Fatty Acids and Risk of Prostate Cancer in a Nested Case-Control Study in Male Smokers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis
International Journal of Molecular Sciences Review Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis David Johane Machate 1, Priscila Silva Figueiredo 2 , Gabriela Marcelino 2 , Rita de Cássia Avellaneda Guimarães 2,*, Priscila Aiko Hiane 2 , Danielle Bogo 2, Verônica Assalin Zorgetto Pinheiro 2, Lincoln Carlos Silva de Oliveira 3 and Arnildo Pott 1 1 Graduate Program in Biotechnology and Biodiversity in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] (D.J.M.); [email protected] (A.P.) 2 Graduate Program in Health and Development in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; pri.fi[email protected] (P.S.F.); [email protected] (G.M.); [email protected] (P.A.H.); [email protected] (D.B.); [email protected] (V.A.Z.P.) 3 Chemistry Institute, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-67-3345-7416 Received: 9 March 2020; Accepted: 27 March 2020; Published: 8 June 2020 Abstract: Long-term high-fat dietary intake plays a crucial role in the composition of gut microbiota in animal models and human subjects, which affect directly short-chain fatty acid (SCFA) production and host health. This review aims to highlight the interplay of fatty acid (FA) intake and gut microbiota composition and its interaction with hosts in health promotion and obesity prevention and its related metabolic dysbiosis. -

Free Fatty Acids Are Associated with the Cognitive Functions in Stroke Survivors
International Journal of Environmental Research and Public Health Article Free Fatty Acids Are Associated with the Cognitive Functions in Stroke Survivors Dariusz Kotl˛ega 1,* , Barbara Peda 1, Joanna Palma 2 , Agnieszka Zembro ´n-Łacny 3 , Monika Goł ˛ab-Janowska 4, Marta Masztalewicz 4, Przemysław Nowacki 4 and Małgorzata Szczuko 2 1 Department of Neurology, District Hospital, 67-200 Glogow, Poland; [email protected] 2 Department of Human Nutrition and Metabolomics, Pomeranian Medical University, 71-460 Szczecin, Poland; [email protected] (J.P.); [email protected] (M.S.) 3 Department of Applied and Clinical Physiology, Collegium Medicum, University of Zielona Gora, 65-001 Zielona Góra, Poland; [email protected] 4 Department of Neurology, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] (M.G.-J.); [email protected] (M.M.); [email protected] (P.N.) * Correspondence: [email protected] Abstract: Ischemic stroke is a leading cause of motor impairment and psychosocial disability. Al- though free fatty acids (FFA) have been proven to affect the risk of stroke and potentially dementia, the evidence of their impact on cognitive functions in stroke patients is lacking. We aimed to establish such potential relationships. Seventy-two ischemic stroke patients were prospectively analysed. Their cognitive functions were assessed seven days post-stroke and six months later as follow-up (n = 41). Seven days post-stroke analysis of serum FFAs levels showed direct correlations between Citation: Kotl˛ega,D.; Peda, B.; Cognitive Verbal Learning Test (CVLT) and the following FFAs: C20:4n6 arachidonic acid and Palma, J.; Zembro´n-Łacny, A.; C20:5n3 eicosapentaenoic acid, while negative correlations were observed for C18:3n3 linolenic acid Goł ˛ab-Janowska,M.; Masztalewicz, (ALA), C18:4 n3 stearidonic acid and C23:0 tricosanoic acid. -

