Kick ASS Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Altering Cell Death Pathways As an Approach to Cure HIV Infection
Citation: Cell Death and Disease (2013) 4, e718; doi:10.1038/cddis.2013.248 OPEN & 2013 Macmillan Publishers Limited All rights reserved 2041-4889/13 www.nature.com/cddis Review Altering cell death pathways as an approach to cure HIV infection AD Badley*,1,2, A Sainski2,3, F Wightman4,5 and SR Lewin4,5 Recent cases of successful control of human immunodeficiency virus (HIV) by bone marrow transplant in combination with suppressive antiretroviral therapy (ART) and very early initiation of ART have provided proof of concept that HIV infection might now be cured. Current efforts focusing on gene therapy, boosting HIV-specific immunity, reducing inflammation and activation of latency have all been the subject of recent excellent reviews. We now propose an additional avenue of research towards a cure for HIV: targeting HIV apoptosis regulatory pathways. The central enigma of HIV disease is that HIV infection kills most of the CD4 T cells that it infects, but those cells that are spared subsequently become a latent reservoir for HIV against which current medications are ineffective. We propose that if strategies could be devised which would favor the death of all cells which HIV infects, or if all latently infected cells that release HIV would succumb to viral-induced cytotoxicity, then these approaches combined with effective ART to prevent spreading infection, would together result in a cure for HIV. This premise is supported by observations in other viral systems where the relationship between productive infection, apoptosis resistance, and the development of latency or persistence has been established. Therefore we propose that research focused at understanding the mechanisms by which HIV induces apoptosis of infected cells, and ways that some cells escape the pro-apoptotic effects of productive HIV infection are critical to devising novel and rational approaches to cure HIV infection. -

2017-2021 Integrated HIV Prevention and Care Plan
Marin, San Francisco, & San Mateo Counties, California 2017–2021 INTEGRATED HIV PREVENTION AND CARE PLAN SEPTEMBER 30, 2016 1 Marin, San Francisco, & San Mateo Counties, California 2017–2021 INTEGRATED HIV PREVENTION AND CARE PLAN TABLE OF CONTENTS Page # Five-Year HIV Goals & Objectives for the San Francisco Region 3 San Francisco HIV Community Planning Council Roster 5 Letters of Concurrence 6 Section I: Needs Assessment 9 A. Epidemiologic Overview 10 B. HIV Care Continuum 22 C. Financial & Human Resources Inventory 28 D. Assessing Needs, Gaps, & Barriers 63 E. Data: Access, Systems, & Sources 72 Section II. Integrated HIV Prevention & Care Plan 77 A. Integrated HIV Prevention and Care Action Plan 78 B. Collaborations, Partnerships, and Stakeholder Involvement 101 C. People Living with HIV & Community Engagement 104 Section III. Monitoring & Improvement 109 2 FIVE-YEAR GOALS & OBJECTIVES Goal # 1: Reduce New HIV Infections in the San Francisco Region Objective # 1.1: By December 31, 2021, increase the percentage of people living with HIV who know their serostatus to at least 96%. Objective # 1.2: By December 31, 2021, reduce the number of annual new HIV diagnoses by at least 50%. Objective # 1.3: By December 31, 2021, increase the utilization of pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) among high-risk HIV-negative persons by at least 50%, based on base- line data to be identified over the course of the Plan. Goal # 2: Increase Access to Care and Improve Health Outcomes for Persons Living with HIV in the San Francisco Region Objective # 2.1: By December 31, 2021, increase the percentage of annual newly diagnosed persons linked to HIV medical care within one month of HIV diagnosis to at least 90%. -

