Managing Latex Allergy in the Workplace
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genital Allergy C Sonnex
4 Sex Transm Infect: first published as 10.1136/sti.2003.005132 on 30 January 2004. Downloaded from REVIEW Genital allergy C Sonnex ............................................................................................................................... Sex Transm Infect 2004;80:4–7. doi: 10.1136/sti.2003.005132 Genital allergy should be considered as a possible Local responses consist of genital swelling, burning, irritation, or soreness which may occur diagnosis in all patients with genital soreness or irritation during or soon after intercourse, usually becom- for which no infection or dermatosis can be identified and ing maximal at 24 hours and lasting 2–3 days.45 in whom symptoms remain unchanged or worsen with Semen contact with non-genital skin may also give rise to localised itching and urticaria.67 treatment. Type I and IV hypersensitivity reactions are most Generalised reactions associated with semen commonly encountered and can be assessed by allergy include angioedema of the lips and performing skin prick testing/radioallergosorbent test eyelids,68 laryngeal oedema,9 bronchospasm,10 and anaphylaxis347 but, to date, death has not (RAST) or patch testing, respectively. Type IV reactions been reported. Semen allergy mainly affects (contact dermatitis) may sometimes prove difficult to younger women although postmenopausal cases distinguish clinically from an irritant dermatitis. This clinical are documented.11 12 An increasing intensity of reaction with subsequent episodes of coitus is a review attempts to summarise key features of genital common feature. Levine et al described a married allergy for the practising clinician. woman with a 15 year history of hay fever who ........................................................................... initially presented with swollen eyes, nasal congestion, and sneezing an hour after coitus. -
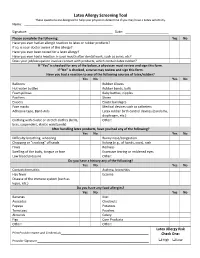
Latex Allergy Screening Tool These Questions Are Designed to Help Your Physician Determine If You May Have a Latex Sensitivity
Latex Allergy Screening Tool These questions are designed to help your physician determine if you may have a Latex sensitivity. Name: ____________________________________ __________ Signature: _________________________________ __________ Date: ______ _______________ Please complete the following: Yes No Have you ever had an allergic reaction to latex or rubber products? If so, is your doctor aware of this allergy? Have you ever been tested for a latex allergy? Have you ever had a reaction in your mouth after dental work, such as sores, etc? Does your job/occupation involve contact with products, which contain latex rubber? If “Yes” is checked for any of the below, a physician must review and sign this form. If “No” is checked, a nurse may review and sign this form. Have you had a reaction to any of the following sources of latex/rubber? Yes No Yes No Balloons Rubber Gloves Hot water bottles Rubber bands, balls Foam pillows Baby bottles, nipples Pacifiers Shoes Erasers Elastic bandages Face masks Medical devices such as catheters Adhesive tape, Band‐Aids Latex rubber birth control devices (condoms, diaphragm, etc.) Clothing with elastic or stretch clothes (belts, Other: bras, suspenders, elastic waistbands) After handling latex products, have you had any of the following? Yes No Yes No Difficulty breathing, wheezing Runny nose/congestion Chapping or “cracking” of hands Itching (e.g., of hands, eyes), rash Hives Redness Swelling of the body, tongue or face Excessive tearing or reddened eyes Low blood pressure Other: Do you have a history any of the following? Yes No Yes No Contact dermatitis Asthma, bronchitis Hay fever Eczema Disease of the immune system (such as lupus, etc.) Do you have any food allergies? Yes No Yes No Bananas Kiwi Avocados Chestnuts Papaya Potatoes Tomatoes Peaches Almonds Celery Figs Corn Products Other: Other: Latex Allergy Risk Print Provider Name and Credentials_________________________________________________ Check One: Provider Signature ______________________________________________________________ High Low . -

