Dermatological Emergencies “The Eschar”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fungal Infections from Human and Animal Contact
Journal of Patient-Centered Research and Reviews Volume 4 Issue 2 Article 4 4-25-2017 Fungal Infections From Human and Animal Contact Dennis J. Baumgardner Follow this and additional works at: https://aurora.org/jpcrr Part of the Bacterial Infections and Mycoses Commons, Infectious Disease Commons, and the Skin and Connective Tissue Diseases Commons Recommended Citation Baumgardner DJ. Fungal infections from human and animal contact. J Patient Cent Res Rev. 2017;4:78-89. doi: 10.17294/2330-0698.1418 Published quarterly by Midwest-based health system Advocate Aurora Health and indexed in PubMed Central, the Journal of Patient-Centered Research and Reviews (JPCRR) is an open access, peer-reviewed medical journal focused on disseminating scholarly works devoted to improving patient-centered care practices, health outcomes, and the patient experience. REVIEW Fungal Infections From Human and Animal Contact Dennis J. Baumgardner, MD Aurora University of Wisconsin Medical Group, Aurora Health Care, Milwaukee, WI; Department of Family Medicine and Community Health, University of Wisconsin School of Medicine and Public Health, Madison, WI; Center for Urban Population Health, Milwaukee, WI Abstract Fungal infections in humans resulting from human or animal contact are relatively uncommon, but they include a significant proportion of dermatophyte infections. Some of the most commonly encountered diseases of the integument are dermatomycoses. Human or animal contact may be the source of all types of tinea infections, occasional candidal infections, and some other types of superficial or deep fungal infections. This narrative review focuses on the epidemiology, clinical features, diagnosis and treatment of anthropophilic dermatophyte infections primarily found in North America. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Review Article Sporotrichosis: an Overview and Therapeutic Options
Hindawi Publishing Corporation Dermatology Research and Practice Volume 2014, Article ID 272376, 13 pages http://dx.doi.org/10.1155/2014/272376 Review Article Sporotrichosis: An Overview and Therapeutic Options Vikram K. Mahajan Department of Dermatology, Venereology & Leprosy, Dr. R. P. Govt. Medical College, Kangra, Tanda, Himachal Pradesh 176001, India Correspondence should be addressed to Vikram K. Mahajan; [email protected] Received 30 July 2014; Accepted 12 December 2014; Published 29 December 2014 Academic Editor: Craig G. Burkhart Copyright © 2014 Vikram K. Mahajan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Sporotrichosis is a chronic granulomatous mycotic infection caused by Sporothrix schenckii, a common saprophyte of soil, decaying wood, hay, and sphagnum moss, that is endemic in tropical/subtropical areas. The recent phylogenetic studies have delineated the geographic distribution of multiple distinct Sporothrix species causing sporotrichosis. It characteristically involves the skin and subcutaneous tissue following traumatic inoculation of the pathogen. After a variable incubation period, progressively enlarging papulo-nodule at the inoculation site develops that may ulcerate (fixed cutaneous sporotrichosis) or multiple nodules appear proximally along lymphatics (lymphocutaneous sporotrichosis). Osteoarticular sporotrichosis or primary pulmonary sporotrichosis are rare and occur from direct inoculation or inhalation of conidia, respectively. Disseminated cutaneous sporotrichosis or involvement of multiple visceral organs, particularly the central nervous system, occurs most commonly in persons with immunosuppression. Saturated solution of potassium iodide remains a first line treatment choice for uncomplicated cutaneous sporotrichosis in resource poor countries but itraconazole is currently used/recommended for the treatment of all forms of sporotrichosis. -

CHAPTER E16 Atlas of Skin Manifestations of Internal Disease CHAPTER E16 Thomas J