The Importance of Community Engagement in Hiv Cure Research
tagline Vol. 26, No. 1, May 2019 SCIENTIFIC COMPLEXITY AND ETHICAL UNCERTAINTIES: THE IMPORTANCE OF COMMUNITY ENGAGEMENT IN HIV CURE RESEARCH By Richard Jefferys Introduction The past decade has seen a major expansion of the research Recent presentations at the March 2019 CROI indicate that effort to develop a cure for HIV infection. The U.S. National two additional people may have joined Brown,6,7 but follow-up Institutes of Health (NIH), the world’s largest biomedical is far shorter: One of the individuals has been off ART without research funder, has identified the pursuit of a cure as one of evidence of HIV rebound for 18 months, while the other is at five primary priorities for HIV.1 Total global financial support about four months. increased substantially in the period 2012–2017, from $88 million to $288.8 million.2 In 2014, TAG launched an online Translating to a Wider Community listing of cure-related clinical research drawn from registries (primarily ClinicalTrials.gov). The list initially contained less These additional cases of possible cures are encouraging, than 50 entries; it currently includes 98 clinical trials and 34 but the method used to achieve this outcome cannot be observational studies that are ongoing.3 Over 7,000 people used in most people with HIV, who do not require stem cell are expected to enroll in these studies. transplants for cancer (the high mortality risk associated with transplantation precludes its use outside of this setting). As with other areas of HIV research, engagement of the community of people living with HIV and their advocates is In the absence of any known safe alternatives for obtaining vital for ensuring that the conduct of cure-related studies is similarly robust depletion of HIV from the body, investigators ethical, appropriate, and responsive to community priorities. -

AIDS Office SFDPH.Tif
:;J . AIDS Office ofthe San Francisco Department ofPublic Health - Records (MSS 95-01) 1982 - 1994 66 cubic feet The AIDS Office (AO)ofthe San Francisco Department ofPublic Health (SFDPH) is responsible for all non acute AIDS activities administered by the city. This includes surveillance, research, administration and oversight ofmuch ofthe city, state and federal funding ofAIDS related services, the coordination ofnon-acute care services for PWAs and HIV+ people, the coordination ofAIDS education and prevention programs, and planning and policy development related to AIDS for the city. Infonnation the AO collects is also passed on to appropriate state and federal offices (CDC, Nlli, etc) to help them understand what is occurring with AIDS and AIDS-related services in San Francisco. The responsibilities and activities ofeach branch ofthe AO and the duties ofindividual staffare described in the "Resource Directory" located in the folder marked "History and Description ofthe AIDS Office" located at the beginning ofCarton 1. Historical Sketch The initial response to the AIDS epidemic by the San Francisco Department ofPublic Health (SFDPH) was centered in the Bureau ofEpidemiology andDisease Control, which, until 1985, was the site ofmost AIDS related surveillance operations within San Francisco. In addition, in 1984 the AIDSActivities Office was fonned to identify needs, address health education, and arrange for funding ofAIDS-related services in San Francisco, with JeffAmory, Michael Bala and Gary Titus as the initial staff AIDS-related policy development and planning has also been done within the office ofthe Director ofPublic Health. Mervyn Silvennan was Director during the first halfofthe 1980s, handling numerous explosive issues such as the bathhouse dispute of 1984. -

G HIV/AIDS & Immune Evasion Strategies the Year 1981…
Micro 320: Infectious Disease & Defense HIV/AIDS & Immune Evasion Strategiesg Wilmore Webley Dept. of Microbiology The Year 1981… Reported by MS Gottlieb, MD, HM Schanker, MD, PT Fan, MD, A Saxon, MD, JD Weisman, DO, Div of Clinical Immunology-Allergy; Dept of Medicine, UCLA School of Medicine; I Pozalski, MD, Cedars-Mt. Siani Hospital, Los Angeles; Field services Div, Epidemiology Program Office, CDC. First Encounter: Dr. Michael Gottleib http://www.pbs.org/wgbh/pages/frontline/aids/view/ What is AIDS? Acquired Immune Deficiency Syndrome • Acquired means you can get infected with it (not inherited) • Immune Deficiency means a weakness in the body's system that fights diseases. • Syndrome means a group of health problems that make up a disease. The term AIDS refers to an advanced stage of HIV infection, when the immune system has sustained substantial damage. Not everyone who has HIV infection develops AIDS http://www.pbs.org/wgbh/pages/fro ntline/aids/view/ Global Statics of HIV/AIDS Transmission of HIV “Patient Zero” and HIV Transmission Gaëtan Dugas: A Canadian who worked for Air Canada as a flight attendant Claimed to have had over 2,500 sexual partners across North America 1972 Diagnosed with Kaposi's Sarcoma in June 1980 In 1982 the CDC linked him to 9 of the first 19 cases in Los Born February 20, 1953 Angeles, 22 cases in NYC and 9 March 30, 1984 Died (aged 31) more in 8 other cities – Total of 40 Quebec City, Quebec of the first 248 cases in the U.S. Occupation Flight attendant New Model: HIV Traveled to Haiti, Then U.S. -

