO BE DEPUTY SECRETARY, DEPARTMENT OF HOUSING AND URBAN DEVELOPMENT FRED P. HOCHBERG, OF NEW YORK, TO BE PRESIDENT AND CHAIRMAN, EXPORT-IMPORT BANK HELEN R. KANOVSKY, OF MARYLAND, TO BE GENERAL COUNSEL, DEPARTMENT OF HOUSING AND URBAN DEVELOPMENT DAVID H. STEVENS, OF VIRGINIA, TO BE ASSISTANT SECRETARY FOR HOUSING–FEDERAL HOUSING COMMISSIONER, DEPARTMENT OF HOUSING AND URBAN DEVELOPMENT PETER KOVAR, OF MARYLAND, TO BE ASSISTANT SECRETARY FOR CONGRESSIONAL AND INTERGOVERNMENTAL AFFAIRS, DEPARTMENT OF HOUSING AND URBAN DEVELOPMENT JOHN D. TRASVIN˜ A, OF CALIFORNIA, TO BE ASSISTANT SECRETARY FOR FAIR HOUSING AND EQUAL OPPORTUNITY, DEPARTMENT OF HOUSING AND URBAN DEVELOPMENT DAVID S. COHEN, OF MARYLAND, TO BE ASSISTANT SECRETARY FOR TERRORIST FINANCING, DEPARTMENT OF THE TREASURY APRIL 23, 2009 Printed for the use of the Committee on Banking, Housing, and Urban Affairs ( Available at: http://www.access.gpo.gov/congress/senate/senate05sh.html U.S. GOVERNMENT PRINTING OFFICE 53–677 PDF WASHINGTON : 2009 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 COMMITTEE ON BANKING, HOUSING, AND URBAN AFFAIRS CHRISTOPHER J. DODD, Connecticut, Chairman TIM JOHNSON, South Dakota RICHARD C. -
Download on the AASL Website an Anonymous Funder Donated $170,000 Tee, and the Rainbow Round Table at Bit.Ly/AASL-Statements
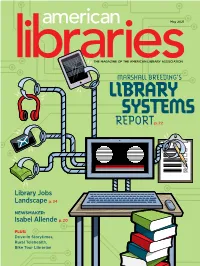
May 2021 THE MAGAZINE OF THE AMERICAN LIBRARY ASSOCIATION MARSHALL BREEDING’S LIBRARY SYSTEMS REPORTp. 22 Library Jobs Landscape p. 34 NEWSMAKER: Isabel Allende p. 20 PLUS: Drive-In Storytimes, Rural Telehealth, Bike Tour Librarian This Summer! Join us online at the event created and curated for the library community. Event Highlights • Educational programming • COVID-19 information for libraries • News You Can Use sessions highlighting • Interactive Discussion Groups new research and advances in libraries • Presidents' Programs • Memorable and inspiring featured authors • Livestreamed and on-demand sessions and celebrity speakers • Networking opportunities to share and The Library Marketplace with more than • connect with peers 250 exhibitors, Presentation Stages, Swag-A-Palooza, and more • Event content access for a full year ALA Members who have been recently furloughed, REGISTER TODAY laid o, or are experiencing a reduction of paid alaannual.org work hours are invited to register at no cost. #alaac21 Thank you to our Sponsors May 2021 American Libraries | Volume 52 #5 | ISSN 0002-9769 COVER STORY 2021 LIBRARY SYSTEMS REPORT Advancing library technologies in challenging times | p. 22 BY Marshall Breeding FEATURES 38 JOBS REPORT 34 The Library Employment Landscape Job seekers navigate uncertain terrain BY Anne Ford 38 The Virtual Job Hunt Here’s how to stand out, both as an applicant and an employer BY Claire Zulkey 42 Serving the Community at All Times Cultural inclusivity programming during a pandemic BY Nicanor Diaz, Virginia Vassar -