CHAPTER e16 Atlas of Skin Manifestations of Internal Disease CHAPTER e16 Thomas J. Lawley Robert A. Swerlick In the practice of medicine, virtually every clinician encounters patients with skin disease. Physicians of all specialties face the daily task of determining the nature and clinical implication of dermatologic disease. In patients with skin eruptions and rashes, the physician must confront the question of whether the cutaneous Atlas of Skin Manifestations Internal Disease process is confined to the skin, representing a pure dermatologic event, or whether it is a manifestation of internal disease relating to the patient’s overall medical condition. Evaluation and accurate diagnosis of skin lesions are also critical given the marked rise in both melanoma and nonmelanoma skin cancer. Dermatologic conditions can be classified and categorized in many different ways, Figure e16-2 Acne rosacea with prominent facial erythema, telangiecta- and in this Atlas, a selected group of inflammatory skin eruptions sias, scattered papules, and small pustules. (Courtesy of Robert Swerlick, and neoplastic conditions are grouped in the following manner: MD; with permission.) (A) common skin diseases and lesions, (B) nonmelanoma skin cancer, (C) melanoma and pigmented lesions, (D) infectious dis- ease and the skin, (E) immunologically mediated skin disease, and (F) skin manifestations of internal disease. COMMON SKIN DISEASES AND LESIONS ( Figs. e16-1 to e16-19) In this section, several common inflamma- tory skin diseases and benign neoplastic and reactive lesions are presented. While most of these dermatoses usually present as a pre- dominantly dermatologic process, underlying systemic associations may be made in some settings. Atopic dermatitis is often present in patients with an atopic diathesis, including asthma and sinusitis. -
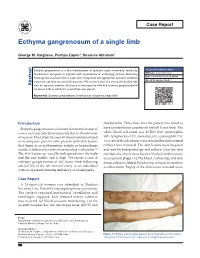
Ecthyma Gangrenosum of a Single Limb
Case Report Ecthyma gangrenosum of a single limb George M. Varghese, Pushpa Eapen1, Susanne Abraham1 Ecthyma gangrenosum is a skin manifestation of systemic sepsis commonly caused by Access this article online Pseudomonas aeruginosa in patients with neutropenia or underlying immune deficiency. Website: www.ijccm.org Although the usual outcome is poor, early recognition and appropriate systemic antibiotic DOI: 10.4103/0972-5229.84898 treatment can lead to successful outcome. We report a case of a previously healthy lady Quick Response Code: Abstract with no apparent immune deficiency or neutropenia who had ecthyma gangrenosum of left lower limb in which the arterial line was placed. Keywords: Ecthyma gangrenosum, Pseudomonas aeruginosa, single limb Introduction thachycardia. Three days later the patient was noted to Ecthyma gangrenosum is a known skin manifestation of have erythematous papules on the left lower limb. The 3 severe systemic infection commonly due to Pseudomonas white blood cell count was 16,500/mm (neutrophils aeruginosa. Most often it is seen in immunocompromised 84%, lymphocytes 12%, monocytes 3%, eosinophils 1%). or neutropenic patients who present with skin lesions Two sets of blood cultures were sent and the intra-arterial that begin as an erythematous nodule or hemorrhagic catheter was removed. The skin lesions were biopsied vesicle, which evolves into a necrotic ulcer with eschar. [1] and sent for histopathology and culture. Over the next The skin lesions are usually widespread over the body few days the skin lesions became blackish with necrotic and the case fatality rate is high. We report a case of areas (arrow) [Figure 1]. The blood, catheter tip, and skin ecthyma gangrenosum of left lower limb following lesion cultures yielded Pseudomonas aeruginosa sensitive arterial line in the left femoral artery in an individual to ceftazidime. -

Skin and Soft Tissue Infections Following Marine Injuries
