Differentiation of Latex Allergy from Irritant Contact Dermatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Fcer11/CD23 Receptor Distribution in Patch Test Reactions to Aeroallergens in Atopic Dermatitis
FceRll/CD23 Receptor Distribution in Patch Test Reactions to Aeroallergens in Atopic Dermatitis Colin C. Buckley, Carol Ivison, Leonard W. Poulter, and Malcolm H.A. Rustin Departments of Dermatology and Immunology (LWP), The Royal Free Hospital and School of Medicine, London, U.K. There is increasing evidence that exposure to organic aller The numbers of Langer hans cells were reduced in the epider gens may induce or exacerbate lesional skin in patients with mis :and increased in the dermis in patch test reactions and atopic dermatitis. In this study, patients with atopic dermati lesional skin compared to their controls. Double staining tis were patch tested to 11 common organic allergens and to reve:aled a change in the distribution of CD23 antigen. In control chambers containing 0.4% phenol and 50% glycerin patch test control and non-Iesional biopsies many macro in 0.9% saline. In biopsies from positive patch test reactions, phages and only a few Langerhans cells within the dermal patch test control skin, lesional eczematous and non-lesional infiltrates expressed this antigen. In patch test reaction and skin from atopic individuals, and normal skin from non lesional skin samples, however, the proportion of CD23+ atopic volunteers, the presence and distribution of macro dermal Langerhans cells had increased compared to macro phages (RFD7+), dendritic cells (RFD1 +), and Langerhans phages. Furthermore, in these latter samples an increased cells, and the expression of the low-affinity receptor for IgE proportion of dermal CD 1+ cells -

Genital Allergy C Sonnex
4 Sex Transm Infect: first published as 10.1136/sti.2003.005132 on 30 January 2004. Downloaded from REVIEW Genital allergy C Sonnex ............................................................................................................................... Sex Transm Infect 2004;80:4–7. doi: 10.1136/sti.2003.005132 Genital allergy should be considered as a possible Local responses consist of genital swelling, burning, irritation, or soreness which may occur diagnosis in all patients with genital soreness or irritation during or soon after intercourse, usually becom- for which no infection or dermatosis can be identified and ing maximal at 24 hours and lasting 2–3 days.45 in whom symptoms remain unchanged or worsen with Semen contact with non-genital skin may also give rise to localised itching and urticaria.67 treatment. Type I and IV hypersensitivity reactions are most Generalised reactions associated with semen commonly encountered and can be assessed by allergy include angioedema of the lips and performing skin prick testing/radioallergosorbent test eyelids,68 laryngeal oedema,9 bronchospasm,10 and anaphylaxis347 but, to date, death has not (RAST) or patch testing, respectively. Type IV reactions been reported. Semen allergy mainly affects (contact dermatitis) may sometimes prove difficult to younger women although postmenopausal cases distinguish clinically from an irritant dermatitis. This clinical are documented.11 12 An increasing intensity of reaction with subsequent episodes of coitus is a review attempts to summarise key features of genital common feature. Levine et al described a married allergy for the practising clinician. woman with a 15 year history of hay fever who ........................................................................... initially presented with swollen eyes, nasal congestion, and sneezing an hour after coitus. -
International Survey on Skin Patch Test Procedures, Attitudes and Interpretation Luciana K
Tanno et al. World Allergy Organization Journal (2016) 9:8 DOI 10.1186/s40413-016-0098-z ORIGINAL RESEARCH Open Access International survey on skin patch test procedures, attitudes and interpretation Luciana K. Tanno1*, Razvigor Darlenski2, Silvia Sánchez-Garcia3, Matteo Bonini4, Andrea Vereda5, Pavel Kolkhir6, Dario Antolin-Amerigo7, Vesselin Dimov8, Claudia Gallego-Corella9, Juan Carlos Aldave Becerra10, Alexander Diaz11, Virginia Bellido Linares12, Leonor Villa13, Lanny J. Rosenwasser14, Mario Sanchez-Borges15, Ignacio Ansotegui16, Ruby Pawankar17, Thomas Bieber18 and on behalf of the WAO Junior Members Group Abstract Background: Skin patch test is the gold standard method in diagnosing contact allergy. Although used for more than 100 years, the patch test procedure is performed with variability