Where's the Cure?
A QUARTERLY JOURNAL ON HIV PREVENTION, TREATMENT AND POLITICS VOLUME 5, NO. 3 acHIeVe INSIDE Personal Perspective: CHANGING MY GENES 6 Where’s Being part of something as big as the search for the cure is a humbling experience. INCHING The TOWARD A VACCINE 9 The past two years Cure? have seen discover- ies that give hope that it may be possible to find an effective vaccine. THE FUTURE OF HIV PREVENTION 12 Three decades into the HIV epidemic, the A Look At Research number of new infections remains distress- ingly high. Across the U.S. HEPATITIS C: NEW DANGERS, that NIH granting procedures drastically NEW HOPES 16 by Stephen LeBlanc New information on slowed research and diverted money to transmission and a cure. university overhead costs, rather than to n 2009, Martin Delaney, a leading the search for a cure. Proponents esti- AIDS activist and the founder of Personal Perspective: mated a budget for the AIDS Cure Project Project Inform, co-authored an arti- MY FIGHT FOR A of $1.84 billion over five years. cle in Science calling for a new “HIV HEPATITIS C CURE 20 ICollaboratory” to focus on cure research. The Delaney Collaboratories The data on the new drug looked fabulous. The Collaboratory would be designed “to Nothing like the HIV Collaboratory or I thought, “I want this drug!” accelerate basic discovery and the clinical the AIDS Cure Project ever emerged, LOOKING BACK, translation of these discoveries.” Sadly, either in the amount of funding or in the LOOKING FOR- he died before the article was published. -

A Publication Such As Yours Is Not the Appropriate Vehicle for Teaching Hiv Prevention
"We believe that a publication such as yours is not the appropriate vehicle for teaching HiV prevention. Rather it encourages a free wheeling life style which helped bring this disease to the epidemic proportions we are now facing." Carol A. Hale, Executive Director Permian Basin AIDS Coalition, Odessa, Texas NOT SANITIZED FOR YOUR PROTECTION HIV Merit Badges, Inkblots ottHlbboas, Love Letter to Heuft, And Mueb More! YOUR CRANKY EDITOR & IRRESISTIBLE FORCE 21-yeai-old Carson Beowulf Thome Tutlio hails from sunny YOUR HUMPY EDITOR Southern California. & INTERNATIONAL LIAISON Write him. c/o DPN Tom Ace we're sure it'll make day. YOUR SLEAZY EDITRIX Wouldyou like to be a & PROTECTOR OF THE STREETS DPN lust object? You Michael Botkin know what to do. 'We've got to have some common sense about a YOUR GRACIOUS KEEPER disease transmitted by people deliberately engaging OF THE CAMERA In unnatural acts." —Sen. Jesse Helms (R-N C.) Mod Bob YOUR CRAFTY ARTIST & DEFENDER OF TRADITIONAL MEDIA KIra Od comm Page Jm Boy Carson Tuffio ^ ACCEPT NO SUBSTITUTES! Sfmzy Wisdom: Josso Helm Makes Me Sick 3 What to do Once You're Dead Diseased Pariah News Is a patently of¬ thy Tim Haggerty 6 fensive publication of, by, and for people i^rs to the BdSorfs) / with HIV disease (and their friends and A Love letter to $lewt by Paul Walker W loved ones). We are a forum for Infected Get Fat, DonWie! explores The Weil-Fed Welfare Queen 11 people to share their thoughts, feelings, Truly Tuttt Frultl Flies fry Lou Ceci 14 art, writing, and brownie recipes In an Inkblots by Glenn Gayford. -

