Exome Sequencing Identifies the Cause of a Mendelian Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Miller Syndrome (Postaxial Acrofacial Dysostosis): and Expansion of The
J Med Genet: first published as 10.1136/jmg.28.10.695 on 1 October 1991. Downloaded from J Med Genet 1991; 28: 695-700 695 Miller syndrome (postaxial acrofacial dysostosis): further evidence for autosomal recessive inheritance and expansion of the phenotype A L Ogilvy-Stuart, A C Parsons Abstract Case reports A sibship with postaxial acrofacial dysostosis CASE 1 syndrome (Miller syndrome) is reported. In This girl is the second daughter born to unrelated addition to the characteristic facial and limb Caucasian parents. The first child is apparently defects, previously undescribed anomalies, entirely normal. At the time of delivery the mother including midgut malrotation, gastric volvu- was 26 years old, and the father 29 years. The lus, and renal anomalies, are recorded. pregancy was uncomplicated and no drugs were taken. She was born at term by lower section caesar- ian section for failure to progress. The Apgar score Miller syndrome is a rare, well defined malformation at one and five minutes was 8. No resuscitation was syndrome. The craniofacial abnormalities are simi- required. At birth her weight was 3160 g (25th lar to those of the Treacher Collins syndrome. The centile), length 46cm (less than the 10th centile), limb defects predominantly involve the postaxial and the head circumference 34 cm (25th centile). ray, with a wide range of severity, and to a lesser The following facial abnormalities were noted: extent the preaxial ray. micrognathia, malar hypoplasia, small shallow orbits copyright. The syndrome was first described as a complete with bilateral proptosis, downward slanting palpe- clinical entity by Miller et all in 1979. -

Download CGT Exome V2.0
CGT Exome version 2. -

Cell-Based Analysis of CAD Variants Identifies Individuals Likely to Benefit from Uridine Therapy
ARTICLE © American College of Medical Genetics and Genomics Cell-based analysis of CAD variants identifies individuals likely to benefit from uridine therapy Francisco del Caño-Ochoa, PhD1,2,25, Bobby G. Ng, BS3, Malak Abedalthagafi, MD4, Mohammed Almannai, MD5, Ronald D. Cohn, MD6,7,8,9, Gregory Costain, MD6,10, Orly Elpeleg, MD11, Henry Houlden, MD, PhD12, Ehsan Ghayoor Karimiani, MD, PhD13, Pengfei Liu, PhD14,15, M. Chiara Manzini, PhD16, Reza Maroofian, PhD12, Michael Muriello, MD17,18, Ali Al-Otaibi, MD19, Hema Patel, MD20, Edvardson Shimon, MD21, V. Reid Sutton, MD22, Mehran Beiraghi Toosi, MD23, Lynne A. Wolfe, MS24, Jill A. Rosenfeld, MS14,15, Hudson H. Freeze, PhD3 and Santiago Ramón-Maiques, PhD 1,2,25 Purpose: Pathogenic autosomal recessive variants in CAD,encoding Results: We identified 25 individuals with biallelic variants in CAD the multienzymatic protein initiating pyrimidine de novo biosynth- and a phenotype consistent with a CAD deficit. We used the CAD- esis, cause a severe inborn metabolic disorder treatable with a dietary knockout complementation assay to test a total of 34 variants, supplement of uridine. This condition is difficult to diagnose given identifying 16 as deleterious for CAD activity. Combination of these the large size of CAD with over 1000 missense variants and pathogenic variants confirmed 11 subjects with a CAD deficit, for the nonspecific clinical presentation. We aimed to develop a whom we describe the clinical phenotype. reliable and discerning assay to assess the pathogenicity of CAD Conclusions: We designed a cell-based assay to test the variants and to select affected individuals that might benefit from pathogenicity of CAD variants, identifying 11 CAD-deficient uridine therapy. -