Dawn of a New Era
CHAPTER FOUR Dawn of a New Era hen Democrat Jim Himes (2009-present) announced that he Wwould challenge Chris Shays for the fourth congressional district, few analysts, including this author, believed Himes would have much of a chance against the more experienced and seasoned Republican maverick. Many predicted that the power of incumbency would likely prevail and that once again Shays would be returned to Congress. After all, Himes had neither name recognition nor the sort of political experience one would expect of a serious congressional candidate. Himes’s political experience was essentially limited to his service as board chairman of the Greenwich Housing Authority and a stint on the Greenwich Board of Finance. He also served as chairman on the board of Aspira of Connecticut, a Bridgeport-based organization that assists young Latinos with educational opportunities.1 Himes was not in any way a public figure, nor had he served in the Connecticut General Assembly. Yet despite a shallow political resume, Himes did bring to the table a very impressive set of professional credentials. He was a former vice president with the Wall Street investment firm Goldman Sachs. He therefore had considerable expertise regarding financial and economic policy. He left his career as a Wall Street executive to lead a non-profit organization that helped companies secure financing for affordable housing projects. He was thus very familiar with the interplay of housing and banking policy. He was a graduate of Harvard University and a former Rhodes Scholar. 64 DAWN OF A NEW ERA Born in Peru to American parents and having lived in Latin America for the first ten years of his life, Himes was fluent in Spanish. -

Bijan Rafiekian, Diane Farrell, William S
S. HRG. 110–924 NOMINATIONS OF: BIJAN RAFIEKIAN, DIANE FARRELL, WILLIAM S. JASIEN, MARK S. SHELTON, AND WILLIAM H. HEYMAN HEARING BEFORE THE COMMITTEE ON BANKING, HOUSING, AND URBAN AFFAIRS UNITED STATES SENATE ONE HUNDRED TENTH CONGRESS FIRST SESSION ON NOMINATIONS OF: BIJAN RAFIEKIAN, OF CALIFORNIA, TO BE A MEMBER OF THE BOARD OF DIRECTORS, EXPORT-IMPORT BANK DIANE FARRELL, OF CONNECTICUT, TO BE A MEMBER OF THE BOARD OF DIRECTORS, EXPORT-IMPORT BANK WILLIAM S. JASIEN, OF VIRGINIA, TO BE A DIRECTOR, SECURITIES INVESTOR PROTECTION CORPORATION MARK S. SHELTON, OF NEW JERSEY, TO BE A DIRECTOR, SECURITIES INVESTOR PROTECTION CORPORATION WILLIAM H. HEYMAN, OF NEW YORK, TO BE A DIRECTOR, SECURITIES INVESTOR PROTECTION CORPORATION WEDNESDAY, JULY 11, 2007 Printed for the use of the Committee on Banking, Housing, and Urban Affairs ( Available at: http://www.access.gpo.gov/congress/senate/senate05sh.html U.S. GOVERNMENT PRINTING OFFICE 50–323 WASHINGTON : 2009 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2104 Mail: Stop IDCC, Washington, DC 20402–0001 VerDate Nov 24 2008 01:13 Dec 18, 2009 Jkt 050323 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 E:\HR\OC\A323.XXX A323 tjames on DSKG8SOYB1PROD with HEARING COMMITTEE ON BANKING, HOUSING, AND URBAN AFFAIRS CHRISTOPHER J. DODD, Connecticut, Chairman TIM JOHNSON, South Dakota RICHARD C. SHELBY, Alabama JACK REED, Rhode Island ROBERT F. BENNETT, Utah CHARLES E. SCHUMER, New York WAYNE ALLARD, Colorado EVAN BAYH, Indiana MICHAEL B. -

