Contents Editor-In-Chief Dr
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effects of Selexipag and Its Active Metabolite in Contrasting The
Cutolo et al. Arthritis Research & Therapy (2018) 20:77 https://doi.org/10.1186/s13075-018-1577-0 RESEARCH ARTICLE Open Access Effects of selexipag and its active metabolite in contrasting the profibrotic myofibroblast activity in cultured scleroderma skin fibroblasts Maurizio Cutolo1*, Barbara Ruaro1, Paola Montagna1, Renata Brizzolara1, Emanuela Stratta2, Amelia Chiara Trombetta1, Stefano Scabini2, Pier Paolo Tavilla3, Aurora Parodi3, Claudio Corallo4, Nicola Giordano4, Sabrina Paolino1, Carmen Pizzorni1, Alberto Sulli1, Vanessa Smith5 and Stefano Soldano1 Abstract Background: Myofibroblasts contribute to fibrosis through the overproduction of extracellular matrix (ECM) proteins, primarily type I collagen (COL-1) and fibronectin (FN), a process which is mediated in systemic sclerosis (SSc) by the activation of fibrogenic intracellular signaling transduction molecules, including extracellular signal-regulated kinases 1 and 2 (Erk1/2) and protein kinase B (Akt). Selexipag is a prostacyclin receptor agonist synthesized for the treatment of pulmonary arterial hypertension. The study investigated the possibility for selexipag and its active metabolite (ACT-333679) to downregulate the profibrotic activity in primary cultures of SSc fibroblasts/myofibroblasts and the fibrogenic signaling molecules involved. Methods: Fibroblasts from skin biopsies obtained with Ethics Committee (EC) approval from patients with SSc, after giving signed informed consent, were cultured until the 3rd culture passage and then either maintained in normal growth medium (untreated cells) or independently treated with different concentrations of selexipag (from 30 μMto 0.3 μM) or ACT-333679 (from 10 μMto0.1μM) for 48 h. Protein and gene expressions of α-smooth muscle actin (α-SMA), fibroblast specific protein-1 (S100A4), COL-1, and FN were investigated by western blotting and quantitative real-time PCR. -

Effect of Prostanoids on Human Platelet Function: an Overview
International Journal of Molecular Sciences Review Effect of Prostanoids on Human Platelet Function: An Overview Steffen Braune, Jan-Heiner Küpper and Friedrich Jung * Institute of Biotechnology, Molecular Cell Biology, Brandenburg University of Technology, 01968 Senftenberg, Germany; steff[email protected] (S.B.); [email protected] (J.-H.K.) * Correspondence: [email protected] Received: 23 October 2020; Accepted: 23 November 2020; Published: 27 November 2020 Abstract: Prostanoids are bioactive lipid mediators and take part in many physiological and pathophysiological processes in practically every organ, tissue and cell, including the vascular, renal, gastrointestinal and reproductive systems. In this review, we focus on their influence on platelets, which are key elements in thrombosis and hemostasis. The function of platelets is influenced by mediators in the blood and the vascular wall. Activated platelets aggregate and release bioactive substances, thereby activating further neighbored platelets, which finally can lead to the formation of thrombi. Prostanoids regulate the function of blood platelets by both activating or inhibiting and so are involved in hemostasis. Each prostanoid has a unique activity profile and, thus, a specific profile of action. This article reviews the effects of the following prostanoids: prostaglandin-D2 (PGD2), prostaglandin-E1, -E2 and E3 (PGE1, PGE2, PGE3), prostaglandin F2α (PGF2α), prostacyclin (PGI2) and thromboxane-A2 (TXA2) on platelet activation and aggregation via their respective receptors. Keywords: prostacyclin; thromboxane; prostaglandin; platelets 1. Introduction Hemostasis is a complex process that requires the interplay of multiple physiological pathways. Cellular and molecular mechanisms interact to stop bleedings of injured blood vessels or to seal denuded sub-endothelium with localized clot formation (Figure1). -