Latex Allergy/Student Effective Date: 1/1/10
OCHSNER CLINICAL SCHOOL POLICY Policy #: OCS 400.14 Title: Latex Allergy/Student Effective Date: 1/1/10 PURPOSE The purpose of this policy is to establish guidelines for the identification, follow-up and work practice modification for all OCS medical students with latex sensitivities or allergies to ensure a consistent safe workplace. Students will be classified in the category of Health Care Worker (HCW) on the Ochsner campuses. Health Care Workers with demonstrated latex sensitivity will be provided with engineering controls, protective apparel and other interventions that will minimize opportunities for development of a true latex allergy. HCW’s with a diagnosed latex allergy will be provided a latex safe environment to the extent possible. DEFINITIONS: Latex refers to natural rubber latex and includes products made from dry natural rubber. Natural rubber latex is the product manufactured from a milky fluid derived mainly from the rubber tree, Hevea brasiliensis. High-risk populations are groups known to have a higher risk for latex allergic reactions and include persons: • with occupational exposure to latex, • diagnosed with myelodysplasia, myeloma, congenital urologic abnormalities, or Spina bifida • with history of asthma, hay fever, contact dermatitis, or autoimmune disease (i.e. Lupus), • with food allergies such as bananas, avocados, potatoes, tomatoes, kiwi fruit, peaches, papaya, fruit or chestnuts and • who have exhibited contact dermatitis, itching or redness of the skin following the touching or wearing of latex products. Sensitization is the development of immunological memory in response to exposure to an antigen. Sensitivity is a clinical response that develops after sensitizations. Allergic reactions range from urticaria, rhinitis, conjunctivitis, angiodema, laryngeal edema, cardiovascular changes, GI upset, psychological distress, and bronchospasm, to severe life threatening anaphylaxis. -

Screening Tool
Natural Rubber Latex Allergy Patient Screening Questionnaire When patients are first being assessed, whether in out-patients, assessment clinics, admission or prior to any intervention in clinical settings, it is important that their allergic status is determined as far as is possible. This assessment tool should aid that process. 1. Initial Assessment i. Ask the patient if they have an allergy to any medicines, foods or other items ii. If the patient states that they have no allergies then treat as normal iii. If the patient states that they are allergic to any of the following, this should trigger additional questioning; balloons, contraceptives, rubber gloves, dental blocks, hot water bottles, erasers, rubber bands/balls, pillows, elastic dressing and bandages, elastic waistbands/underwear. iii. If the patient states that they are allergic to any of the following, this should trigger additional questioning; apples, avocados, bananas, celery, cherries, chestnuts, ficus, figs, grapes, kiwi, latex, mangoes, melons, passion fruit, peaches, pears, pistachios, potatoes, ragweed, strawberries, tomatoes. TREAT AS HIGH RISK 2. Further questions a. Ask the patient what symptoms they experience when they eat/touch the products listed above b. If the patient states any of the following symptoms, further questions should be asked; breathlessness, skin redness, chapping or cracking of hands, swelling of lips or tongue, runny nose, congestion, hives, itching. TREAT AS TYPE I 3. Assessment conclusion If the patient in addition to positive responses to the questions above, suffers from any of the following then treat as a high risk individual and follow the protocol; • Contact dermatitis • Spina bifida • Eczema • Multiple genitourinary • Asthma • Auto-immune disease (Lupus etc) • Hay fever TREAT AS TYPE I If the patient assessment results in a high-risk outcome, then label the patient’s notes and notify all others who may treat the patient. -