Homeland Security: Keeping First Responders First
HOMELAND SECURITY: KEEPING FIRST RESPONDERS FIRST HEARING BEFORE THE SUBCOMMITTEE ON NATIONAL SECURITY, VETERANS AFFAIRS AND INTERNATIONAL RELATIONS OF THE COMMITTEE ON GOVERNMENT REFORM HOUSE OF REPRESENTATIVES ONE HUNDRED SEVENTH CONGRESS SECOND SESSION JULY 30, 2002 Serial No. 107–220 Printed for the use of the Committee on Government Reform ( Available via the World Wide Web: http://www.gpo.gov/congress/house http://www.house.gov/reform U.S. GOVERNMENT PRINTING OFFICE 87–386 PDF WASHINGTON : 2003 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512–1800; DC area (202) 512–1800 Fax: (202) 512–2250 Mail: Stop SSOP, Washington, DC 20402–0001 VerDate 11-MAY-2000 09:35 Jun 24, 2003 Jkt 000000 PO 00000 Frm 00001 Fmt 5011 Sfmt 5011 D:\DOCS\87386.TXT HGOVREF1 PsN: HGOVREF1 COMMITTEE ON GOVERNMENT REFORM DAN BURTON, Indiana, Chairman BENJAMIN A. GILMAN, New York HENRY A. WAXMAN, California CONSTANCE A. MORELLA, Maryland TOM LANTOS, California CHRISTOPHER SHAYS, Connecticut MAJOR R. OWENS, New York ILEANA ROS-LEHTINEN, Florida EDOLPHUS TOWNS, New York JOHN M. MCHUGH, New York PAUL E. KANJORSKI, Pennsylvania STEPHEN HORN, California PATSY T. MINK, Hawaii JOHN L. MICA, Florida CAROLYN B. MALONEY, New York THOMAS M. DAVIS, Virginia ELEANOR HOLMES NORTON, Washington, MARK E. SOUDER, Indiana DC STEVEN C. LATOURETTE, Ohio ELIJAH E. CUMMINGS, Maryland BOB BARR, Georgia DENNIS J. KUCINICH, Ohio DAN MILLER, Florida ROD R. BLAGOJEVICH, Illinois DOUG OSE, California DANNY K. DAVIS, Illinois RON LEWIS, Kentucky JOHN F. TIERNEY, Massachusetts JO ANN DAVIS, Virginia JIM TURNER, Texas TODD RUSSELL PLATTS, Pennsylvania THOMAS H. -

Congressional Elections: a Political Turning Point? Social Education Staff
Social Education 70(6), pp. 382–386 ©2006 National Council for the Social Studies Congressional Elections: A Political Turning Point? Social Education Staff The Democrats have their best chance in 10 years to when national issues are on everybody’s mind. During the summer, make major gains in the congressional elections on November the approval rating of President Bush ranged between 33% and 7, while Republicans are striving to retain control of both the 42% in the different opinion polls. One of the issues identified by House and the Senate. For Republicans to lose control of both Americans as especially important was the war in Iraq, closely houses of the legislature, the Democrats need net gains of 15 identified with Bush, which the majority of Americans believe House seats and 6 Senate seats. was a mistake to start. The elections are taking place against a backdrop of dimin- In general, when a president’s approval rating is below 50%, that ishing confidence in the performance of Congress. Corruption spells potential trouble for his party in congressional elections. scandals, pork barrel politics, perceptions that politicians are The fact that the U.S. economy has grown at a good pace too beholden to lobbies and political donors, and a widespread would normally be positive for an incumbent party. Despite public belief that the country is heading in the wrong direction, economic growth, however, most Americans do not seem combined to give Congress unusually high disapproval rat- to believe that the economy is heading in the right direc- ings in polls taken this summer. -

A District Represented by Mavericks
CHAPTER THREE A District Represented by Mavericks f there is one word that best describes those individuals who have Ibeen elected to the United States Congress from Connecticut’s fourth congressional district, that word, plain and simple, is “maverick.” Indeed, Lowell P. Weicker, Jr., who represented the fourth district prior to his election to the United States Senate, titled his autobiography “Maverick” to underscore his conduct and orientation during his years in public office.1 Political mavericks, however, have ruled the fourth district long before the appearance of the contentious Weicker. Clare Boothe Luce (1943-47) Clare Boothe Luce, who served in Congress from 1943-47, is perhaps the first representative from Connecticut’s fourth congressional district to deserve the maverick moniker. The fact that she was not only a woman but also a woman elected to Congress during World War II speaks volumes about the independence and resolve of this quite extraordinary individual. A woman elected to the U.S. House of Representatives at a time when so few women had even considered entering politics, and during a world war no less, is in itself quite remarkable. During Luce’s first term in Congress slightly less than two percent of House members were women, while during her second term slightly less than three percent of the House consisted of females. There were no women in A DISTRICT REPRESENTED BY MAVERICKS 37 the United States Senate during Luce’s two congressional terms.2 Prior to her election to Congress, Luce was a writer, accomplished and renowned playwright, journalist, and a widely traveled and astute foreign correspondent. -