Control of Differentiation of a Mammary Cell Line by Lipids
Proc. Natl. Acad. Sci. USA Vol. 77, No. 3, pp. 1551-1555, March 1980 Cell Biology Control of differentiation of a mammary cell line by lipids (domes/tumor promoters/fatty acids/lysolecithins) RENATO DULBECCO*, MAURO BOLOGNAt, AND MICHAEL UNGER The Salk Institute, 10010 N. Torrey Pines Road, La Jolla, California 92037 Contributed by Renato Dulbecco, December 17, 1979 ABSTRACT A rat mammary cell line (LA7) undergoes profound effect on cultured cells of various types (13, 14). These spontaneous differentiation into domes due to production of effects include stimulation of growth (15), suppression of several specific inducers by the cells. Some of these inducers may be kinds of differentiation and induction of some other lipids, and we show that lipids regulate this differentiation as (16-24), both inducers and inhibitors. One inhibitor is the tumor pro- kinds of differentiation (25-27). TPA also induces a phenotype moter tetradecanoyl-13 phorbol 12-acetate. The inducers are similar to that of transformed cells (28-30), with a reduced saturated fatty acids of two groups: butyric acid and acids with contact inhibition of growth (31), increased production of chain lengths from C13 to C16, especially myristic acid (C14). plasminogen activator (32-35), increased phospholipid turnover Other inducers are myristoyl and palmitoyl lysolecithins, (36-38), decrease of LETS protein (39), and induction of myristic acid methyl ester, and two cationic detergents with a polyamine synthesis (40). TPA may alter the function of the cell tetradecenyl chain. We propose that the lipids with a C14-CI6 plasma membrane, as its alkyl chain affect differentiation by recognizing specific re- suggested by ability to inhibit the ceptors through their alkyl chains and that the effects obtained binding of epidermal growth factor to its receptors at the cell depend on the head groups. -
(L. 1758): on the Origin of Fatty Acids in Prepupae B
www.nature.com/scientificreports OPEN About lipid metabolism in Hermetia illucens (L. 1758): on the origin of fatty acids in prepupae B. Hoc1, M. Genva2, M.‑L. Fauconnier2, G. Lognay1, F. Francis1 & R. Caparros Megido1* Although increasingly targeted in animal nutrition, black soldier fy larvae or prepupae (BSF, Hermetia illucens L. 1758) require the characterization and modulation of their fatty acid profle to become fully integrated within the feed sector. This improvement will only be possible by the understanding of underlaying biochemical pathways of fatty acid synthesis in BSF. In this study, we hypothesized a labelling of de novo synthesized fatty acids in BSF by the incorporation of deuterated water (D2O) in their feed. Three batches of ffty larvae were reared on two diets with diferent polyunsaturated fatty acid profles moistened with 40% of H2O or D2O: chicken feed or 40% of chicken feed and 60% of fax cake. Although the occurrence of D2O in insect feed increased the larval development time and decreased prepupal weight, it was possible to track the biosynthesis of fatty acids through deuterium labelling. Some fatty acids (decanoic, lauric or myristic acid) were exclusively present in their deuterated form while others (palmitic, palmitoleic or oleic acid) were found in two forms (deuterated or not) indicating that BSF can partially produce these fatty acids via biosynthesis pathways and not only by bioaccumulation from the diet. These results suggest the importance of carbohydrates as a source of acetyl‑CoA in the constitution of the BSF fatty acid profle but also the potential importance of specifc enzymes (e.g. -

Fatty Acids: Structures and Introductory Article Properties Article Contents
Fatty Acids: Structures and Introductory article Properties Article Contents . Introduction Arild C Rustan, University of Oslo, Oslo, Norway . Overview of Fatty Acid Structure . Major Fatty Acids Christian A Drevon, University of Oslo, Oslo, Norway . Metabolism of Fatty Acids . Properties of Fatty Acids Fatty acids play a key role in metabolism: as a metabolic fuel, as a necessary component of . Requirements for and Uses of Fatty Acids in Human all membranes, and as a gene regulator. In addition, fatty acids have a number of industrial Nutrition uses. Uses of Fatty Acids in the Pharmaceutical/Personal Hygiene Industries Introduction doi: 10.1038/npg.els.0003894 Fatty acids, both free and as part of complex lipids, play a number of key roles in metabolism – major metabolic fuel (storage and transport of energy), as essential components subsequent one the b carbon. The letter n is also often used of all membranes, and as gene regulators (Table 1). In ad- instead of the Greek o to indicate the position of the double dition, dietary lipids provide polyunsaturated fatty acids bond closest to the methyl end. The systematic nomencla- (PUFAs) that are precursors of powerful locally acting ture for fatty acids may also indicate the location of double metabolites, i.e. the eicosanoids. As part of complex lipids, bonds with reference to the carboxyl group (D). Figure 2 fatty acids are also important for thermal and electrical outlines the structures of different types of naturally insulation, and for mechanical protection. Moreover, free occurring fatty acids. fatty acids and their salts may function as detergents and soaps owing to their amphipathic properties and the for- Saturated fatty acids mation of micelles. -