2016 Annual Report
June 12, 2017 Dear Friend of TAG: I’m so proud to share with you Treatment Action Group’s 2016 Annual Report. As you will see, TAG’s passionately dedicated, deeply informed staff have been unstinting in their efforts to speed up research and high-quality prevention, treatment, and care programs for people living with HIV, hepatitis C virus (HCV), or tuberculosis (TB), and for those most at risk of acquiring these infections. Today, more than ever, TAG’s work is vital. We are living Ending the in an unprecedented political era. Every day brings a new outrage and gathering threats to our work promoting research, prevention, and treatment. Everything TAG has fought for over the past three decades to defeat HIV/AIDS and end the TB and HCV Epidemic epidemics is at risk. Our progress towards ending these epidemics with Progress in the Fight extremely effective new tools for prevention, treatment, and cures will be in vain if people don’t have comprehensive for Better Treatment, coverage to ensure access. TAG’s vital work needs your support now more than ever: a Vaccine, and a • TAG is leading community efforts to end AIDS as an 2016 epidemic in New York State by the close of 2020 by Cure for AIDS Annual strengthening HIV, STD, and sexual health programs for Report those most affected • TAG is expanding its Ending the Epidemic work to southern states where the HIV/AIDS epidemic continues at its worst • TAG is leading efforts to build on existing law and regulation to control drug costs • TAG is leading efforts to defend key National Institutes of Health AIDS research agencies and their budgets from brutal cuts proposed by the new administration • TAG is fighting efforts to greatly weaken the U.S. -

Item 3I. LBR-2016-17-027 Project Open Hand
SMALL BUSINESS COMMISSION CITYAND COUNTYOF SAN FRANCISCO M ARK DWIGHT, PRESIDENT EDWIN M. LEE, M AYOR REGINA D ICK-E NDRIZZI, D IRECTOR Legacy Business Registry Staff Report HEARING DATE DECEMBER 12, 2016 PROJECT OPEN HAND Application No.: LBR-2016-17-027 Business Name: Project Open Hand Business Address: 730 Polk Street District: District 6 Applicant: Mark Ryle, CEO Nomination Date: September 30, 2016 Nominated By: Supervisor Jane Kim Staff Contact: Richard Kurylo [email protected] BUSINESS DESCRIPTION Project Open Hand is a nonprofit organization based in the Tenderloin that provides free healthy meals, groceries, nutrition counseling and education, and social work services to senior citizens and critically ill community members. Historically, Project Open Hand was one of the first organizations to support gay men suffering from AIDS during a time when social services for AIDS victims were nonexistent. Its roots date to 1985 when founder Ruth Brinker was moved to feed her ailing neighbors suffering from AIDS. After three years of working out of her kitchen, Brinker was able to secure a space for the project in the basement of Trinity Episcopal Church at 1668 Bush Street, and in 1987, the organization purchased its first kitchen at 2720 17th Street. The organization incorporated as a nonprofit 501(c)(3) a few years later in 1991, after serving its 1 millionth meal. Today, Project Open Hand operates out of an architecturally significant four-story brick building at the southeast corner of Polk and Ellis streets, which it purchased in 1997. What began as preparing meals for her seven neighbors grew into a pioneering and influential organization that provides 2,500 meals and 200 bags of groceries per day to senior citizens and clients who battle a range of diseases and illnesses. -