Felty's Syndrome - Definition of Felty's Syndrome by Medical Dictionary
Felty's syndrome - definition of Felty's syndrome by Medical dictionary forum List Mailing Day the of Word the Join webmasters For Dictionary, Ency Ency Dictionary, T E X T TheFreeDictionary Google Bing E-mail ? Password 60% Word / Article Starts with Ends with Text Remember Me 6,931,716,780 visitors served. Register Forgot password? Dictionary/ Medical Legal Financial Acronyms Idioms Encyclopedia Wikipedia ? thesaurus dictionary dictionary dictionary encyclopedia Felty's syndrome Also found in: Dictionary/thesaurus, Encyclopedia, Wikipedia 0.01 sec. Page tools ? Like 0 Share: Cite / link: On this page Printer friendly Feedback Word Browser Cite / link Add definition syndrome /syn·drome/ (sin´drōm) a set of symptoms occurring together; the sum of signs of any morbid state; a symptom complex. See also entries under disease. This site: Aarskog syndrome , Aarskog-Scott syndrome a hereditary X-linked condition characterized by ocular Like 334k hypertelorism, anteverted nostrils, broad upper lip, peculiar scrotal “shawl” above the penis, and small hands. on h Wr o te a MiigList Mailing Day the of Word the Join acquired immune deficiency syndrome , acquired immunodeficiency syndrome an epidemic, Follow: Share: transmissible retroviral disease caused by infection with the human immunodeficiency virus, manifested in severe cases as profound depression of cell-mediated immunity, and affecting certain recognized risk groups. Diagnosis is by the presence of a disease indicative of a defect in cell-mediated immunity (e.g., life- threatening opportunistic infection) in the absence of any known causes of underlying immunodeficiency or of any other host defense defects reported to be associated with that disease (e.g., iatrogenic immunosuppression). -
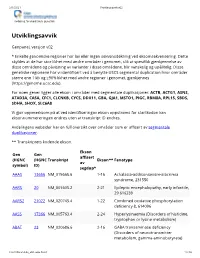
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate) -

Modulating Pyrimidine Ribonucleotide Levels for the Treatment of Cancer Tanzina Mollick1,2 and Sonia Laín1,2*
Mollick and Laín Cancer & Metabolism (2020) 8:12 https://doi.org/10.1186/s40170-020-00218-5 REVIEW Open Access Modulating pyrimidine ribonucleotide levels for the treatment of cancer Tanzina Mollick1,2 and Sonia Laín1,2* Abstract By providing the necessary building blocks for nucleic acids and precursors for cell membrane synthesis, pyrimidine ribonucleotides are essential for cell growth and proliferation. Therefore, depleting pyrimidine ribonucleotide pools has long been considered as a strategy to reduce cancer cell growth. Here, we review the pharmacological approaches that have been employed to modulate pyrimidine ribonucleotide synthesis and degradation routes and discuss their potential use in cancer therapy. New developments in the treatment of myeloid malignancies with inhibitors of pyrimidine ribonucleotide synthesis justify revisiting the literature as well as discussing whether targeting this metabolic pathway can be effective and sufficiently selective for cancer cells to warrant an acceptable therapeutic index in patients. Keywords: Pyrimidine ribonucleotide metabolism, Cancer therapy, CAD, DHODH, UMPS, Nucleoside transporters, CDA, CTPS, Therapeutic index Background pyrimidine ribonucleotide pools has long been consid- Pyrimidine ribonucleotides are involved in multiple ered an option for cancer treatment. In light of this, a cellular processes that maintain cell growth and me- number of inhibitors of enzymes of the pyrimidine ribo- tabolism [1]. Aside from being the building blocks nucleotide synthesis pathway have been developed in the of RNA and precursors for deoxyribonucleotides, past decades. However, due to unsatisfactory results in pyrimidine ribonucleotides are necessary for glyco- the clinic, further work in this line of therapy was not gen and cell membrane precursor synthesis, glyco- given priority [21–31]. -
Prevalence of Rare Diseases: Bibliographic Data
Prevalence distribution of rare diseases 200 180 160 140 120 100 80 Number of diseases 60 November 2009 40 May 2014 Number 1 20 0 0 5 10 15 20 25 30 35 40 45 50 Estimated prevalence (/100000) Prevalence of rare diseases: Bibliographic data Listed in alphabetical order of disease or group of diseases www.orpha.net Methodology A systematic survey of the literature is being Updated Data performed in order to provide an estimate of the New information from available data sources: EMA, prevalence of rare diseases in Europe. An updated new scientific publications, grey literature, expert report will be published regularly and will replace opinion. the previous version. This update contains new epidemiological data and modifications to existing data for which new information has been made Limitation of the study available. The exact prevalence rate of each rare disease is difficult to assess from the available data sources. Search strategy There is a low level of consistency between studies, a poor documentation of methods used, confusion The search strategy is carried out using several data between incidence and prevalence, and/or confusion sources: between incidence at birth and life-long incidence. - Websites: Orphanet, e-medicine, GeneClinics, EMA The validity of the published studies is taken for and OMIM ; granted and not assessed. It is likely that there - Registries, RARECARE is an overestimation for most diseases as the few - Medline is consulted using the search algorithm: published prevalence surveys are usually done in «Disease names» AND Epidemiology[MeSH:NoExp] regions of higher prevalence and are usually based OR Incidence[Title/abstract] OR Prevalence[Title/ on hospital data. -