Egg Allergy: Diagnosis and Immunotherapy
International Journal of Molecular Sciences Review Egg Allergy: Diagnosis and Immunotherapy Dulashi Withanage Dona and Cenk Suphioglu * NeuroAllergy Research Laboratory (NARL), School of Life and Environmental Sciences, Faculty of Science, Engineering and Built Environment, Deakin University, 75 Pigdons Road, Geelong 3216 VIC, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-3-5227-2886 Received: 1 May 2020; Accepted: 14 July 2020; Published: 16 July 2020 Abstract: Hypersensitivity or an allergy to chicken egg proteins is a predominant symptomatic condition affecting 1 in 20 children in Australia; however, an effective form of therapy has not yet been found. This occurs as the immune system of the allergic individual overreacts when in contact with egg allergens (egg proteins), triggering a complex immune response. The subsequent instantaneous inflammatory immune response is characterized by the excessive production of immunoglobulin E (IgE) antibody against the allergen, T-cell mediators and inflammation. Current allergen-specific approaches to egg allergy diagnosis and treatment lack consistency and therefore pose safety concerns among anaphylactic patients. Immunotherapy has thus far been found to be the most efficient way to treat and relieve symptoms, this includes oral immunotherapy (OIT) and sublingual immunotherapy (SLIT). A major limitation in immunotherapy, however, is the difficulty in preparing effective and safe extracts from natural allergen sources. Advances in molecular techniques allow for the production of safe and standardized recombinant and hypoallergenic egg variants by targeting the IgE-binding epitopes responsible for clinical allergic symptoms. Site-directed mutagenesis can be performed to create such safe hypoallergens for their potential use in future methods of immunotherapy, providing a feasible standardized therapeutic approach to target egg allergies safely. -

What Is Natural Rubber Latex?
latex allergy latexallergy What is natural rubber latex? NATURAL RUBBER IS A HIGHLY PROCESSED PLANT PRODUCT FROM THE LATEX OF THE COMMERCIAL RUBBER TREE. ABOUT 90% IS PROCESSED FOR MANUFACTURE OF EXTRUDED RUBBER PRODUCTS, MOULDED GOODS OR PNEUMATIC TYRES. The remaining 10% is used for the manufacture of rubber gloves and other dipped products, such as condoms, swimming caps and balloons. Although there are traces of latex allergen in tyre dust, dipped rubber products are responsible for most allergic reactions. What is a latex allergy? A latex allergy is an allergy to products made from natural rubber latex. The allergy-causing particles become attached to the cornstarch powder in gloves, swimming caps and balloons. Moisture from the skin can enhance this process. The particles can become airborne and inhaled when products are used. Sensitized individuals react to these particles. Milk protein is sometimes mixed in with latex in surgical and household gloves and this can be the cause of reactions in milk allergic individuals. Who is at risk of a latex allergy? Adults and children most at risk are those with other allergies such as eczema, asthma and hayfever.Those who have regular contact with natural rubber latex such as powdered gloves or catheters are the most likely to become sensitized. What are the symptoms of a latex allergy? The reactions can be mild and cause rashes on the hands, itchy swollen eyes, runny nose and sneezing.An asthma attack can occur. latex allergy It is also possible to have a severe life threatening allergic reaction (anaphylactic shock).This is occurs when the latex particles come in contact with mucous membranes. -

Latex Allergy in the Hospital
Latex Allergy in the Hospital What is a latex allergy? Latex is found in a variety of products, from everyday household items to many articles used in routine medical and dental care. An allergic reaction to natural rubber latex is actually a reaction to a protein contained in the sap of the Brazilian rubber tree (Hevea brasiliensis). This sap is used in manufacturing latex products. Who is at risk to develop latex allergy? People with spina bifida Health care workers such as: doctors, nurses, surgical staff, dentists, dental hygienists, emergency medical services personnel, lab technicians People with other types of allergies or asthma People who have had many surgeries or medical procedures Rubber industry workers: those working in tire factories, rubber manufacturing and glove manufacturing What are some of the symptoms of latex allergy? Skin rash or itching (generally on the hands) Hives Swollen red skin Swollen lips and tongue with difficulty breathing, wheezing Shortness of breath Dizziness Fainting Abdominal (belly) pain Diarrhea UMHS Hospitals and Health Centers - 1 - In very rare cases people with a latex allergy may suffer an anaphylactic shock, a severe allergic reaction that may be life threatening. Symptoms of anaphylaxis shock include: Throat hoarseness or swelling Persistent wheezing Fainting Low blood pressure The risk of anaphylactic shock seems to be greatest in people who have had: Previous allergic reactions to products that contain latex. Prior anaphylaxis with an unknown cause. What is the treatment? Certain medications may reduce allergy symptoms but the most effective approach is to reduce exposure to latex products. How can I avoid exposure to latex in the hospital? Many hospital items and supplies contain latex. -