CHAPTER 6 Skin and Soft Tissue Infections Following Marine Injuries V. Savini, R. Marrollo, R. Nigro, C. Fusella, P. Fazii Spirito Santo Hospital, Pescara, Italy 1. INTRODUCTION Bacterial diseases following aquatic injuries occur frequently worldwide and usually develop on the extremities of fishermen and vacationers, who are exposed to freshwater and saltwater.1,2 Though plenty of bacterial species have been isolated from marine lesions, superficial soft tissue and invasive systemic infections after aquatic injuries and exposures are related to a restricted number of microorganisms including, in alphabetical order, Aeromonas hydrophila, Chromobacterium violaceum, Edwardsiella tarda, Erysipelothrix rhusiopathiae, Myco- bacterium fortuitum, Mycobacterium marinum, Shewanella species, Streptococcus iniae, and Vibrio vulnificus.1,2 In particular, skin disorders represent the third most common cause of morbidity in returning travelers and are usually represented by bacterial infections.3–12 Bacterial skin and soft tissue infectious conditions in travelers often follow insect bites and can show a wide range of clinical pictures including impetigo, ecthyma, erysipelas, abscesses, necro- tizing cellulitis, myonecrosis.3–12 In general, even minor abrasions and lacerations sustained in marine waters should be considered potentially contaminated with marine bacteria.3–12 Despite variability of the causative agents and outcomes, the initial presentations of skin and soft tissue infections (SSTIs) complicating marine injuries are similar to those occurring after terrestrial exposures and usually include erysipelas, impetigo, cellulitis, and necrotizing infections.3 Erysipelas is characterized by fiery red, tender, painful plaques showing well-demarcated edges, and, though Streptococcus pyogenes is the major agent of this pro- cess, E. rhusiopathiae infections typically cause erysipeloid displays.3 Impetigo is initially characterized by bullous lesions and is usually due to Staphylococcus aureus or S. -

| Oa Tai Ei Rama Telut Literatur
|OA TAI EI US009750245B2RAMA TELUT LITERATUR (12 ) United States Patent ( 10 ) Patent No. : US 9 ,750 ,245 B2 Lemire et al. ( 45 ) Date of Patent : Sep . 5 , 2017 ( 54 ) TOPICAL USE OF AN ANTIMICROBIAL 2003 /0225003 A1 * 12 / 2003 Ninkov . .. .. 514 / 23 FORMULATION 2009 /0258098 A 10 /2009 Rolling et al. 2009 /0269394 Al 10 /2009 Baker, Jr . et al . 2010 / 0034907 A1 * 2 / 2010 Daigle et al. 424 / 736 (71 ) Applicant : Laboratoire M2, Sherbrooke (CA ) 2010 /0137451 A1 * 6 / 2010 DeMarco et al. .. .. .. 514 / 705 2010 /0272818 Al 10 /2010 Franklin et al . (72 ) Inventors : Gaetan Lemire , Sherbrooke (CA ) ; 2011 / 0206790 AL 8 / 2011 Weiss Ulysse Desranleau Dandurand , 2011 /0223114 AL 9 / 2011 Chakrabortty et al . Sherbrooke (CA ) ; Sylvain Quessy , 2013 /0034618 A1 * 2 / 2013 Swenholt . .. .. 424 /665 Ste - Anne -de - Sorel (CA ) ; Ann Letellier , Massueville (CA ) FOREIGN PATENT DOCUMENTS ( 73 ) Assignee : LABORATOIRE M2, Sherbrooke, AU 2009235913 10 /2009 CA 2567333 12 / 2005 Quebec (CA ) EP 1178736 * 2 / 2004 A23K 1 / 16 WO WO0069277 11 /2000 ( * ) Notice : Subject to any disclaimer, the term of this WO WO 2009132343 10 / 2009 patent is extended or adjusted under 35 WO WO 2010010320 1 / 2010 U . S . C . 154 ( b ) by 37 days . (21 ) Appl. No. : 13 /790 ,911 OTHER PUBLICATIONS Definition of “ Subject ,” Oxford Dictionary - American English , (22 ) Filed : Mar. 8 , 2013 Accessed Dec . 6 , 2013 , pp . 1 - 2 . * Inouye et al , “ Combined Effect of Heat , Essential Oils and Salt on (65 ) Prior Publication Data the Fungicidal Activity against Trichophyton mentagrophytes in US 2014 /0256826 A1 Sep . 11, 2014 Foot Bath ,” Jpn . -

Cutaneous Manifestations of Infection in the Immunocompromised Host