Joel H. Rosenthal Curriculum Vitae
JOEL H. ROSENTHAL CURRICULUM VITAE Address: Carnegie Council for Ethics in International Affairs 170 East 64th Street New York, NY 10065 212-838-4120 [email protected] Web Page: www.joelrosenthal.org Personal Data: Born April 28, 1960; Brookline, MA Current Positions President, Carnegie Council for Ethics in International Affairs Editor-in-Chief, Ethics & International Affairs Adjunct Professor, Program in International Relations, Department of Politics, New York University Adjunct Professor and Chairman, Globalization and International Affairs Program, Bard College Education Yale University Ph.D. American Studies 1988 M. Phil. 1986, M.A. 1985 Harvard University B.A. History 1982 Fellowships and Prizes Dorsett Fellow, Dartmouth College 2016 Honorary Doctor of Social Science, University of Edinburgh 2013 Honorary Professor, University of Copenhagen 2010 - 2015 2 John Addison Porter Prize, Yale University 1988 For a work of scholarship presented “in such a literary form as to make the product of general human interest” Institute for the Study of World Politics, Washington, DC Dissertation Year Fellowship 1987-1988 Institute for the Study of World Politics, Washington, DC Dissertation Year Fellowship 1987-1988 John Harvard Scholarship 1979-1982 Awarded for academic achievement of the highest distinction Publications Books Righteous Realists: Political Realism, Responsible Power, and American Culture in the Nuclear Age (Baton Rouge: Louisiana State University Press, 1991) Edited Volumes Ethics & International Affairs: A Reader 3rd Edition (Georgetown University Press, 2009) with Christian Barry Ethics and International Relations (Library of Essays in International Relations Series, Ashgate Publishing, 2009) with Ethan B. Kapstein Ethics of Spying: A Reader for the Intelligence Professional Foreword, (The Scarecrow Press, Inc., January 2005) Political Theory and International Affairs: Hans J. -

Federal Election Commission Annual Report 2004
Federal Election Commission Annual Report 2004 Federal Election Commission Washington, DC 20463 Commissioners Scott E. Thomas, Chairman Michael E. Toner, Vice Chairman David M. Mason, Commissioner Danny L. McDonald, Commissioner Bradley A. Smith, Commissioner Ellen L. Weintraub, Commissioner Statutory Officers James A. Pehrkon, Staff Director Lawrence H. Norton, General Counsel Lynne A. McFarland, Inspector General The Annual Report is prepared by: Gregory J. Scott, Assistant Staff Director, Information Division Amy L. Kort, Ph.D., Senior Technical Writer, Information Division Michelle L. Ryan, Public Affairs Specialist Paul Clark, Ph.D., Statistician, Information Technology Division FEDERAL ELECTION COMMISSION WASHINGTON, D.C. 20463 OFFICE OF THE CHAIRMAN June 1, 2005 The President of the United States Members of The United States Senate Members of The United States House of Representatives Dear Mr. President, Senators and Representatives: We are pleased to submit for your information the 30th Annual Report of the Federal Elec- tion Commission, pursuant to 2 U.S.C. §438(a)(9). The Annual Report 2004 describes the activities performed by the Commission in the last calendar year. In 2004, the agency provided critical election-year guidance and oversight. During this Presidential election year, the Commission completed work on five rulemakings, issued 39 advisory opinions, signed 38 conciliation agreements, collected $2,674,745 in civil penalties for the U.S. Treasury and closed 12 litigation cases. At the same time, the agency efficiently received and made public volumes of financial data—including disclosure information required for the first time under the Bipartisan Campaign Reform Act of 2002--during an election year of unprecedented financial activity. -