Latex Allergy and Foods Positioned Here SUB TITLECARE POSITIONED INSTRUCTIONS HERE
Title of article is Latex Allergy and Foods positioned here SUB TITLECARE POSITIONED INSTRUCTIONS HERE The foods listed in the chart below have shown to cause allergic reactions in some individuals with latex allergy. Reactions can occur because these foods contain a protein that resembles a protein in latex. If you have had an allergic reaction to any of these foods, you should avoid them in the future. Some allergists recommend that ALL persons with latex allergy should avoid the four foods with the *highest prevalence of reactions. During your hospitalization, avocado, banana, chestnut and kiwi will be omitted from your diet. Please be aware that as more research is done this list may change. LATEX RELATED FOODS *HIGH PREVALENCE OF Moderate Prevalence of Lower Prevalence of REACTION Reaction Reaction Avocado Apple Apricot Banana Carrot Cherry Chestnut Celery Coconut Kiwi Cherimoya Fig Melons Grapes Papaya Loquat Potato Mango Tomato Nectarine Nuts (all) Passion fruit Peach Pear Plum Swiss chard This information is not intended to diagnose health problems or to take the place of medical advice or care you receive from your physician or other health care professional. If you have persistent health problems, or if you have additional questions, please consult your doctor. If you have questions or need more information about your medication, please speak to your pharmacist. Kaiser Permanente does not endorse any brand names; any similar products may be used. Herbs and supplements are sold over-the-counter. Kaiser Permanente carries only herb categories for which some evidence exists to show that the herbs may be effective to treat certain medical conditions. -

Oral Allergy Syndrome
Oxford University Hospitals NHS Trust Children’s Allergy Clinic Oral allergy syndrome Information for parents What is oral allergy syndrome? • In the common form, oral allergy syndrome usually causes redness, itching, burning and swelling of the lips, inside of the mouth, tongue and soft palate. A child will often refuse the food once it starts irritating their mouth. • Occasionally itching and swelling of the throat occurs. Other reactions such as hives (similar to nettle rash), conjunctivitis (itchy, watery eyes), rhinitis (inflammation inside the nose), asthma, nausea and vomiting may occur later. • Severe symptoms such as anaphylactic shock or breathing problems are rare. What are the causes? • Oral allergy syndrome (OAS) is usually caused by an allergy to certain fruit and vegetables, especially when eaten raw. • Reactions to the same foods when they are cooked are less likely but can sometimes happen. The skin of certain fruit and vegetables can cause a reaction. • OAS is also associated with an allergy to pollen, especially from silver birch, but also grasses, ragweed (ragwort) and mugwort. 75% of people with silver birch allergy will have OAS. Allergic rhinitis symptoms may flare up when these pollens are in season. • OAS can also occur in people allergic to rubber latex. What to do if a child has an allergic reaction If an allergic reaction occurs, the child should stop eating the food immediately and spit it out. Give the child a dose of antihistamine. In the unlikely event that a severe reaction occurs, then dial 999 for an ambulance. page 2 OAS reactions are usually immediate and occur within 1-5 minutes of the problem food coming into contact with the mouth. -