Nanosuspensions of Selexipag: Formulation, Characterization, and in Vitro Evaluation Rusul M
Iraqi J Pharm Sci, Vol.30(1) 2021 Selexipag nanosuspension DOI : https://doi.org/10.31351/vol30iss1pp144-153 Nanosuspensions of Selexipag: Formulation, Characterization, and in vitro Evaluation Rusul M. Alwan*,1 and Nawal A. Rajab** * Ministry of Health and Environment, Najaf Health Department, Najaf, Iraq. **Department of Pharmaceutics, College of Pharmacy, University of Baghdad, Baghdad, Iraq. Abstract Selexipag(SLP) is an orally selective long-acting prostacyclin receptor agonist indicated for pulmonary arterial hypertension treatment. It is practically insoluble in water (class II, according to BCS). This work aims to prepare and optimize Selexipag nanosuspensions (SLPNS) to enhance the saturation solubility and in vitro dissolution rate. The solvent antisolvent precipitation method was used for the production of NS, and the effect of formulation parameters (stabilizer type, drug: stabilizer ratio, and use of co-stabilizer) and process parameter (stirring speed) on the particle size (P.S) and polydispersity index (PDI) were studied. The result revealed that the P.S of all prepared SLPNS formulation was in the nanometer range, except for the formulas that stabilized by Poloxamer. The optimal SLPNS (F15), which is stabilized by Soluplus® (SLP: stabilizer ratio 1:2) and prepared at a stirring speed of 1000 rpm, showed the smallest P.S and appropriate PDI, which are 47 nm and 0.073. The formula F5 exhibits 136 folds, an increase in the saturation solubility, and an enhancement in the dissolution rate in phosphate buffer pH 6.8 (100% drug release during 60 min) compared to the pure drug. This result indicates that SLPNS is an efficient way for improving the saturation solubility and the dissolution rate of SLP. -

Formulation and Optimization of Lyophilized Selexipag Nanocrystals to Improve the Saturation Solubility and Dissolution Rate
Sys Rev Pharm 2020;11(11):596-605 A multifaceted review journal in the field of pharmacy Formulation and Optimization of Lyophilized Selexipag Nanocrystals to Improve the Saturation Solubility and Dissolution Rate Rusul M. Alwana*, Nawal A. Rajab, Areej W. Alhagiesac a* b Ministry of Health and Environment, Najaf health department, Najaf, Iraq. c Department of Pharmaceutics, College of Pharmacy, University of Baghdad, Baghdad, Iraq * Department of Pharmaceutics, College of Pharmacy, University of Kufa, Najaf, Iraq Corresponding author Email: [email protected] Phone number: 07831480928 Abstract Selexipag is first in class orally active, selective non- Keywords: Selexipag, Nanocrystal, nanosuspension, prostanoid prostacyclin receptor agonist with a long half- Selexipag nanocrystals. life. It has low oral bioavailability due to a poor dissolution rate, which is considered a rate-limiting step for drug absorption. Nanocrystals (NCs) formulation is an attractive approach for enhancing the poorly soluble drug's saturation solubility and dissolution rate. They offer the advantages of crystalline state, high drug loading capacity, and simple preparation method. This study aims to prepare and characterize Selexipag