WES Gene Package Metabolic Disorders.Xlsx
Whole Exome Sequencing Gene package Metabolic disorders, version 5, 30‐9‐2019 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x AASS Hyperlysinemia, 238700 605113 63 100 97 90 Saccharopinuria, 268700 ABAT GABA‐transaminase deficiency, 613163 137150 100 100 100 96 ABCA1 HDL deficiency, familial, 1, 604091 600046 92 100 100 97 Tangier disease, 205400 ABCB11 Cholestasis, benign recurrent intrahepatic, -

Mackenzie's Mission Gene & Condition List
Mackenzie’s Mission Gene & Condition List What conditions are being screened for in Mackenzie’s Mission? Genetic carrier screening offered through this research study has been carefully developed. It is focused on providing people with information about their chance of having children with a severe genetic condition occurring in childhood. The screening is designed to provide genetic information that is relevant and useful, and to minimise uncertain and unclear information. How the conditions and genes are selected The Mackenzie’s Mission reproductive genetic carrier screen currently includes approximately 1300 genes which are associated with about 750 conditions. The reason there are fewer conditions than genes is that some genetic conditions can be caused by changes in more than one gene. The gene list is reviewed regularly. To select the conditions and genes to be screened, a committee comprised of experts in genetics and screening was established including: clinical geneticists, genetic scientists, a genetic pathologist, genetic counsellors, an ethicist and a parent of a child with a genetic condition. The following criteria were developed and are used to select the genes to be included: • Screening the gene is technically possible using currently available technology • The gene is known to cause a genetic condition • The condition affects people in childhood • The condition has a serious impact on a person’s quality of life and/or is life-limiting o For many of the conditions there is no treatment or the treatment is very burdensome for the child and their family. For some conditions very early diagnosis and treatment can make a difference for the child. -