around the world. A number of factors can influence the test results, namely the quality of reagents used, the timing of the application, the patch test series (allergens/haptens) that have been used for testing, the appropriate interpretation of the skin reactions or the evaluation of the patient’s benefit. Methods: We performed an Internet –based survey with 38 questions covering the educational background of respondents, patch test methods and interpretation. The questionnaire was distributed among all representatives of national member societies of the World Allergy Organization (WAO), and the WAO Junior Members Group. Results: One hundred sixty-nine completed surveys were received from 47 countries. The majority of participants had more than 5 years of clinical practice (61 %) and routinely carried out patch tests (70 %). Both allergists and dermatologists were responsible for carrying out the patch tests. We could observe the use of many different guidelines regardless the geographical distribution. -

Allergy and Dermatology Patch Test Clinic (ADPT)
4 Skin Patch Tests – Allergy and Dermatology Patch Test Clinic (ADPT) Questions the doctor or nurse will ask you during your first visit. Your answers can help us with collecting your medical information: • When did your symptoms begin? • Have your symptoms changed over time? • What at home treatments have you used? • How did those treatments work? • What, if anything, appears to make your symptoms worse? • Do allergies run in your family? Skin Patch Tests Plan your schedule Allergy and Dermatology Patch Test Clinic (ADPT) Patches are applied on Monday, and then you return on Wednesday for patch removal and Friday for final reading. On Wednesday wear an old or dark coloured shirt. We mark the back after the patches are removed and the ink Why have skin patch testing? may rub off on your clothing. The cause of an allergy is usually found based on: Day Length of visit During the visit Special care • Your symptoms, a rash is very common. Monday 30 to 60 minutes Discussion about the No water or sweat on • A history of contact with substances that cause the allergy. history of your the patches for 2 days. These substances are called allergens. rash/symptoms. Physical exam. When the cause of an allergy is not clear, a skin patch test may be done to Patches applied. help find the cause of your allergy. Skin patch tests are done to see if a Wednesday Short visit Patches removed. Wear an old or dark certain substance is causing an allergic skin reaction. 10 to 15 minutes shirt to this visit. -
Allergy Testing
Effective February 26, 2018 Policy Replaced by LCD L33417 Name of Blue Advantage Policy: Allergy Testing Policy #: 071 Latest Review Date: February 2017 Category: Laboratory/Medical Policy Grade: D Background: Blue Advantage medical policy does not conflict with Local Coverage Determinations (LCDs), Local Medical Review Policies (LMRPs) or National Coverage Determinations (NCDs) or with coverage provisions in Medicare manuals, instructions or operational policy letters. In order to be covered by Blue Advantage the service shall be reasonable and necessary under Title XVIII of the Social Security Act, Section 1862(a)(1)(A). The service is considered reasonable and necessary if it is determined that the service is: 1. Safe and effective; 2. Not experimental or investigational*; 3. Appropriate, including duration and frequency that is considered appropriate for the service, in terms of whether it is: • Furnished in accordance with accepted standards of medical practice for the diagnosis or treatment of the patient’s condition or to improve the function of a malformed body member; • Furnished in a setting appropriate to the patient’s medical needs and condition; • Ordered and furnished by qualified personnel; • One that meets, but does not exceed, the patient’s medical need; and • At least as beneficial as an existing and available medically appropriate alternative. *Routine costs of qualifying clinical trial services with dates of service on or after September 19, 2000 which meet the requirements of the Clinical Trials NCD are considered reasonable and necessary by Medicare. Providers should bill Original Medicare for covered services that are related to clinical trials that meet Medicare requirements (Refer to Medicare National Coverage Determinations Manual, Chapter 1, Section 310 and Medicare Claims Processing Manual Chapter 32, Sections 69.0-69.11). -
Dermatology Patch Allergy Testing Post Service - Information Request Form