Sharon Lewin
AIDS 2014 Key Media Coverage: HIV Cure 1 Key Media Coverage th 20 International AIDS Conference (AIDS 2014) Melbourne, Australia July 20-25, 2014 AIDS 2014 Key Media Coverage: HIV Cure 2 HIV Cure AIDS 2014. Melbourne, Australia A. Wire Reuters ............................................................................................................................................... 3 Bloomberg .......................................................................................................................................... 5 Agence France Press (AFP) .............................................................................................................. 10 Australian Associated Press (AAP) .................................................................................................. 12 Indo-Asian News Service ................................................................................................................. 13 B. Broadcast ABC RADIO ......................................................................................................................................... 18 9NEWS ............................................................................................................................................. 33 7NEWS ............................................................................................................................................. 33 C. Online media and blogs The Sydney Morning Herald ................................................................................................................. -
Aids Walk Statement
Dear AIDS Walk San Francisco Supporter, Thank you for being such an important part of AIDS Walk San Francisco (AWSF) and congratulations again on a very empowering and gratifying 2017 event, as well as on its success. We have an important announcement to share with you regarding the future of AWSF, and an invitation. Starting this year, the world's leading research organization on HIV and aging, ACRIA, will become the fiscal sponsor of AWSF. ACRIA will also join Project Open Hand (POH) and Positive Resource Center (PRC) as a lead co-beneficiary of the event. Since its formation in the summer of 2015, one of the top priorities of the AIDS Walk San Francisco Foundation (AWSFF) has been addressing the challenges facing older people living with HIV/AIDS. “Over the past two years, AWSFF is proud to have provided the sole funding to launch the Golden Compass Program at UCSF’s Ward 86, granting it a total of $175,000,” said Serafina Palandech, Board Chair of AWSFF. “In 2017, we were pleased to support the San Francisco AIDS Foundation (SFAF) with a grant of $15,000 for its HIV and aging program, The Elizabeth Taylor 50-Plus Network. In creating this opportunity for ACRIA, we are not only maintaining, but strengthening AWSF’s commitment to care for long-term survivors and older people living with HIV in the Bay Area.” “We are proud to usher in ACRIA to the helm of this much beloved and vital community event,” said Robert Mansfield, AWSFF Treasurer. “ACRIA’s leadership will bolster the fiscal stability of AWSF, enabling the Walk to focus less on sustaining solvency and more on ending HIV and AIDS. -
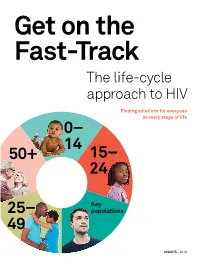
Get on the Fast-Track — the Life-Cycle Approach To
Get on the Fast-Track The life-cycle approach to HIV Finding solutions for everyone at every stage of life 0 – 14 50+ 1 5 – 24 Key 2 5 – populations 49 UNAIDS | 2016 2 contents 1 Foreword 3 2 Introduction 6 3 Children (0–14) 12 4 Young people (15–24) 28 5 Key populations throughout the life cycle 50 6 Adulthood (25–49) 72 7 Ageing (50+) 90 8 Conclusion 101 9 AIDS by the numbers 105 10 Annex on methods 133 2 foreword The scope of HIV prevention and treatment options has never been wider than it is today. The world now has the scientific knowledge and experience to reach people with HIV options tailored to their lives in the communities in which they live. This life-cycle approach to HIV ensures that we find the best solutions for people throughout their lifetime. And it begins with giving children a healthy start in life free from HIV. The progress made in reducing mother-to-child transmission of HIV is one of the remarkable success stories in global health. Antiretroviral medicines have averted 1.6 million new HIV infections among children since 2000. Even so, intensified efforts are needed to virtually eliminate transmis- sion from mother to child. Adolescence is a turbulent time, and a particularly dangerous time for young women living in sub-Saharan Africa. As they transition to adulthood, their risk of becoming infected with HIV increases dramatically. When women and girls are empowered, they have the means to protect themselves from becoming infected with HIV and to access HIV services.