NCs, filled in hard gelatin capsule in attempt to improve its solubility and dissolution rate. The effect of stabilizer type and preparation methods on the NC particle size and polydispersity index were evaluated to select the most stable formula. The results revealed that the formula (F7) prepared by the solvent antisolvent precipitation with the ultrasonication method (which contain SLX: Soluplus® at a ratio of 1:2) has the smallest mean particle size (38.5 nm) and appropriate polydispersity index (0.12); hence it was selected as the optimal formula. -

Club Health Assessment for District 306 A1 Through May 2013
Club Health Assessment for District 306 A1 through May 2013 Status Membership Reports Finance LCIF Number of YTD Member Avg. length of Months Yrs. Since Months Donations Times on Status Current YTD YTD YTD Net Count 12 service Since Last No Since Last for current Club Club Charter Current Quo within 2 Member Members Members Net Growth% Months for dropped Last Officer President Active Activity Account Fiscal Number Name Date Status * years Count Added Dropped Growth Ago members MMR *** Report Rotation Email ** Report *** Balance Year If below If net loss If no report When Number Notes the If no report 15 is greater in 3 more than of officers that in 12 members than 20% months one year repeat do not have months appears appears appears in appears in terms an active appears in in red in red red red indicated Email red Clubs less than two years old 118121 AMBALANGODA CREATORS 10/24/2012 Active 22 22 0 22 100.00% 0 7 N/R 116852 BENTOTA INNER CIRCLE 05/15/2012 Cancelled(8) 1 0 0 20 -20 -100.00% 20 1 5 None N/A 90+ Days 116241 BENTOTA MID-TOWN 03/05/2012 Active 24 8 4 4 20.00% 20 0 0 5 90+ Days 118152 COLOMBO NEW 11/15/2012 Active 20 20 0 20 100.00% 0 2 N/R GENERATION 116948 DEHIWALA MOUNT LAVINIA 05/29/2012 Active 32 14 3 11 52.38% 21 0 2 2 T 7 MID CITY 117766 DHARGA TOWN UNITED 09/11/2012 Active 27 27 0 27 100.00% 0 0 M 1 CREATORS 116949 MORAGALLA METRO 05/22/2012 Active 36 3 0 3 9.09% 33 0 2 P,T,M N/R 90+ Days 116174 MORATUMULLA MID TOWN 02/24/2012 Active 1 20 7 7 0 0.00% 20 1 0 S,T 7 118886 MORATUWA 04/10/2013 Newly Chartered 22 22 0 22 100.00% -
Report on Investigation Results
Pharmaceuticals and Medical Devices Agency This English version is intended to be a reference material for the convenience of users. In the event of inconsistency between the Japanese original and this English translation, the former shall prevail. Report on Investigation Results March 16, 2020 Pharmaceuticals and Medical Devices Agency I. Summary of drug [Brand name] See Appendix 1 [Non-proprietary name] See Appendix 1 [Approval holder] See Appendix 1 [Indications] See Appendix 1 [Dosage and administration] See Appendix 1 [Investigation office] Office of Pharmacovigilance I II. Investigation background Selexipag, clopidogrel sulfate (hereinafter referred to as “clopidogrel”), and clopidogrel/aspirin are approved for marketing with the indications and dosage and administration stated in Appendix 1. As it was considered appropriate to contraindicate the co-administration of selexipag and preparations containing clopidogrel based on the following information obtained on selexipag and preparations containing clopidogrel after their commercial launch, each package insert contains the precaution for the co-administration of these drugs in the CONTRAINDICATIONS and Contraindications for Co-administration sections. An overseas clinical study (AC-065-113 Study) was conducted to investigate the effects on pharmacokinetics of selexipag and its active metabolite (MRE-269) in