Dermatology Patch Allergy Testing Post Service - Information Request Form Blue Cross NC will review associated claim(s) for services rendered on the patient listed below. In order to determine benefits are available for the reported condition, please answer the questions below. If you would prefer to send medical records, relating to the condition for the dates listed you may do so. In this case, all answers must be supported by documentation in the patient's medical record. Please submit the completed form to Blue Cross NC per the Medical Record Submission instructions found on the bcbsnc.com provider site (https://www.bcbsnc.com/assets/providers/public/pdfs/submissions/how_to_submit_provider_initiated_medical_records.pdf) or if requested by Blue Cross NC via a bar-coded coversheet, please fax the form/medical records to the number noted on the bar-coded cover sheet within 7-10 days to facilitate the claim payment. This form must be filled out by the patient's physician or their designee which may be any of the following: Physician Assistant (PA), Nurse Practitioner (NP), Registered Nurse (RN), or Licensed Practical Nurse (LPN). Note: Credentials must be provided with signature or the form will be returned. PROVIDER INFORMATION Requesting Provider Information Place of Service Provider Name Facility Name Provider ID Facility ID PATIENT INFORMATION Patient Name:_____________________________ Patient DOB :_____________ Patient Account Number______________ Patient ID:______________ CLAIM INFORMATION Date(s) of Service_____________ CPT_________ Diagnosis_______ Dermatology Patch Allergy Testing - Information Request Form Page 1 of 3 CLINICAL INFORMATION Did the patient have direct skin testing (for immediate hypersensitivity) by: Percutaneous or epicutaneous (scratch, prick, or puncture)? ________________ Intradermal testing? ___________________________________ Inhalant allergy evaluation? _________________ Did the patient have patch (application) testing (most commonly used: T.R.U.E. -
Allergy Skin and Challenge Testing
Corporate Medical Policy Allergy Skin and Challenge Testing File Name: allergy_skin_and_challenge_testing Origination: 7/1979 Last CAP Review: 11/2020 Next CAP Review: 11/2021 Last Review: 11/2020 Description of Procedure or Service Management of the allergic patient may include identifying the offending agent by means of allergy testing. Allergy testing can be broadly grouped into in vivo and in vitro methodologies: • In vivo testing - includes allergy skin testing such as the scratch, puncture or prick test (epicutaneous), intradermal test (intracutaneous) and patch test, and food and bronchial challenges. • In vitro testing - includes various techniques to test the blood for the presence of specific IgE antibodies to a particular antigen. Once the agent is identified, treatment is provided by avoidance, medication or immunotherapy (allergy shots). Allergic or hypersensitivity disorders may be manifested by generalized systemic reactions as well as by localized reactions in any organ system of the body. The reactions may be acute, subacute, or chronic, immediate or delayed, and may be caused by numerous offending agents: pollen, molds, dust mites, animal dander, stinging insect venoms, foods, drugs, etc. This policy only addresses in vivo (skin and challenge) testing; for vitro testing, see policy titled, Allergen Testing. Related Policies: Allergy Immunotherapy Desensitization Allergen Testing AHS – G2031 Maximum Units of Service Idi ***Note: This Medical Policy is complex and technical. For questions concerning the technical language and/or specific clinical indications for its use, please consult your physician. Policy BCBSNC will provide coverage for Allergy skin and challenge testing when it is determined to be medically necessary because the medical criteria and guidelines shown below are met. -

Guideline on Diagnostic Procedures for Suspected Hypersensitivity to Beta-Lactam Antibiotics
