Patent Foramen Ovale: Current Pathology, Pathophysiology, And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -
Heart and Circulatory System I
Heart and Circulatory System I Daphne T. Hsu, MD Professor of Clinical Pediatrics [email protected] Outline • Vasculogenesis • Embryonic Folding • Formation of the Primary Heart Tube • Looping • Atrial Septation • Primitive Ventricular Septum • Atrioventricular Canal/Endocardial Cushions • Conotruncal Septation • Ventricular septation • Congenital Heart Defects CARDIOVASCULAR SYSTEM: EARLY DEVELOPMENT: WEEK 3 EMBRYONIC FOLDING: WEEK 4 Formation of Heart Tube (17-22 days) Heart Development: 26 days PRIMITIVE HEART TUBE: WEEK 4 Cardiac Loop (8-16 somites) VENTRICULAR LOOPING END WEEK 4 NORMAL : Loop to the RIGHT: Levocardia! ABNORMAL: Loop to the LEFT: Dextrocardia! FROM TUBE TO FOUR CHAMBERS INTERNAL VIEW Formation of Primitive Ventricles Atrial Septation: 3 Septums Primum, Secundum, Intermedium Endocardial Cushion: 80 days Endocardial Cushions • Atrioventricular Canal: Divide between the atria and ventricles • Endocardial Cushions: Four tissue expansions found in periphery of AV canal – Atrial septation – Atrioventricular valve formation: Mitral and Tricuspid Valves – Ventricular septation Endocardial Cushions • Superior-Inferior cushions – Septum Intermedium – Inferior atrial septum – Posterior/superior ventricular septum • Right and Left Cushions – Ventricular myocardium – Mitral valve – Tricuspid valve Atrioventricular Valve Formation • Left and Right Endocardial Cushions FOUR CHAMBERS- ULTRASOUND VIEW @ 20 wks Congenital Heart Defect: Endocardial Cushion Defect Normal Endocardial Cushion Defect Ventricular Outflow Tracts and Great -

A 29-Year-Old Man with Acute Onset Blurry Vision, Weakness, and Gait Abnormality
Journal of the Louisiana State Medical Society CLINICAL CASE OF THE MONTH A 29-Year-Old Man With Acute Onset Blurry Vision, Weakness, and Gait Abnormality Deepu Thoppil, MD; Murtuza J. Ali, MD; Neeraj Jain, MD; Sanjay Kamboj, MD; Pramilla Subramaniam, MD; and Fred A. Lopez, MD (Section Editor) A 29-year-old man, with no significant past medical history, was in his usual state of health until the afternoon of admission. The patient was seated at work eating lunch when he suddenly noticed that his vision became blurry. He covered his right eye and had no visual difficulty but noted blurry vision upon covering his left eye. At this point, the patient tried to stand up, but had difficulty walking and noticed he was “falling toward his left.” Facial asymmetry when smiling was also appreciated. The patient denied any alteration in mental status, confusion, antecedent or current headaches, aura, chest pains, or shortness of breath. He was not taking any prescribed medications and had no known allergies. The patient denied any prior hospitalization or surgery. He denied use of tobacco, alcohol, or illicit drugs, and worked as a maintenance worker in a hotel. His family history is remarkable for his father who died of pancreatic cancer in his 50s and his mother who died of an unknown heart condition in her late 40s. Vital signs on presentation to the emergency department included temperature of 97.6oF; respiratory rate of 18 per minute; pulse of 68 per minute; blood pressure of 124/84 mmHg; pulse oximetry of 99% on ambient air. -
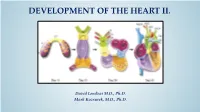
Development of Right Ventricle
DEVELOPMENT OF THE HEART II. David Lendvai M.D., Ph.D. Mark Kozsurek, M.D., Ph.D. • Septation of the common atrioventricular (AV) orifice. • Formation of the interatrial septum. • Formation of the muscular interventricular septum. • Appearance of the membranous interventricular septum and the spiral aorticopulmonary septum. right left septum primum septum primum septum primum septum primum septum primum septum primum foramen primum foramen primum septum primum septum primum foramen primum foramen primum septum primum septum primum foramen secundum foramen secundum foramen primum foramen primum septum primum foramen secundum septum primum foramen secundum foramen primum foramen primum septum primum septum primum foramen secundum foramen secundum