Preparation and Properties of Capric–Myristic Acid/Expanded Graphite Composite Phase Change Materials for Latent Heat Thermal Energy Storage
energies Article Preparation and Properties of Capric–Myristic Acid/Expanded Graphite Composite Phase Change Materials for Latent Heat Thermal Energy Storage Dongyi Zhou 1,2,3, Jiawei Yuan 2, Yuhong Zhou 2 and Yicai Liu 1,* 1 School of Energy Science and Engineering, Central South University, Changsha 410083, China; [email protected] 2 School of Mechanical and Energy Engineering, Shaoyang University, Shaoyang 422000, China; [email protected] (J.Y.); [email protected] (Y.Z.) 3 Key Laboratory of Hunan Province for Efficient Power System and Intelligent Manufacturing, Shaoyang University, Shaoyang 422000, China * Correspondence: [email protected]; Tel.: +86-0731-8887-6111 Received: 9 April 2020; Accepted: 6 May 2020; Published: 14 May 2020 Abstract: A novel composite phase change material (CPCM), capric–myristic acid/expanded graphite (CA–MA/EG) CPCM, was prepared by absorbing liquid CA–MA (as the phase change material (PCM)) into EG (as the substrate material) for heat storage in the backfill materials of soil-source heat pump systems. The thermal characteristics and microstructure of the novel CPCM were analyzed using differential scanning calorimetry (DSC) and scanning electronic microscopy (SEM). The thermal conductivities of CA–MA/EG CPCM were surveyed. The thermal stability of the CA–MA/EG was analyzed using thermogravimetric analysis (TGA) and thermal cycle tests. The results showed that the optimal mass content of CA–MA in CPCM was approximately 92.4% and the CA–MA was uniformly distributed in the vesicular structure of EG; the CA–MA/EG CPCM had an appropriate phase change temperature (Tm: 19.78 ◦C, Tf: 18.85 ◦C), high latent heat (Hm: 137.3 J/g, Hf: 139.9 J/g), and excellent thermostability and thermal reliability. -
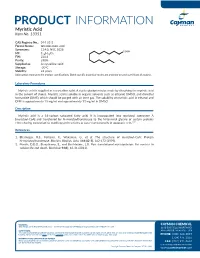
Download Product Insert (PDF)
PRODUCT INFORMATION Myristic Acid Item No. 13351 CAS Registry No.: 544-63-8 Formal Name: tetradecanoic acid Synonyms: C14:0, NSC 5028 COOH MF: C14H28O2 FW: 228.4 Purity: ≥98% Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Myristic acid is supplied as a crystalline solid. A stock solution may be made by dissolving the myristic acid in the solvent of choice. Myristic acid is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF), which should be purged with an inert gas. The solubility of myristic acid in ethanol and DMF is approximately 15 mg/ml and approximately 12 mg/ml in DMSO. Description Myristic acid is a 14-carbon saturated fatty acid. It is incorporated into myristoyl coenzyme A (myristoyl-CoA) and transferred by N-myristoyltransferase to the N-terminal glycine of certain proteins either during translation to modify protein activity or post-translationally in apoptotic cells.1,2 References 1. Bhatnagar, R.S., Fütterer, K., Waksman, G., et al. The structure of myristoyl-CoA: Protein N-myristoyltransferase. Biochim. Biophys. Acta. 1441(2-3), 162-172 (1999). 2. Martin, D.D.O., Beauchamp, E., and Berthiaume, L.G. Post-translational myristoylation: Fat matters in cellular life and death. Biochimie 93(1), 18-31 (2011). WARNING CAYMAN CHEMICAL THIS PRODUCT IS FOR RESEARCH ONLY - NOT FOR HUMAN OR VETERINARY DIAGNOSTIC OR THERAPEUTIC USE. 1180 EAST ELLSWORTH RD SAFETY DATA ANN ARBOR, MI 48108 · USA This material should be considered hazardous until further information becomes available. -

Page 1 of 12Journal Name RSC Advances Dynamic Article Links ►
RSC Advances This is an Accepted Manuscript, which has been through the Royal Society of Chemistry peer review process and has been accepted for publication. Accepted Manuscripts are published online shortly after acceptance, before technical editing, formatting and proof reading. Using this free service, authors can make their results available to the community, in citable form, before we publish the edited article. This Accepted Manuscript will be replaced by the edited, formatted and paginated article as soon as this is available. You can find more information about Accepted Manuscripts in the Information for Authors. Please note that technical editing may introduce minor changes to the text and/or graphics, which may alter content. The journal’s standard Terms & Conditions and the Ethical guidelines still apply. In no event shall the Royal Society of Chemistry be held responsible for any errors or omissions in this Accepted Manuscript or any consequences arising from the use of any information it contains. www.rsc.org/advances Page 1 of 12Journal Name RSC Advances Dynamic Article Links ► Cite this: DOI: 10.1039/c0xx00000x www.rsc.org/xxxxxx ARTICLE TYPE Trends and demands in solid-liquid equilibrium of lipidic mixtures Guilherme J. Maximo, a,c Mariana C. Costa, b João A. P. Coutinho, c and Antonio J. A. Meirelles a Received (in XXX, XXX) Xth XXXXXXXXX 20XX, Accepted Xth XXXXXXXXX 20XX DOI: 10.1039/b000000x 5 The production of fats and oils presents a remarkable impact in the economy, in particular in developing countries. In order to deal with the upcoming demands of the oil chemistry industry, the study of the solid-liquid equilibrium of fats and oils is highly relevant as it may support the development of new processes and products, as well as improve those already existent. -