published by: guidelines Allergo J Int https://doi.org/10.1007/s40629-019-0100-8 Guideline on diagnostic procedures for suspected hypersensitivity to beta-lactam antibiotics Guideline of the German Society for Allergology and Clinical Immunology (DGAKI) in collaboration with the German Society of Allergology (AeDA), German Society for Pediatric Allergology and Environmental Medicine (GPA), the German Contact Dermatitis Research Group (DKG), the Austrian Society for Allergology and Immunology (ÖGAI), and the Paul-Ehrlich Society for Chemotherapy (PEG) Gerda Wurpts · Werner Aberer · Heinrich Dickel · Randolf Brehler · Thilo Jakob · Burkhard Kreft · Vera Mahler · Hans F. Merk · Norbert Mülleneisen · Hagen Ott · Wolfgang Pfützner · Stefani Röseler · Franziska Ruëff · Helmut Sitter · Cord Sunderkötter · Axel Trautmann · Regina Treudler · Bettina Wedi · Margitta Worm · Knut Brockow © The Author(s) 2019 Electronic supplementary material The online version of this article (https://doi.org/10.1007/s40629-019-0100-8) contains supplementary material, which is available to authorized users. Dr. G. Wurpts () · H. F.Merk · S. Röseler V. Ma h l e r Clinic for Dermatology and Allergology, Aachen Paul-Ehrlich Institute, Langen, Germany Comprehensive Allergy Center (ACAC), Uniklinik RWTH Department of Dermatology, University Hospital Erlangen, Aachen, Pauwelsstraße 30, 52074 Aachen, Germany Erlangen, Germany [email protected] N. Mülleneisen W. Aberer Asthma and Allergy Centre, Leverkusen, Germany Department of Dermatology, Graz Medical University, Graz, Austria H. Ott Division of Pediatric Dermatology and Allergology, Auf der H. Dickel Bult Children’s Hospital, Hannover, Germany Department of Dermatology, Venereology and Allergology, St. Josef Hospital, University Hospital of the Ruhr University W. Pfützner Bochum, Bochum, Germany Department of Dermatology and Allergology, University Hospital Gießen und Marburg, Marburg Site, Marburg, R. -

Hypersensitivity Reactions (Types I, II, III, IV)
Hypersensitivity Reactions (Types I, II, III, IV) April 15, 2009 Inflammatory response - local, eliminates antigen without extensively damaging the host’s tissue. Hypersensitivity - immune & inflammatory responses that are harmful to the host (von Pirquet, 1906) - Type I Produce effector molecules Capable of ingesting foreign Particles Association with parasite infection Modified from Abbas, Lichtman & Pillai, Table 19-1 Type I hypersensitivity response IgE VH V L Cε1 CL Binds to mast cell Normal serum level = 0.0003 mg/ml Binds Fc region of IgE Link Intracellular signal trans. Initiation of degranulation Larche et al. Nat. Rev. Immunol 6:761-771, 2006 Abbas, Lichtman & Pillai,19-8 Factors in the development of allergic diseases • Geographical distribution • Environmental factors - climate, air pollution, socioeconomic status • Genetic risk factors • “Hygiene hypothesis” – Older siblings, day care – Exposure to certain foods, farm animals – Exposure to antibiotics during infancy • Cytokine milieu Adapted from Bach, JF. N Engl J Med 347:911, 2002. Upham & Holt. Curr Opin Allergy Clin Immunol 5:167, 2005 Also: Papadopoulos and Kalobatsou. Curr Op Allergy Clin Immunol 7:91-95, 2007 IgE-mediated diseases in humans • Systemic (anaphylactic shock) •Asthma – Classification by immunopathological phenotype can be used to determine management strategies • Hay fever (allergic rhinitis) • Allergic conjunctivitis • Skin reactions • Food allergies Diseases in Humans (I) • Systemic anaphylaxis - potentially fatal - due to food ingestion (eggs, shellfish, -
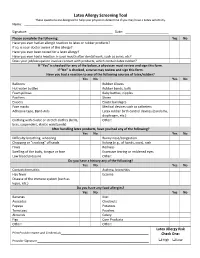
Latex Allergy Screening Tool These Questions Are Designed to Help Your Physician Determine If You May Have a Latex Sensitivity
Latex Allergy Screening Tool These questions are designed to help your physician determine if you may have a Latex sensitivity. Name: ____________________________________ __________ Signature: _________________________________ __________ Date: ______ _______________ Please complete the following: Yes No Have you ever had an allergic reaction to latex or rubber products? If so, is your doctor aware of this allergy? Have you ever been tested for a latex allergy? Have you ever had a reaction in your mouth after dental work, such as sores, etc? Does your job/occupation involve contact with products, which contain latex rubber? If “Yes” is checked for any of the below, a physician must review and sign this form. If “No” is checked, a nurse may review and sign this form. Have you had a reaction to any of the following sources of latex/rubber? Yes No Yes No Balloons Rubber Gloves Hot water bottles Rubber bands, balls Foam pillows Baby bottles, nipples Pacifiers Shoes Erasers Elastic bandages Face masks Medical devices such as catheters Adhesive tape, Band‐Aids Latex rubber birth control devices (condoms, diaphragm, etc.) Clothing with elastic or stretch clothes (belts, Other: bras, suspenders, elastic waistbands) After handling latex products, have you had any of the following? Yes No Yes No Difficulty breathing, wheezing Runny nose/congestion Chapping or “cracking” of hands Itching (e.g., of hands, eyes), rash Hives Redness Swelling of the body, tongue or face Excessive tearing or reddened eyes Low blood pressure Other: Do you have a history any of the following? Yes No Yes No Contact dermatitis Asthma, bronchitis Hay fever Eczema Disease of the immune system (such as lupus, etc.) Do you have any food allergies? Yes No Yes No Bananas Kiwi Avocados Chestnuts Papaya Potatoes Tomatoes Peaches Almonds Celery Figs Corn Products Other: Other: Latex Allergy Risk Print Provider Name and Credentials_________________________________________________ Check One: Provider Signature ______________________________________________________________ High Low . -