Cutaneous Manifestations of Infection in the Immunocompromised Host Marc E. Grossman • Lindy P. Fox • Carrie Kovarik Misha Rosenbach Cutaneous Manifestations of Infection in the Immunocompromised Host Second Edition Authors Marc E. Grossman, M.D. Carrie Kovarik, M.D. Professor of Clinical Dermatology Assistant Professor of Dermatology College of Physicians and Surgeons Dermatopathology, and Infectious Diseases Director, Hospital Consultation Service University of Pennsylvania New York Presbyterian Hospital Philadelphia, Pennsylvania, USA Columbia University Medical Center New York, New York, USA Misha Rosenbach, M.D. Assistant Professor of Dermatology Lindy P. Fox, M.D. and Internal Medicine Associate Professor of Clinical Dermatology Director, Dermatology Inpatient Consult Service Director, Hospital Consultation Service University of Pennsylvania University of California, San Francisco Philadelphia, Pennsylvania, USA San Francisco, California, USA ISBN 978-1-4419-1577-1 e-ISBN 978-1-4419-1578-8 DOI 10.1007/978-1-4419-1578-8 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2011933837 Springer Science+Business Media, LLC 2012 All rights reserved. Th is work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter devel- oped is forbidden. Th e use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identifi ed as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. -

Application to Add Itraconazole and Voriconazole to the Essential List of Medicines for Treatment of Fungal Diseases – Support Document
Application to add itraconazole and voriconazole to the essential list of medicines for treatment of fungal diseases – Support document 1 | Page Contents Page number Summary 3 Centre details supporting the application 3 Information supporting the public health relevance and review of 4 benefits References 7 2 | Page 1. Summary statement of the proposal for inclusion, change or deletion As a growing trend of invasive fungal infections has been noticed worldwide, available few antifungal drugs requires to be used optimally. Invasive aspergillosis, systemic candidiasis, chronic pulmonary aspergillosis, fungal rhinosinusitis, allergic bronchopulmonary aspergillosis, phaeohyphomycosis, histoplasmosis, sporotrichosis, chromoblastomycosis, and relapsed cases of dermatophytosis are few important concern of southeast Asian regional area. Considering the high burden of fungal diseases in Asian countries and its associated high morbidity and mortality (often exceeding 50%), we support the application of including major antifungal drugs against filamentous fungi, itraconazole and voriconazole in the list of WHO Essential Medicines (both available in oral formulation). The inclusion of these oral effective antifungal drugs in the essential list of medicines (EML) would help in increased availability of these agents in this part of the world and better prompt management of patients thereby reducing mortality. The widespread availability of these drugs would also stimulate more research to facilitate the development of better combination therapies. -

Make Progress with Wound Debridement
Advanced Wound Care Make Progress with Wound Debridement A discussion on necrotic tissue, the importance of removing necrotic tissue from the wound environment, methods of debridement, and the role of MediHoney® dressings. 1 1 MediHoney Wound and Burn Dressing Importance of Optimizing and Controlling the Wound Bed Environment A wound management plan should include a thorough wound assessment and selection of appropriate products to address the specific needs of the wound. Setting goal- oriented strategies to gain control over the wound environment will help get the wound back on track towards healing. Appropriate goals such as maintaining the Necrotic Tissue and Necrotic Burden Causes of Necrotic Burden LACK OF BLOOD FLOW OR DECREASED INFECTION AND BIOFILM physiologic wound environment (e.g., debridement, cleansing, prevention/management of infection)1-3, 10 and TISSUE PERFUSION An infection is the presence of replicating microorganisms Necrotic or avascular tissue is the result of an inadequate blood SKIN FAILURE providing systemic support (e.g., edema reduction, nutrition, hydration) are the foundation to the process. Lack of blood flow or decreased tissue perfusion may be caused invading wound tissue and causing damage to the tissue and supply to the tissue in the wound area. It contains dead cells and Skin failure happens when skin and underlying tissue die because 1-3 by occlusion, vasoconstriction, venous hypertension, hypotension, the host. Biofilms are created by colonies of bacteria attached When necrotic tissue is present, there are a number of related factors that could be the root cause of delayed healing: debris that is a consequence of the dying cells. -