Acetal Acetaldehyde Acetic Acid Acetone Acetonitrile Acetylcholine
Acetal Butanedione Acetaldehyde Butanone Acetic acid Butenone Acetone Butyraldehyde Acetonitrile Caffeine Acetylcholine Calcium carbonate Acids Caramel Acrolein Carbon, Activated Acrylonitrile Carbon dioxide Acetoin Carbon disulfide Acetophenone Carbon monoxide Acetylpropionyl Cardamom Acetylpyrazine Carob Alanine Catechol Alcohol Catecholamines Aldehydes Catechols Alfalfa extract Cedrol Alkaloids Cellulose Allspice Cherry Amides Chocolate liquor Aminoapthalene Cinnamaldehyde Aminobiphenyl Cinnamic acid Ammonia Cinnamon Ammonium bicarbonate Ammonium Cinnamyl isovalerate carbonate Ammonium chloride Citronella Ammonium hydroxide Citronellol Ammonium sulfide Clove Anethole Cocoa (Chocolate) Anise Cocoa derivatives Asbestos Coconut Ascorbic acid Coffee Asparagine Cognac Aspartic acid Coriander Benzaldehyde Corn syrup Benzene Cresol Benzo(a)pyrene Crotonaldehyde Benzodiazepines Cyclopentene one Benzyl benzoate Dextrose Benzyl cinnamate Diacetyl Benzyl isovalerate Diammonium phosphate Birch Diethylene glycol Butanone Dimethylfuran Butyric acid Dimethylpyrazine Butadiene Esters Ethanolamine Lead Ethyl acetate Lemon Ethyl alcohol Lemongrass Ethyl isobutyrate Levulinic acid Ethyl maltol Licorice Ethyl palmitate Lime Ethyl phenylacetate Limonene Ethyl proprionate Linalool Ethyl vanillin Locust gum Ethylbenzene Limonene Ethylpyridine Magnesium carbonate Eugenol Malic acid Fig Maltol Formaldehyde Maple Fructose Mate Furan Menthol Furfural Mercury Gas phase constituents Metals Gas phase nicotine Methanol Gas phase organics Methoprene Gelatin Methyl -

Interpretive Guide for Fatty Acids
Interpretive Guide for Fatty Acids Name Potential Responses Metabolic Association Omega-3 Polyunsaturated Alpha Linolenic L Add flax and/or fish oil Essential fatty acid Eicosapentaenoic L Eicosanoid substrate Docosapentaenoic L Add fish oil Nerve membrane function Docosahexaenoic L Neurological development Omega-6 Polyunsaturated Linoleic L Add corn or black currant oil Essential fatty acid Gamma Linolenic L Add evening primrose oil Eicosanoid precursor Eicosadienoic Dihomogamma Linolenic L Add black currant oil Eicosanoid substrate Arachidonic H Reduce red meats Eicosanoid substrate Docosadienoic Docosatetraenoic H Weight control Increase in adipose tissue Omega-9 Polyunsaturated Mead (plasma only) H Add corn or black Essential fatty acid status Monounsaturated Myristoleic Palmitoleic Vaccenic Oleic H See comments Membrane fluidity 11-Eicosenoic Erucic L Add peanut oils Nerve membrane function Nervonic L Add fish or canola oil Neurological development Saturated Even-Numbered Capric Acid H Assure B3 adequacy Lauric H Peroxisomal oxidation Myristic H Palmitic H Reduce sat. fats; add niacin Cholesterogenic Stearic H Reduce sat. fats; add niacin Elevated triglycerides Arachidic H Check eicosanoid ratios Behenic H Δ6 desaturase inhibition Lignoceric H Consider rape or mustard seed oils Nerve membrane function Hexacosanoic H Saturated Odd-Numbered Pentadecanoic H Heptadecanoic H Nonadecanoic H Add B12 and/or carnitine Propionate accumulation Heneicosanoic H Omega oxidation Tricosanoic H Trans Isomers from Hydrogenated Oils Palmitelaidic H Eicosanoid interference Eliminate hydrogenated oils Total C18 Trans Isomers H Calculated Ratios LA/DGLA H Add black currant oil Δ6 desaturase, Zn deficiency EPA/DGLA H Add black currant oil L Add fish oil Eicosanoid imbalance AA/EPA (Omega-6/Omega-3) H Add fish oil Stearic/Oleic (RBC only) L See Comments Cancer Marker Triene/Tetraene Ratio (plasma only) H Add corn or black currant oil Essential fatty acid status ©2007 Metametrix, Inc. -