Latex Allergy/Student Effective Date: 1/1/10
OCHSNER CLINICAL SCHOOL POLICY Policy #: OCS 400.14 Title: Latex Allergy/Student Effective Date: 1/1/10 PURPOSE The purpose of this policy is to establish guidelines for the identification, follow-up and work practice modification for all OCS medical students with latex sensitivities or allergies to ensure a consistent safe workplace. Students will be classified in the category of Health Care Worker (HCW) on the Ochsner campuses. Health Care Workers with demonstrated latex sensitivity will be provided with engineering controls, protective apparel and other interventions that will minimize opportunities for development of a true latex allergy. HCW’s with a diagnosed latex allergy will be provided a latex safe environment to the extent possible. DEFINITIONS: Latex refers to natural rubber latex and includes products made from dry natural rubber. Natural rubber latex is the product manufactured from a milky fluid derived mainly from the rubber tree, Hevea brasiliensis. High-risk populations are groups known to have a higher risk for latex allergic reactions and include persons: • with occupational exposure to latex, • diagnosed with myelodysplasia, myeloma, congenital urologic abnormalities, or Spina bifida • with history of asthma, hay fever, contact dermatitis, or autoimmune disease (i.e. Lupus), • with food allergies such as bananas, avocados, potatoes, tomatoes, kiwi fruit, peaches, papaya, fruit or chestnuts and • who have exhibited contact dermatitis, itching or redness of the skin following the touching or wearing of latex products. Sensitization is the development of immunological memory in response to exposure to an antigen. Sensitivity is a clinical response that develops after sensitizations. Allergic reactions range from urticaria, rhinitis, conjunctivitis, angiodema, laryngeal edema, cardiovascular changes, GI upset, psychological distress, and bronchospasm, to severe life threatening anaphylaxis. -

Screening Tool
Natural Rubber Latex Allergy Patient Screening Questionnaire When patients are first being assessed, whether in out-patients, assessment clinics, admission or prior to any intervention in clinical settings, it is important that their allergic status is determined as far as is possible. This assessment tool should aid that process. 1. Initial Assessment i. Ask the patient if they have an allergy to any medicines, foods or other items ii. If the patient states that they have no allergies then treat as normal iii. If the patient states that they are allergic to any of the following, this should trigger additional questioning; balloons, contraceptives, rubber gloves, dental blocks, hot water bottles, erasers, rubber bands/balls, pillows, elastic dressing and bandages, elastic waistbands/underwear. iii. If the patient states that they are allergic to any of the following, this should trigger additional questioning; apples, avocados, bananas, celery, cherries, chestnuts, ficus, figs, grapes, kiwi, latex, mangoes, melons, passion fruit, peaches, pears, pistachios, potatoes, ragweed, strawberries, tomatoes. TREAT AS HIGH RISK 2. Further questions a. Ask the patient what symptoms they experience when they eat/touch the products listed above b. If the patient states any of the following symptoms, further questions should be asked; breathlessness, skin redness, chapping or cracking of hands, swelling of lips or tongue, runny nose, congestion, hives, itching. TREAT AS TYPE I 3. Assessment conclusion If the patient in addition to positive responses to the questions above, suffers from any of the following then treat as a high risk individual and follow the protocol; • Contact dermatitis • Spina bifida • Eczema • Multiple genitourinary • Asthma • Auto-immune disease (Lupus etc) • Hay fever TREAT AS TYPE I If the patient assessment results in a high-risk outcome, then label the patient’s notes and notify all others who may treat the patient.