Commencement 1971-1980
r / / .# . /X/^:^// fM ////// Digitized by the Internet Arciiive in 2012 with funding from LYRASIS IVIembers and Sloan Foundation http://archive.org/details/commencement1974 ORDER OF PROCESSION MARSHALS MARY D. AINSWORTH MATTHEW A. CRENSON HANS GOEDICKE GERALD S. GOTTERER ROBERT E. GREEN JOHN W. GRYDER WILLIAM H. HUGGINS ROBERT A. LYSTAD RICHARD A. MACKSEY PAUL R. OLSON EVERETT L. SCHILLER THE GRADUATES * MARSHALS CARL F. CHRIST FRANCIS E. ROURKE MEMBERS OF THE SOCIETY OF SCHOLARS THE DEANS OFFICERS OF THE UNIVERSITY THE TRUSTEES * MARSHALS MICHAEL BEER JOHN WALTON THE FACULTIES * CHIEF MARSHAL MAURICE MANDELBAUM THE CHAPLAINS NEWLY INDUCTED MEMBERS OF THE SOCIETY OF SCHOLARS PRESENTORS OF THE HONORARY DEGREE CANDIDATES AND THE HONORARY DEGREE CANDIDATES THE PROVOST OF THE UNIVERSITY PRESIDENT EMERITUS OF THE UNIVERSITY CHAIRMAN OF THE BOARD OF TRUSTEES THE PRESIDENT OF THE UNIVERSITY ORDER OF EVENTS STEVEN MULLER President of the University, presiding Hs Hf * PROCESSIONAL The audience is requested to stand as the Academic Procession moves into the area and to remain standing until after the Invocation Crown Imperial Sir William Walton The Peabody Wind Ensemble Richard Higgins, Director INVOCATION REV. CHESTER WICKWIRE Chaplain, The Johns Hopkins University sN " THE STAR-SPANGLED BANNER " * GREETINGS ROBERT D. H. HARVEY Chairman of the Board of Trustees PRESENTATION OF NEW MEMBERS OF THE SOCIETY OF SCHOLARS LYMAN C. CRAIG HELEN VAN VUNAKIS SCHOLARS PRESENTED BY HARRY WOOLF Provost of the University MUSICAL INTERLUDE The Peabody Wind Ensemble CONFERRING OF HONORARY DEGREES BENJAMIN M. BAKER FREDERIC C. LANE JOHN MERRILL OLIN RAFAEL HERNANDEZ-COLON * ADDRESS HIS EXCELLENCY RAFAEL HERnAnDEZ-COLON Governor of the Commonwealth of Puerto Rico CONFERRING OF DEGREES ON CANDIDATES BACHELORS OF ARTS BACHELORS OF ENGINEERING SCIENCE Presented by GEORGE E. -

September 2004 Record.Indd
September 2004 Federal Election Commission Volume 30, Number 9 Table of Contents Regulations Court Cases Regulations 1 Political Committee Rules Political Committee Rules Wisconsin Right to Life, Approved Approved Inc. v FEC 4 Rulemaking Petition On August 19, 2004, the Commis- On August 17, 2004, the U.S. sion approved final rules that may District Court for the District of Court Cases require more so-called 527 organiza- 1 Wisconsin Right to Life, Inc. v Columbia denied Wisconsin Right tions to register and report with the to Life, Inc.’s (WRTL) motion for FEC FEC, beginning in 2005. In general, 3 LaRouche’s Committee for a New a preliminary injunction that would Bretton Woods v FEC the new regulations: have exempted certain WRTL broad- 3 New Litigation • Expand the definition of contribu- cast ads from the ban on corporate tion to include funds received as funding of electioneering communi- 4 Nonfilers a result of a communication that cations. indicates any portion of those funds 4 Advisory Opinions Background will be used to support or oppose WRTL had filed suit in the U.S. Public Funding the election of a clearly identified federal candidate; and District Court for the District of 7 Public Funding for Kerry-Edwards Columbia on July 26, 2004, asking 8 Matching Fund Certifications • Define the types of costs that feder- al PACs may allocate between their the court to find the prohibition on the use of corporate funds to pay 8 Publications federal and nonfederal accounts, and modify the allocation methods for electioneering communications unconstitutional as applied to certain Administrative Fines they must use.