ORPHA Number Disease Or Group of Diseases 300305 11P15.4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CADASIL Testing
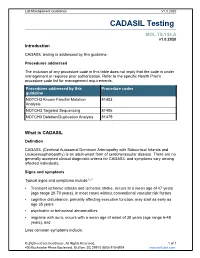
Lab Management Guidelines V1.0.2020 CADASIL Testing MOL.TS.144.A v1.0.2020 Introduction CADASIL testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline NOTCH3 Known Familial Mutation 81403 Analysis NOTCH3 Targeted Sequencing 81406 NOTCH3 Deletion/Duplication Analysis 81479 What is CADASIL Definition CADASIL (Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy) is an adult-onset form of cerebrovascular disease. There are no generally accepted clinical diagnostic criteria for CADASIL and symptoms vary among affected individuals. Signs and symptoms Typical signs and symptoms include1,2,3 Transient ischemic attacks and ischemic stroke, occurs at a mean age of 47 years (age range 20-70 years), in most cases without conventional vascular risk factors cognitive disturbance, primarily affecting executive function, may start as early as age 35 years psychiatric or behavioral abnormalities migraine with aura, occurs with a mean age of onset of 30 years (age range 6-48 years), and Less common symptoms include: © 2020 eviCore healthcare. All Rights Reserved. 1 of 7 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 recurrent seizures with onset in middle age, usually secondary to stroke acute encephalopathy, with a mean age of onset of 42 years Life expectancy for men with CADASIL is reduced by approximately five years and for women by 1 to 2 years.4 Diagnosis Brain Magnetic Resonance Imaging (MRI) findings include T2-signal-abnormalities in the white matter of the temporal pole and T2-signal-abnormalities in the external capsule and corpus callosum.1,2 CADASIL is suspected in an individual with the clinical signs and MRI findings. -

Mimics, Miscalls, and Misses in Pancreatic Disease Koenraad J
Mimics, Miscalls, and Misses in Pancreatic Disease Koenraad J. Mortelé1 The radiologist plays a pivotal role in the detection and This chapter will summarize, review, and illustrate the characterization of pancreatic disorders. Unfortunately, the most common and important mimics, miscalls, and misses in accuracy of rendered diagnoses is not infrequently plagued by pancreatic imaging and thereby improve diagnostic accuracy a combination of “overcalls” of normal pancreatic anomalies of diagnoses rendered when interpreting radiologic studies of and variants; “miscalls” of specific and sometimes pathog- the pancreas. nomonic pancreatic entities; and “misses” of subtle, uncom- mon, or inadequately imaged pancreatic abnormalities. Ba- Normal Pancreatic Anatomy sic understanding of the normal and variant anatomy of the The Gland pancreas, knowledge of state-of-the-art pancreatic imaging The coarsely lobulated pancreas, typically measuring ap- techniques, and familiarity with the most commonly made mis- proximately 15–20 cm in length, is located in the retroperito- diagnoses and misses in pancreatic imaging is mandatory to neal anterior pararenal space and can be divided in four parts: avoid this group of errors. head and uncinate process, neck, body, and tail [4]. The head, neck, and body are retroperitoneal in location whereas the Mimics of pancreatic disease, caused by developmental tail extends into the peritoneal space. The pancreatic head is variants and anomalies, are commonly encountered on imag- defined as being to the right of the superior mesenteric vein ing studies [1–3]. To differentiate these benign “nontouch” en- (SMV). The uncinate process is the prolongation of the medi- tities from true pancreatic conditions, radiologists should be al and caudal parts of the head; it has a triangular shape with a familiar with them, the imaging techniques available to study straight or concave anteromedial border. -

Next Generation Sequencing Panels for Disorders of Sex Development
Next Generation Sequencing Panels for Disorders of Sex Development Disorders of Sex Development – Overview Disorders of sex development (DSDs) occur when sex development does not follow the course of typical male or female patterning. Types of DSDs include congenital development of ambiguous genitalia, disjunction between the internal and external sex anatomy, incomplete development of the sex anatomy, and abnormalities of the development of gonads (such as ovotestes or streak ovaries) (1). Sex chromosome anomalies including Turner syndrome and Klinefelter syndrome as well as sex chromosome mosaicism are also considered to be DSDs. DSDs can be caused by a wide range of genetic abnormalities (2). Determining the etiology of a patient’s DSD can assist in deciding gender assignment, provide recurrence risk information for future pregnancies, and can identify potential health problems such as adrenal crisis or gonadoblastoma (1, 3). Sex chromosome aneuploidy and copy number variation are common genetic causes of DSDs. For this reason, chromosome analysis and/or microarray analysis typically should be the first genetic analysis in the case of a patient with ambiguous genitalia or other suspected disorder of sex development. Identifying whether a patient has a 46,XY or 46,XX karyotype can also be helpful in determining appropriate additional genetic testing. Abnormal/Ambiguous Genitalia Panel Our Abnormal/Ambiguous Genitalia Panel includes mutation analysis of 72 genes associated with both syndromic and non-syndromic DSDs. This comprehensive panel evaluates a broad range of genetic causes of ambiguous or abnormal genitalia, including conditions in which abnormal genitalia are the primary physical finding as well as syndromic conditions that involve abnormal genitalia in addition to other congenital anomalies. -