healthy adults when selexipag was co-administered with gemfibrozil, a strong CYP2C8 inhibitor. As a result, Cmax and AUC0-∞ of selexipag increased by 1.4-fold and 2.0-fold, respectively, while Cmax and AUC0-∞ of MRE-269 increased by 3.6-fold and 11-fold, respectively when selexipag was co-administered with gemfibrozil compared to those when the drug was administered alone.1 The results exceeded the changes in exposure of selexipag and MRE-269 when CYP2C8 was inhibited estimated at the marketing-approval review 1 Bruderer S, et al. -

AHRQ Healthcare Horizon Scanning System – Status Update
AHRQ Healthcare Horizon Scanning System – Status Update Horizon Scanning Status Update: January 2014 Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA290201000006C Prepared by: ECRI Institute 5200 Butler Pike Plymouth Meeting, PA 19462 January 2014 Statement of Funding and Purpose This report incorporates data collected during implementation of the Agency for Healthcare Research and Quality (AHRQ) Healthcare Horizon Scanning System by ECRI Institute under contract to AHRQ, Rockville, MD (Contract No. HHSA290201000006C). The findings and conclusions in this document are those of the authors, who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. A novel intervention may not appear in this report simply because the System has not yet detected it. The list of novel interventions in the Horizon Scanning Status Update Report will change over time as new information is collected. This should not be construed as either endorsements or rejections of specific interventions. As topics are entered into the System, individual target technology reports are developed for those that appear to be closer to diffusion into practice in the United States. A representative from AHRQ served as a Contracting Officer’s Technical Representative and provided input during the implementation of the horizon scanning system. AHRQ did not directly participate in the horizon scanning, assessing the leads or topics, or provide opinions regarding potential impact of interventions. -
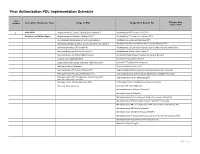
Prior Authorization PDL Implementation Schedule
Prior Authorization PDL Implementation Schedule Item Effective Date: Number Descriptive Therapeutic Class Drugs on PDL Drugs which Require PA July 1, 2018 1 ADD/ADHD Amphetamine Salt Combo Tablet (Generic Adderall®) Amphetamine ODT (Adzenys® XR ODT) Stimulants and Related Agents Amphetamine Salt Combo ER (Adderall XR®) Amphetamine ER Suspension (Adzenys ER®) Atomoxetine Capsule (Generic; Authorized Generic) Amphetamine Suspension (Dyanavel XR®) Dexmethylphenidate (Generic; Authorized Generic of Focalin®) Amphetamine/Dextroamphetamine XR Capsule (Mydayis ER®) Dexmethylphenidate ER (Focalin XR®) Amphetamine Salt Combo ER (Generic; Authorized Generic for Adderall XR) Dextroamphetamine Solution (Procentra®) Amphetamine Sulfate Tablet (Evekeo®) Dextroamphetamine Sulfate Tablet (Generic) Armodafinil Tablet (Generic; Authorized Generic; Nuvigil®) Guanfacine ER Tablet (Generic) Atomoxetine Capsule (Strattera®) Lisdexamfetamine Capsule, Chewable Tablet (Vyvanse®) Clonidine ER Tablet (Generic; Kapvay®) Methylphenidate IR (Generic) Dexmethylphenidate (Focalin®) Methylphenidate ER Chew (Quillichew ER®) Dexmethylphenidate XR (Generic; Authorized Generic for Focalin XR) Methylphenidate ER Capsule (Metadate CD®) Dextroamphetamine Sulfate Capsule ER (Generic; Dexedrine®Spansule) Methylphenidate ER Tablet (Generic; Generic Concerta®; Dextroamphetamine IR Tablet (Zenzedi®) Authorized Generic Concerta®) Methylphenidate ER Susp (Quillivant XR®) Dextroamphetamine Solution (Generic for Procentra®) Modafinil Tablet (Generic) Guanfacine ER Tablet (Intuniv®) Methamphetamine -