Latex Allergy: Position Paper
Latex Allergy: Position Paper REVIEW Latex Allergy: Position Paper N Cabañes,1 JM Igea,2 B de la Hoz3 On behalf of the Committee of Latex Allergy of the SEAIC: P Agustín, C Blanco, N Cabañes, J Domínguez, B de la Hoz, JM Igea, M Lázaro, R Lleonart, J Méndez, A Nieto, A Rodríguez, N Rubia, A Tabar, JM Beitia, MC Dieguez, C Martínez-Cócera, S Quirce 1Allergy Department, Hospital Virgen del Valle, Toledo, Spain 2Clínica Alergoasma, Salamanca, Spain 3Servicio de Alergia Hospital Ramón y Cajal, Madrid, Spain ■ Abstract Correct management of latex allergy is essential to ensure adequate care of patients who are allergic to latex, which is ubiquitous in the health care setting. In this Position Paper, the Latex Committee of the Spanish Society of Allergology and Clinical Immunology provides guidelines for the management of latex allergy. Key words: Latex allergy. Guidelines. ■ Resumen El correcto manejo de la alergia al látex es fundamental para garantizar la buena atención de este colectivo de pacientes, dada la ubicuidad de este alergeno en el medio sanitario. El comité de alergia a látex de la SEAIC con este documento de posición pretende resumir de forma clara las directrices a tener en cuenta en esta patología. Palabras clave: Alergia a látex. Recomendaciones. Introduction (with additives), moulding, and vulcanization (a type of polymerization which creates a hard, crystalline structure). Natural rubber is obtained from the Hevea brasiliensis tree. In this type of processing, the protein content is lower, and It takes the form of a milky aqueous suspension and is extracted vulcanization denaturalizes the proteins that remain. -

PE001 Latex Allergy
Latex Allergy Who's at risk and how to lower risk of a reaction This handout explains latex allergy symptoms, what triggers them, who’s at risk, how to lower risk of an allergic reaction and what to do if a reaction happens. What is latex? Latex is made from tree sap and is used to make rubber products. Latex is found in items in hospitals (more rarely today), the community and at home. It is in some clothing, toys, gloves, balloons, condoms, rubber tires and many other items. Look for other materials like plastic, vinyl or silicone to replace latex items. These do not cause latex allergies. What is latex Latex contains proteins that cause allergies in some people. Signs of an allergy? allergic reaction to latex are: • Whole body reaction leading to shock (anaphylaxis: an-eh-fil-AK-siss): Watery eyes, breathing problems (wheezing) • Skin: Swelling, redness, itching, hives or rash These responses occur when latex items touch the skin, the mucous membranes (like inside the nose, mouth, bladder, vagina or rectum) or are breathed into the lungs like when a rubber balloon pops. For some people, the symptoms can get worse the more contact they have with latex. It is rare, but in some cases, a life-threatening reaction called anaphylaxis may happen. This is when the mucous membranes swell and breathing may be cut off. It’s important to have an EpiPen or alternative ready and call your doctor or 911 if this happens. Who is at risk for Anyone can develop a latex allergy, but certain groups are at greater risk of developing a latex becoming allergic. -

Cataract Surgery for Natural Rubber Latex Allergic Patients
Eye (2003) 17, 129–138 & 2003 Nature Publishing Group All rights reserved 0950-222X/03 $25.00 www.nature.com/eye Cataract surgery for D Cheung1 and T Gillow2 REVIEW natural rubber latex allergic patients Abstract In July 2001, the authors were involved in the management of patients undergoing cataract The prevalence of reactions against natural surgery who were known to be NRL sensitive. rubber latex (NRL) is thought to be increasing We discovered that not only did our hospital not in both the general public and healthcare have a formal management plan for NRL- workers. These can vary from mild benign sensitive patients undergoing cataract surgery, skin reactions to bronchospasm, anaphylactic but also that our department was not alone, and shock, and death. Difficulties exist for a brief telephone survey of the theatre sisters of ophthalmic departments wishing to establish other ophthalmic units revealed a similar protocols in providing ‘latex-free situation. Not only were these ophthalmology environments’ for patients undergoing cataract departments lacking a formal protocol of action, surgery. Currently no legislation exists but there was also a general lack of awareness regarding the labelling of NRL-containing amongst ophthalmologists and ophthalmology products in the United Kingdom with nurses to the scale of the problem. information on a product’s NRL content A MEDLINE and EMBASE literature review provided by the manufacturer on a voluntary highlighted several review articles that describe basis only. It is hoped this review article will the magnitude of the problem and basic science act as a basic guide in the management of behind NRL reactions.