Oral Health in Prevalent Types of Ehlers–Danlos Syndromes
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Ghent University Academic Bibliography J Oral Pathol Med (2005) 34: 298–307 ª Blackwell Munksgaard 2005 Æ All rights reserved www.blackwellmunksgaard.com/jopm Oral health in prevalent types of Ehlers–Danlos syndromes Peter J. De Coster1, Luc C. Martens1, Anne De Paepe2 1Department of Paediatric Dentistry, Centre for Special Care, Paecamed Research, Ghent University, Ghent; 2Centre for Medical Genetics, Ghent University Hospital, Ghent, Belgium BACKGROUND: The Ehlers–Danlos syndromes (EDS) Introduction comprise a heterogenous group of heritable disorders of connective tissue, characterized by joint hypermobility, The Ehlers–Danlos syndromes (EDS) comprise a het- skin hyperextensibility and tissue fragility. Most EDS erogenous group of heritable disorders of connective types are caused by mutations in genes encoding different tissue, largely characterized by joint hypermobility, skin types of collagen or enzymes, essential for normal pro- hyperextensibility and tissue fragility (1) (Fig. 1). The cessing of collagen. clinical features, modes of inheritance and molecular METHODS: Oral health was assessed in 31 subjects with bases differ according to the type. EDS are caused by a EDS (16 with hypermobility EDS, nine with classical EDS genetic defect causing an error in the synthesis or and six with vascular EDS), including signs and symptoms processing of collagen types I, III or V. The distribution of temporomandibular disorders (TMD), alterations of and function of these collagen types are displayed in dental hard tissues, oral mucosa and periodontium, and Table 1. At present, two classifications of EDS are was compared with matched controls. -

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

The Genetic Basis for Skeletal Diseases
insight review articles The genetic basis for skeletal diseases Elazar Zelzer & Bjorn R. Olsen Harvard Medical School, Department of Cell Biology, 240 Longwood Avenue, Boston, Massachusetts 02115, USA (e-mail: [email protected]) We walk, run, work and play, paying little attention to our bones, their joints and their muscle connections, because the system works. Evolution has refined robust genetic mechanisms for skeletal development and growth that are able to direct the formation of a complex, yet wonderfully adaptable organ system. How is it done? Recent studies of rare genetic diseases have identified many of the critical transcription factors and signalling pathways specifying the normal development of bones, confirming the wisdom of William Harvey when he said: “nature is nowhere accustomed more openly to display her secret mysteries than in cases where she shows traces of her workings apart from the beaten path”. enetic studies of diseases that affect skeletal differentiation to cartilage cells (chondrocytes) or bone cells development and growth are providing (osteoblasts) within the condensations. Subsequent growth invaluable insights into the roles not only of during the organogenesis phase generates cartilage models individual genes, but also of entire (anlagen) of future bones (as in limb bones) or membranous developmental pathways. Different mutations bones (as in the cranial vault) (Fig. 1). The cartilage anlagen Gin the same gene may result in a range of abnormalities, are replaced by bone and marrow in a process called endo- and disease ‘families’ are frequently caused by mutations in chondral ossification. Finally, a process of growth and components of the same pathway. -

Spectrum of PEX1 and PEX6 Variants in Heimler Syndrome
European Journal of Human Genetics (2016) 24, 1565–1571 Official Journal of The European Society of Human Genetics www.nature.com/ejhg ARTICLE Spectrum of PEX1 and PEX6 variants in Heimler syndrome Claire EL Smith1, James A Poulter1, Alex V Levin2,3,4, Jenina E Capasso4, Susan Price5, Tamar Ben-Yosef6, Reuven Sharony7, William G Newman8,9, Roger C Shore10, Steven J Brookes10, Alan J Mighell1,11,12 and Chris F Inglehearn*,1,12 Heimler syndrome (HS) consists of recessively inherited sensorineural hearing loss, amelogenesis imperfecta (AI) and nail abnormalities, with or without visual defects. Recently HS was shown to result from hypomorphic mutations in PEX1 or PEX6,both previously implicated in Zellweger Syndrome Spectrum Disorders (ZSSD). ZSSD are a group of conditions consisting of craniofacial and neurological abnormalities, sensory defects and multi-organ dysfunction. The finding of HS-causing mutations in PEX1 and PEX6 shows that HS represents the mild end of the ZSSD spectrum, though these conditions were previously thought to be distinct nosological entities. Here, we present six further HS families, five with PEX6 variants and one with PEX1 variants, and show the patterns of Pex1, Pex14 and Pex6 immunoreactivity in the mouse retina. While Ratbi et al. found more HS-causing mutations in PEX1 than in PEX6, as is the case for ZSSD, in this cohort PEX6 variants predominate, suggesting both genes play a significant role in HS. The PEX6 variant c.1802G4A, p.(R601Q), reported previously in compound heterozygous state in one HS and three ZSSD cases, was found in compound heterozygous state in three HS families. -