septum secundum septum secundum foramen secundum foramen ovale foramen ovale septum primum septum primum septum secundum septum secundum foramen secundum foramen ovale foramen ovale septum primum septum primum septum secundum septum secundum foramen secundum septum primum foramen ovale foramen ovale septum primum SUMMARY • The septation of the common atrium starts with the appearance of the crescent-shaped septum primum. The opening of this septum, the foramen primum, becomes progressively smaller. • Before the foramen primum completly closes, postero-superiorly several small openings appear on the septum primum. These perforations coalesce later and form the foramen secundum. • On the right side of the septum primum a new septum, the septum secundum, starts to grow. The orifice of the septum secundum is the foramen ovale. • Finally two crescent-like, incomplete, partially overlapping septa exist with one hole on each. Septum secundum is more rigid and the septum primum on its left side acts as a valve letting the blood flow exclusively from the right to the left. -

The Zebrafish Cardiac Endothelial Cell—Roles in Development And
Journal of Cardiovascular Development and Disease Review The Zebrafish Cardiac Endothelial Cell—Roles in Development and Regeneration Vanessa Lowe 1, Laura Wisniewski 2 and Caroline Pellet-Many 3,* 1 Heart Centre, Barts & The London School of Medicine, William Harvey Research Institute, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK; [email protected] 2 Centre for Tumour Microenvironment, Barts Cancer Institute, Queen Mary University London, Charterhouse Square, London EC1M 6BQ, UK; [email protected] 3 Department of Comparative Biomedical Sciences, Royal Veterinary College, 4 Royal College Street, London NW1 0TU, UK * Correspondence: [email protected] Abstract: In zebrafish, the spatiotemporal development of the vascular system is well described due to its stereotypical nature. However, the cellular and molecular mechanisms orchestrating post-embryonic vascular development, the maintenance of vascular homeostasis, or how coronary vessels integrate into the growing heart are less well studied. In the context of cardiac regeneration, the central cellular mechanism by which the heart regenerates a fully functional myocardium relies on the proliferation of pre-existing cardiomyocytes; the epicardium and the endocardium are also known to play key roles in the regenerative process. Remarkably, revascularisation of the injured tissue occurs within a few hours after cardiac damage, thus generating a vascular network acting as a scaffold for the regenerating myocardium. The activation of the endocardium leads to the secretion of cytokines, further supporting the proliferation of the cardiomyocytes. Although epicardium, Citation: Lowe, V.; Wisniewski, L.; endocardium, and myocardium interact with each other to orchestrate heart development and Pellet-Many, C. The Zebrafish Cardiac regeneration, in this review, we focus on recent advances in the understanding of the development of Endothelial Cell—Roles in the endocardium and the coronary vasculature in zebrafish as well as their pivotal roles in the heart Development and Regeneration. -

Persistent Patent Foramen Ovale in Adult Male
Internatiional Journal of Biioassays ISSN: 2278-778X www.ijbio.com Case Report PERSISTENT PATENT FORAMEN OVALE IN ADULT MALE Santhoshkumar N, Kunjumon PC and Anju Balaji More* Department of Anatomy, Sree Mookambika Institute of Medical Sciences, Kulasekharam, Tamilnadu, 629161, India Received for publication: February 17, 2014; Accepted: March 13, 2014 Abstract: In this case report, we want to present a persistent foramen ovale with length of 1.4 cm in an adult male cadaver approximately 60 years of age. The person had a heavy built up and appeared well nourished. The foramen ovale is a normal interatrial communication during fetal life. The persistence of this opening in the later life may go unnoticed if asymptomatic. But symptoms can begin in adult life due to pulmonary hypertension. It will become an added complication to any cardio-vascular disorder developing in later life. With