Myristic Acid Produces Anxiolytic-Like Effects in Wistar Rats in the Elevated Plus Maze
Hindawi Publishing Corporation BioMed Research International Volume 2014, Article ID 492141, 8 pages http://dx.doi.org/10.1155/2014/492141 Research Article Myristic Acid Produces Anxiolytic-Like Effects in Wistar Rats in the Elevated Plus Maze Carlos M. Contreras,1,2 Juan Francisco Rodríguez-Landa,2 Rosa Isela García-Ríos,2 Jonathan Cueto-Escobedo,2 Gabriel Guillen-Ruiz,2 and Blandina Bernal-Morales2 1 Unidad Periferica´ Xalapa, Instituto de Investigaciones Biomedicas,´ Universidad Nacional Autonoma´ de Mexico,´ 91190 Xalapa, VER, Mexico 2 Laboratorio de Neurofarmacolog´ıa, Instituto de Neuroetolog´ıa, Universidad Veracruzana, Avenida Dr. Luis Castelazo s/n, Colonia Industrial Las Animas,91190Xalapa,VER,Mexico´ Correspondence should be addressed to Carlos M. Contreras; [email protected] Received 17 July 2014; Revised 1 September 2014; Accepted 4 September 2014; Published 18 September 2014 Academic Editor: Saulius Butenas Copyright © 2014 Carlos M. Contreras et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. A mixture of eight fatty acids (linoleic, palmitic, stearic, myristic, elaidic, lauric, oleic, and palmitoleic acids) at similar concentrations identified in human amniotic fluid produces anxiolytic-like effects comparable to diazepam in Wistar rats. However, individual effects of each fatty acid remain unexplored. In Wistar rats, we evaluated the separate action of each fatty acidat the corresponding concentrations previously found in human amniotic fluid on anxiety-like behaviour. Individual effects were compared with vehicle, an artificial mixture of the same eight fatty acids, and a reference anxiolytic drug (diazepam, 2 mg/kg). -

United States Patent (10) Patent No.: US 8,835,369 B2 Cifeli (45) Date of Patent: Sep
USOO8835369B2 (12) United States Patent (10) Patent No.: US 8,835,369 B2 Cifeli (45) Date of Patent: Sep. 16, 2014 (54) ODORLESSACETONE-FREE NAIL POLISH 2008/0207933 A1* 8/2008 Bigorra Llosas et al. ....... 554/52 REMOVING COMPOSITION 2008/0241089 A1 * 10, 2008 Banowski et al. .............. 424,65 2009 OO68255 A1* 3, 2009 Yu et al. ......... ... 424/450 O - O 2009/0162446 A1* 6/2009 Gatto et al. ................... 424/489 (75) Inventor: Dana Cifeli, Clark, NJ (US) 2009,0191138 A1 7, 2009 Dechow 2010/0204076 A1 8/2010 Cheng (73) Assignee: L'Oreal, Paris (FR) - FOREIGN PATENT DOCUMENTS (*) Notice: Subject to any disclaimer, the term of this patent is extended or adjusted under 35 CN 101112351 A 1, 2008 U.S.C. 154(b) by 134 days. CN 101953.769. A 1, 2011 DE 202009000908 U1 6, 2009 (21) Appl. No.: 13/487,639 JP 2006182674 A T 2006 OTHER PUBLICATIONS (22) Filed: Jun. 4, 2012 English Abstract of CN-10 1953769-A. (65) Prior Publication Data English Abstract of CN-101112351-A. English Abstract of JP-2006182674-A. US 2013/0319462 A1 Dec. 5, 2013 Notification of Transmittal of the International Search Report and the Written Opinion of the International Searching Authority, or the (51) Int. Cl. Declaration, International Application No. PCT/US2013/042406, CID 3/43 (2006.01) mailed Nov. 12, 2013, including International Search Report and CI ID3/20 (2006.01) Written Opinion of the ISA. (52) U.S. Cl. CPC ................ CIID3/43 (2013.01); C1 1D3/2093 * cited by examiner (2013.01) USPC ........................................... 510/118, 5.10/407 Primary Examiner — Gregory Webb (58) Field of Classification Search (74) Attorney, Agent, or Firm — Novak Druce Connolly CPC .............................