Description of Eschar-Associated Rickettsial Diseases Using Passive Surveillance Data — United States, 2010–2016
Morbidity and Mortality Weekly Report Description of Eschar-Associated Rickettsial Diseases Using Passive Surveillance Data — United States, 2010–2016 Naomi Drexler, MPH1; Kristen Nichols Heitman, MPH1; Cara Cherry, DVM1 Rickettsial eschars are necrotic lesions that occur at the site systems, and includes clinical details, diagnostic criteria, and of tick or mite bites and represent locations of primary inocula- patient outcomes. Since 2010, the CDC supplemental case tion of spotted fever group Rickettsia and Orientia species. In report form* has requested information on eschars. the United States, eschars are hallmarks of less severe spotted For this report, supplementary surveillance data collected fever diseases, including those caused by endemic agents such as by state and local health departments for illness with onset Rickettsia parkeri (1) and Rickettsia species 364D (2), as well as during 2010–2016 that were received and entered by CDC several imported agents, including Rickettsia africae, Rickettsia as of November 13, 2018, were summarized. TBRDs are not conorii, and Orientia tsutsugamushi. Eschars generally do not reportable conditions in Alaska and Hawaii, so no data from occur with Rocky Mountain spotted fever (RMSF), a poten- these states were included in this report. Case classifications tially deadly disease caused by Rickettsia rickettsii and have not were made according to the Council of State and Territorial been associated with Ehrlichia or Anaplasma species. The pres- Epidemiologists definitions (6,7). Confirmed cases were clini- ence of eschars can help differentiate less severe spotted fever cally compatible and had confirmatory diagnostic evidence rickettsioses from RMSF and clarify the potential contributions obtained by seroconversion (fourfold change) in anti-Ehrlichia, of each within surveillance data. -
Dermatology in the ER
DRUG ERUPTIONS and OTHER DISORDERS Lloyd J. Cleaver D.O. , F.A.O.C.D, F.A.A.D. Professor of Dermatology ATSU-Kirksville College of Osteopathic Medicine INTERNAL MEDICINE BOARD REVIEW COURSE I Disclosures No Relevant Financial Relationships DRUG ERUPTIONS Drug Reactions 3 things you need to know 1. Type of drug reaction 2. Statistics What drugs are most likely to cause that type of reaction? 3. Timing How long after the drug was started did the reaction begin? Clinical Pearls Drug eruptions are extremely common Tend to be generalized/symmetric Maculopapular/morbilliform are most common Best Intervention: Stop the Drug! Do not dose reduce Completely remove the exposure How to spot the culprit? Drug started within days to a week prior to rash Can be difficult and take time Tip: can generally exclude all drugs started after onset of rash Drug eruptions can continue for 1-2 weeks after stopping culprit drug LITT’s drug eruption database Drug Eruptions Skin is one of the most common targets for drug reactions Antibiotics and anticonvulsants are most common 1-5% of patients 2% of all drug eruptions are “serious” TEN, DRESS More common in adult females and boys < 3 y/o Not all drugs cause eruptions at same rate: Aminopenicillins: 1.2-8% of exposures TMP-SMX: 2.8-3.7% NSAIDs: 1 in 200 Lamotrigine: 10% Drug Eruptions Three basic rules 1. Stop any unnecessary medications 2. Ask about non-prescription medications Eye drops, suppositories, implants, injections, patches, vitamin and health supplements, friend’s medications