no other anomalous findings in the heart, it appears that the foramen ovale was probe patent. There are five types of foramen ovale according to its location. The present finding belongs to type I that is patent foramen ovale of ostium secundum type. Echocardiogram, Electrocardiogram, Doppler image, Cardiac catheterization, Chest x-ray and MRI of the heart are the various imaging techniques which can detect this variance. Keywords: Atrium, Foramen ovale (Patent oval foramen), Fossa ovalis (Oval fossa). INTRODUCTION An atrial septal defect (ASD) is an opening in made available for the purpose of dissection under the interatrial septum. It allows oxygen rich blood in Anatomy Act. left atrium to mix with oxygen-poor blood in right atrium. -
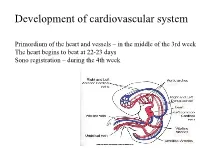
Primitive Blood Circulation. • Heart Development (Dev. of Heart Tube, Septa and Valves) • Aortal Arches and Their Derivatives
Development of cardiovascular system Primordium of the heart and vessels – in the middle of the 3rd week The heart begins to beat at 22-23 days Sono registration – during the 4th week • Primitive blood circulation. • Heart development (dev. of heart tube, septa and valves) • Aortal arches and their derivatives. • Fetal blood circulation. • Cardiovascular system malformations. Vessels development: (from week 3) hemangiogenesis - blood islands (insulae sanguinae) DAY 15 – 16 in extraembryonic mesoderm of - yolk sac (vasa omphalomesenterica /vitellina/), - connecting stalk and placenta (vasa umbilicalia) DAY 17 – 18 in mesenchyme of embryo Groups of angiogenic cells in mesenchyma ectoderm Blood islet mesenchyme angioblasts endoderm hemoblasts primitive erythrocytes primitive endothelium Differentiation of mesenchymal cells angiogenic cells: - angioblasts endothelium (at the periphery of blood islets) - hemoblasts primitive erythrocytes (in the center of blood islets) angiogenic cells form a "horseshoe-shaped" space between somatic and splanchnic layer of mesoderm = pericardial cavity. Two endothelial tubes arrise in splanchnic mesoderm. The ventral portion with tubes forms the cardiogenic area two heart tubes, while the lateral portions form the dorsal aortae. Cardiogenic region just cranial to the prechordal plate. Fusion of heart tubes mesocardium dorsale diferentiation of heart wall: endocardium ● heart jelly epimyocardium Vitelline, umbilical and intraembryonic vessels fuse together and form the primitive blood circulation ( fetal blood circulation!) Pericardial cavity Cor tubulare simplex Septum transversum branchial arteries 1-6 Right Leftt Desc.aorta Ventral wiew Truncus arteriosus Asc.aorta Sinus venosus right horn degenerate Saccus aorticus Vessels v. cardinalis ant. sin. + v. cardinalis com.sin. cor tubulare Yolk sac v. cardinalis post. sin. aa.omphalomesentericae a. mesenterica sin. -

The Sinus Venosus Typeof Interatrial Septal Defect*
Thorax: first published as 10.1136/thx.13.1.12 on 1 March 1958. Downloaded from Thorax (I9%8), 13, 12. THE SINUS VENOSUS TYPE OF INTERATRIAL SEPTAL DEFECT* BY H. R. S. HARLEY Cardiff (RECEIVED FOR PUBLICATION DECEMBER 30, 1957) Defects of the interatrial septum, other than namely, (1) it lies above and independent of valvular patency of the foramen ovale, are often the fossa ovalis; (2) its margin is incomplete, classified into ostium primum and ostium secun- being absent superiorly and incomplete pos- dum varieties. The relationship of the former type teriorly; and (3) it is associated with anomalous to abnormal development of the atrioventricular drainage of the right superior, and sometimes of canal has been stressed by several workers, includ- the right middle or inferior, pulmonary vein. This ing Rogers and Edwards (1948), Wakai and type of defect is illustrated in Fig. 1 (after Lewis Edwards (1956), Wakai, Swan, and Wood (1956), et al., 1955) and Fig. 2 (after Geddes, 1912). In Brandenburg and DuShane (1956), Toscano- the case reported by Ross (1956), who kindly per- Barbosa, Brandenburg, and Burchell (1956), and mitted me to see the heart, the interatrial Cooley and Kirklin (1956). These workers prefer communication was described as ". lying the term "persistent common within the orifice of atrioventricular the superior vena cava in itscopyright. canal " to "persistent ostium primum." medial wall opposite the mouths of the anomalous In addition to the above types of interatrial pulmonary veins." Ross goes on to say: "On septal defect there is a third variety, which was casual inspection of the interior of the left atrium, described as long ago as 1868 by Wagstaffe, but the defect was not visible unless a search was made which has come into prominence only since the within the superior caval orifice." The relation- http://thorax.bmj.com/ introduction of surgical repair of interatrial ship of the defect to the orifice of the superior communications under direct vision. -

THE CARDIOVASCULAR SYSTEM the Picture Shows the Tranverse Section of the Embryo Demonstrating the Formation of the Angioblastic Cords
EMBRYOLOGY: THE CARDIOVASCULAR SYSTEM The picture shows the tranverse section of the embryo demonstrating the formation of the angioblastic cords . In which region do these cords develop? The picture shows the lateral folding of the embryo and the fusion of the endocardial heart tubes . What is the significance of this folding? This picture shows the formation of cardiac loop . What are the five dilatations which form on the primordial heart tube? . What results in the bending of the heart tube? The picture shows the structure of a primordial heart . Give the three pairs of veins which are received by the sinus nenosus. The picture shows blood circulation through a primordial heart . Describe the circulation of blood through the primordial heart. The picture shows the formation of endocardial cushions . What are endocardial cushions and what is their significance? The picture shows the septation of the atrium in the primordial heart . Give the two septa which are responsible for the formation of the interatrial septa. What results in the perforations denoted by the red arrows? . What results in the formation of foramen primum and foramen secundum? . What is its significance? . What result in the formation of foramen ovale? What is the significance of this foramen? . What structure does formen ovale forms in the adult? The diagram shows the division of the sinus venosus into the left and right horns . Which structure is responsible for this division? . What are the derivatives/remnants of the left horn of the sinus venosus? . What is the fate of the right horn of the sinus venosus? The picture shows the absorption of the pulmonary vein into the left atrium . -

Study of Morphological Characteristics of Fossa Ovalis and Its Clinical Importance - a Cadaveric Study Dr
Scholars International Journal of Anatomy and Physiology Abbreviated Key Title: Sch Int J Anat Physiol ISSN 2616-8618 (Print) |ISSN 2617-345X (Online) Scholars Middle East Publishers, Dubai, United Arab Emirates Journal homepage: http://saudijournals.com/sijap/ Original Research Article Study of Morphological Characteristics of Fossa Ovalis and Its Clinical Importance - A Cadaveric Study Dr. Ashita Kaore1, Dr. Ashish Kamdi2*, Dr. N. Y. Kamdi3 1Assistant Professor, DepartmentofAnatomy, Government Medical College, Nagpur, Maharashtra, India 2Assistant Professor, Department of Anatomy, Government Medical College, Chhindwara, Madhya Pradesh, India 3Professor and Head, Department of Anatomy, Government Medical College, Nagpur Maharashtra, India *Corresponding author: Dr. Ashish Kamdi | Received: 02.03.2019 | Accepted: 05.03.2019 | Published: 30.03.2019 DOI:10.21276/sijap.2019.2.3.2 Abstract Transseptal access from right atrium to left atrium through the fossa ovalis using transseptal puncture and patent fossa ovalis repair are widely used cardiac techniques. These techniques require through knowledge of the cardiac anatomy especially of the fossa ovalis .Evaluation of the various morphological parameters of the fossa ovalis forms an important prerequisite before undertaking any surgical procedure in this region. This study was conducted on 60 cadaveric hearts from the department of Anatomy, Government medical college, Nagpur. The right atrium was opened and the fossa ovalis was studied for its shape, size, floor and the prominence and extent of the limbus fossa ovalis was noted. The fossa ovalis was observed for the presence of any patent foramen ovale or probe patency. In majority of the cases the shape of fossa ovalis was found to be oval 66.7% cases, the average craniocaudal diameter was found to be 15.03mm, and average anteroposterior diameter was found to be 14.44mm. -