Non-Steroidal Anti-Inflammatories
PDL Drug Class Review Announcement October 5, 2021 Drug Classes to be reviewed: Non-Steroidal Anti-Inflammatories (NSAIDs) (Oral & Non-Oral); Antibiotics, Inhaled; Anti-Herpetic Agents (Oral & Topical); Fluoroquinolones, Oral; Hepatitis C Virus Treatments (Direct Acting Antivirals & Ribavirin Products); Human Immunodeficiency Virus (HIV) Agents, Oral; Pulmonary Arterial Hypertension Therapies (Phosphodiesterase Inhibitors, Endothelin Antagonists, Prostanoids, Guanylate Cyclase Stimulator); Newer Generation Antidepressants; Monoamine Oxidase Inhibitors (MAOIs); Tricyclic Antidepressants (TCAs); Triptans and Other Migraine Agents (Oral & Non-Oral); Anti-Psoriatics (Oral & Topical); Topical Immunomodulators; Topical Steroids (Low, Medium, High, & Very High Potency); Antiemetics (Oral & Non-Oral); H. Pylori Treatments; Pancreatic Enzymes; Proton Pump Inhibitors; Non- Biologic Ulcerative Colitis Agents (Oral & Rectal); Immune Globulins; Newer Generation Antihistamines; Antihistamine/Decongestant Combinations; Intranasal Rhinitis Agents; Leukotriene Modifiers; Methotrexate Products; Targeted Immune Modulators; Epinephrine Products; Newer Hereditary Angioedema Agents; Antihyperuricemics; Respiratory Agents [Anticholinergics & Combinations, Beta-2 Agonists (Short & Long), Corticosteroids & Combinations, Phosphodiesterase Inhibitors]. These drug classes will be reviewed at the October 5th, 2021 P&T Committee meeting from 1-5pm. The meeting will be held virtually. Dossiers and Supplemental Rebate offers are due to Magellan by September 7, 2021. -

Queensland Health List of Approved Medicines
Queensland Health List of Approved Medicines Drug Form Strength Restriction abacavir * For use in accord with PBS Section 100 indications * oral liquid See above 20 mg/mL See above tablet See above 300 mg See above abacavir + lamivudine * For use in accord with PBS Section 100 indications * tablet See above 600 mg + 300 mg See above abacavir + lamivudine + * For use in accord with PBS Section 100 indications * zidovudine tablet See above 300 mg + 150 mg + 300 mg See above abatacept injection 250 mg * For use in accord with PBS Section 100 indications * abciximab (a) Interventional Cardiologists for complex angioplasty (b) Interventional and Neuro-interventional Radiologists for rescue treatment of thromboembolic events that occur during neuroendovascular procedures. * Where a medicine is not TGA approved, patients should be made fully aware of the status of the medicine and appropriate consent obtained * injection See above 10 mg/5 mL See above abiraterone For use by medical oncologists as per the PBS indications for outpatient and discharge use only tablet See above 250 mg See above 500 mg See above acamprosate Drug and alcohol treatment physicians for use with a comprehensive treatment program for alcohol dependence with the goal of maintaining abstinence. enteric tablet See above 333 mg See above acarbose For non-insulin dependent diabetics with inadequate control despite diet; exercise and maximal tolerated doses of other anti-diabetic agents tablet See above 50 mg See above 100 mg See above acetazolamide injection 500 mg tablet 250 mg acetic acid ear drops 3% 15mL solution 2% 100mL green 3% 1 litre 6% 1 Litre 6% 200mL Generated on: 30-Aug-2021 Page 1 of 142 Drug Form Strength Restriction acetylcysteine injection For management of paracetamol overdose 2 g/10 mL See above 6 g/30 mL See above aciclovir cream Infectious disease physicians, haematologists and oncologists 5% See above eye ointment For use on the advice of Ophthalmologists only. -