ORPHA Number Disease Or Group of Diseases 300305 11P15.4
Supplementary material J Med Genet ORPHA Disease or Group of diseases Number 300305 11p15.4 microduplication syndrome 444002 11q22.2q22.3 microdeletion syndrome 313884 12p12.1 microdeletion syndrome 94063 12q14 microdeletion syndrome 412035 13q12.3 microdeletion syndrome 261120 14q11.2 microdeletion syndrome 261229 14q11.2 microduplication syndrome 261144 14q12 microdeletion syndrome 264200 14q22q23 microdeletion syndrome 401935 14q24.1q24.3 microdeletion syndrome 314585 15q overgrowth syndrome 261183 15q11.2 microdeletion syndrome 238446 15q11q13 microduplication syndrome 199318 15q13.3 microdeletion syndrome 261190 15q14 microdeletion syndrome 94065 15q24 microdeletion syndrome 261211 16p11.2p12.2 microdeletion syndrome 261236 16p13.11 microdeletion syndrome 261243 16p13.11 microduplication syndrome 352629 16q24.1 microdeletion syndrome 261250 16q24.3 microdeletion syndrome 217385 17p13.3 microduplication syndrome 97685 17q11 microdeletion syndrome 139474 17q11.2 microduplication syndrome 261272 17q12 microduplication syndrome 363958 17q21.31 microdeletion syndrome 261279 17q23.1q23.2 microdeletion syndrome 254346 19p13.12 microdeletion syndrome 357001 19p13.13 microdeletion syndrome 447980 19p13.3 microduplication syndrome 217346 19q13.11 microdeletion syndrome 293948 1p21.3 microdeletion syndrome 401986 1p31p32 microdeletion syndrome 456298 1p35.2 microdeletion syndrome 250994 1q21.1 microduplication syndrome 238769 1q44 microdeletion syndrome 261295 20p12.3 microdeletion syndrome 313781 20p13 microdeletion syndrome 444051 20q11.2 -

Inborn Metabolic Diseases, DOI 10.1007/978-3-662-49771-5 , © Springer-Verlag Berlin Heidelberg 2016 644 Subject Index
643 Subject Index J.-M. Saudubray et al. (Eds.), Inborn Metabolic Diseases, DOI 10. -

Newborndxtm Advanced Sequencing Evaluation Disorders List
NewbornDxTM Advanced Sequencing Evaluation Disorders List Skeletal Abnormal bone and cartilage Contractures (cont.) Disorder Associated gene(s) Disorder Associated gene(s) Alpha-mannosidosis MAN2B1 Lethal arthrogryposis, with anterior GLE1 horn cell disease Camurati-Engelmann disease TGFB1 Lethal congenital contracture syndrome ADCY6, CNTNAP1, DNM2, Cerebrocostomandibular syndrome SNRPB ERBB3, GLE1, MYBPC1, Chondrocalcinosis ANKH PIP5K1C Chondrodysplasia punctata ARSE, EBP, PTH1R Marden-Walker syndrome PIEZO2 Chondrodysplasia with joint dislocations IMPAD1 Multicentric osteolysis, MMP2 nodulosis, and arthropathy Craniometaphyseal dysplasia ANKH Osteogenesis Imperfecta BMP1 Eiken syndrome PTH1R Osteogenesis imperfecta COL1A1, COL1A2, CRTAP, Familial osteochondritis dissecans ACAN FKBP10, IFITM5, P3H1, PPIB, Fibrodysplasia ossificans progressiva ACVR1 SERPINF1, SERPINH1, SP7, TMEM38B, WNT1 Hyperphosphatasia with PGAP3, PIGV mental retardation syndrome Osteopathia striata with cranial sclerosis AMER1 Kabuki syndrome KDM6A Osteopetrosis with renal tubular acidosis CA2 Keutel syndrome MGP Van den Ende-Gupta syndrome SCARF2 Klippel-Feil syndrome GDF3, GDF6, MEOX1, Winchester syndrome MMP14 MYO18B Lethal restrictive dermopathy ZMPSTE24 Hand and foot abnormalities Mandibuloacral dysplasia with ZMPSTE24 Adams-Oliver syndrome ARHGAP31, DOCK6, EOGT, type B lipodystrophy NOTCH1 Marshall-Smith syndrome NFIX Atelosteogenesis SLC26A2 Metaphyseal chondrodysplasia PTH1R Bardet-Biedl syndrome ARL6, BBIP1, IFT27, LZTFL1, MKKS, MKS1 Multiple epiphyseal dysplasia