Development of Heart Notes
Formation of heart tube: 3rd week Heart beat: 22nd –23rd day (beginning of fourth week) USG detection of heart beat: 7th week Foetal ECG: 11th week Endocardium from original heart tube Myocardium from surrounding mesoderm & epicardium (myoepicardial mantle) (visceral pericardium) Lining of pericardium epithelium of pericardial cavity Transverse sinus formed by disappearance of dorsal mesocardium (Present between arterial and venous ends of the heart tube) FATE Of SINUS VENOSUS Left horn of sinus venosus, along with medial part of common cardinal vein forms coronary sinus Lateral part of common cardinal vein forms oblique vein of left atrium Left venous valve merges with septum secundum. Right venous valve is divided in three parts by appearance of two transverse muscular bands, called limbic bands. i) The part above superior limbic band forms crista terminalis ii) The part between the two bands forms valve of inferior vena cava iii) The part below the inferior limbic band forms valve of coronary sinus INTERATRIAL SEPTUM i) Upper, thicker part is formed by septum secundum ii) Lower, thin part (floor of fossa ovalis) is formed by septum primum iii) Sharp margin of fossa ovalis is formed by lower, curved margin of septum secundum DEVELOPMENT OF RIGHT ATRIUM It develops from 1. Right half of primitive atrial chamber (rough part); 2. Absorption of right horn of sinus venosus (smooth part) and 3. Right atrioventricular canal. DEVELOPMENT OF LEFT ATRIUM It develops from 1. Left half of primitive atrial chamber (rough part – confined to the auricle); 2. Absorption of pulmonary veins (smooth part) and 3. Left atrioventricular canal. -

Atrioventricular Node (AVN) Originates from (I) the Left Wall of Sinus Venosus and (Ii) Superior Endocardial Cushion of the Atriventricular Canal
W.S. O School of Biomedical Sciences, University of Hong Kong Objectives: • Describe early angiogenesis. • Describe the heart tube formation. • Describe the partitioning into a 4- chambered heart. • List the formation of heart valves and the conducting system in the heart. • Explain the basis of congenital heart malformation. Day 25 Day 20 Heart tubes and Intraembryonic embryonic vessels circulation established develop 6 weeks 4-5 weeks Heart tube partitions into 4 Aortic arches heart chambers transform 8 weeks Heart valves Birth completed Foramen ovale closes with increased blood flow from lungs Blood and blood vessels Primitive blood cells Angioblast (mesodermal) Endothelial cells Connective tissue surrounding mesoderm Smooth muscles Blood vessels formation The three parts of circulation: vitelline, chorionic & intraembryonic Molecular regulation of cardiac development • Heart induction – BMPs secreted by endoderm and lateral plate mesoderm together with inhibition of WNT in the anterior part of the embryo induce the expression of NKX-2.5 in the heart -forming region . • Cardiac looping - is induced by the nodal and lefty2 genes. These two genes induce the transcription factor of PITX2 in deposition of extracellular matrix in looping. Development of the heart - 1 1. Cardiogenic plate appears around 3rd week Anterior to prochordal plate Pericardial coelom develop around heart tube 2. Rotation of heart primordia –180 rotation 3. Fusion of heart tubes around 4th week; 4. Differentiation of the heart tube tissue Epicardium – connective tissue Myocardium – cardiac muscle Subendocardium – spongy reticular tissue Endocardium - endothelium Embryonic development of the heart. (a) Endocardial heart tubes start to fuse, (b) Fusion of heart tubes complete, (c) Division of heart tube into dilated segments, (d) Looping of the heart tube, (e) Looping complete, (f) Frontal section of heart tube.