Prostacyclin: an Inflammatory Paradox
REVIEW ARTICLE published: 13 May 2011 doi: 10.3389/fphar.2011.00024 Prostacyclin: an inflammatory paradox Jeremiah Stitham, Charles Midgett, Kathleen A. Martin and John Hwa* Section of Cardiovascular Medicine, Department of Internal Medicine, Yale School of Medicine, Yale University, New Haven, CT, USA Edited by: Prostacyclin (PGI2) is a member of the prostaglandin family of bioactive lipids. Its best- Angel Lanas, University of Zaragoza, characterized role is in the cardiovascular system, where it is released by vascular endothelial cells, Spain serving as a potent vasodilator and inhibitor of platelet aggregation. In recent years, prostacyclin Reviewed by: Emer Smyth, University of (PGI2) has also been shown to promote differentiation and inhibit proliferation in vascular smooth Pennsylvania, USA muscle cells. In addition to these well-described homeostatic roles within the cardiovascular Steven W. Kerrigan, Royal College of system, prostacyclin (PGI2) also plays an important role as an inflammatory mediator. In this Surgeons in Ireland, Ireland review, we focus on the contribution of prostacyclin (PGI2) as both a pathophysiological mediator *Correspondence: and therapeutic agent in three major inflammatory-mediated disease processes, namely John Hwa, Section of Cardiovascular Medicine, Department of Internal rheumatoid arthritis, where it promotes disease progression (“pro-inflammatory”), along Medicine, Yale School of Medicine, with pulmonary vascular disease and atherosclerosis, where it inhibits disease progression Cardiovascular Research Center, 300 (“anti-inflammatory”). The emerging role of prostacyclin (PGI2) in this context provides new George Street, Room 759H, New opportunities for understanding the complex molecular basis for inflammatory-related diseases, Haven, CT 06511, USA. e-mail: [email protected] and insights into the development of current and future anti-inflammatory treatments. -

In the High Court of Karnataka, Bangalore
1 R IN THE HIGH COURT OF KARNATAKA, BANGALORE DATED THIS THE 24TH DAY OF JUNE, 2014 BEFORE THE HON'BLE MR.JUSTICE RAM MOHAN REDDY W.P.Nos.22422 – 22512/2014 & 24164 – 24401/2014 & 24402 – 24891/2014 c/w W.P.Nos.22513 – 22557/2014 & 24962 – 25321/2014 & W.P.Nos.22087 – 22108/2014 & 22583 – 22758/2014 (EXCISE) IN W.P.Nos.22422 – 22512 & 24164 – 24401 & 24402 – 24891/2014: BETWEEN: 1. M/S K.T MEHARWADE AND COMPANY A PARTNERSHIP FIRM, CL-9 LICENSEE, CTS NO. 1928, OPPOSITE TO APMC YARD, PLOT NO.2, WARD NO.3, AMARGOL, HUBLI-580020, DHARWAD DISTRICT, REP. BY ITS PARTNER T.M. MEHARWADE 2. M/S AMRUT BAR AND RESTAURANT A PARTNERSHIP FIRM, CL-9 LICENSEE, CTS NO.4808, GOKUL ROAD, HUBLI 580020, DHARWAD DISTRICT, REP. BY ITS PARTNER SHRI VINAYAK P AKALWADI 3. M/S. SILLY POINT A PARTNERSHIP FIRM, CL-2 LICENSEE, CTS NO. 2927/A/B, STALL NO.1, BYLAPPANAVARA NAGAR, AKSHAYA APARTMENT, HUBLI 580020, DHARWAD DISTRICT, REP BY ITS PARTNER SURYAKANTH M HABEEB 2 4. SHRI M.M HABIB S/O MURARSA HABIB, AGED ABOUT 48 YEARS, CL-9 LICENSEE, CTS NO. 3445/B SIDDHESHWARA NAGARA, UNAKAL HUBLI 580020, DHARWAD DISTRICT 5. M/S. SHRINGARA WINES A PARTNERSHIP FIRM, CL-9 LICENSEE CTS NO. 2733, 2734, STATION ROAD, HUBLI 580020, DHARWAD DISTRICT REP. BY ITS PARTNER VINOD M. DHARMADAS 6. M/S. SHRINGARA BAR A PARTNERSHIP FIRM, CL-9 LICENSEE CTS NO. 2772 TO 2775/1B, STATION ROAD, HUBLI 580020 DHARWAD DISTRICT REP BY ITS PARTNER T.G DHARMADAS 7.