To View the ESE Recommended Curriculum of Specialisation in Clinical Endocrinology, Diabetes and Metabolism
European Society of Endocrinology Recommended Curriculum of Specialisation in Clinical Endocrinology, Diabetes and Metabolism Version 2, November 2019 Contents Endorsement ........................................................................................................................................ 2 Introduction .......................................................................................................................................... 3 1. Diabetes mellitus .............................................................................................................................. 4 2. Lipid disorders ................................................................................................................................... 5 3. Obesity and bariatric endocrinology ................................................................................................. 5 4. Pituitary ............................................................................................................................................ 5 5. Thyroid .............................................................................................................................................. 6 6. Parathyroid, calcium and bone ......................................................................................................... 7 7. Adrenal ............................................................................................................................................. 8 8. Reproductive endocrinology and sexual function -

Peripheral Neuropathy in Complex Inherited Diseases: an Approach To
PERIPHERAL NEUROPATHY IN COMPLEX INHERITED DISEASES: AN APPROACH TO DIAGNOSIS Rossor AM1*, Carr AS1*, Devine H1, Chandrashekar H2, Pelayo-Negro AL1, Pareyson D3, Shy ME4, Scherer SS5, Reilly MM1. 1. MRC Centre for Neuromuscular Diseases, UCL Institute of Neurology and National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 2. Lysholm Department of Neuroradiology, National Hospital for Neurology and Neurosurgery, London, WC1N 3BG, UK. 3. Unit of Neurological Rare Diseases of Adulthood, Carlo Besta Neurological Institute IRCCS Foundation, Milan, Italy. 4. Department of Neurology, University of Iowa, 200 Hawkins Drive, Iowa City, IA 52242, USA 5. Department of Neurology, University of Pennsylvania, Philadelphia, PA 19014, USA. * These authors contributed equally to this work Corresponding author: Mary M Reilly Address: MRC Centre for Neuromuscular Diseases, 8-11 Queen Square, London, WC1N 3BG, UK. Email: [email protected] Telephone: 0044 (0) 203 456 7890 Word count: 4825 ABSTRACT Peripheral neuropathy is a common finding in patients with complex inherited neurological diseases and may be subclinical or a major component of the phenotype. This review aims to provide a clinical approach to the diagnosis of this complex group of patients by addressing key questions including the predominant neurological syndrome associated with the neuropathy e.g. spasticity, the type of neuropathy, and the other neurological and non- neurological features of the syndrome. Priority is given to the diagnosis of treatable conditions. Using this approach, we associated neuropathy with one of three major syndromic categories - 1) ataxia, 2) spasticity, and 3) global neurodevelopmental impairment. Syndromes that do not fall easily into one of these three categories can be grouped according to the predominant system involved in addition to the neuropathy e.g. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

Imaging Pearls of the Annular Pancreas on Antenatal Scan and Its
Imaging pearls of the annular pancreas on antenatal scan and its diagnostic Case Report dilemma: A case report © 2020, Roul et al Pradeep Kumar Roul,1 Ashish Kaushik,1 Manish Kumar Gupta,2 Poonam Sherwani,1 * Submitted: 22-08-2020 Accepted: 10-09-2020 1 Department of Radiodiagnosis, All India Institute of Medical Sciences, Rishikesh 2 Department of Pediatric Surgery, All India Institute of Medical Sciences, Rishikesh License: This work is licensed under a Creative Commons Attribution 4.0 Correspondence*: Dr. Poonam Sherwani. DNB, EDIR, Fellow Pediatric Radiology, Department of International License. Radiodiagnosis, All India Institute of Medical Sciences, Rishikesh, E-mail: [email protected] DOI: https://doi.org/10.47338/jns.v9.669 KEYWORDS ABSTRACT Annular pancreas, Background: Annular pancreas is an uncommon cause of duodenal obstruction and rarely Duodenal obstruction, causes complete duodenal obstruction. Due to its rarity of identification in the antenatal Double bubble sign, period and overlapping imaging features with other causes of duodenal obstruction; it is Hyperechogenic band often misdiagnosed. Case presentation: A 33-year-old primigravida came for routine antenatal ultrasonography at 28 weeks and 4 days of gestational age. On antenatal ultrasonography, dilated duodenum and stomach were seen giving a double bubble sign and a hyperechoic band surrounding the duodenum. Associated polyhydramnios was also present. Fetal MRI was also done. Postpartum ultrasonography demonstrated pancreatic tissue surrounding the duodenum. The upper gastrointestinal contrast study showed a non-passage of contrast beyond the second part of the duodenum. Due to symptoms of obstruction, the neonate was operated on, and the underlying cause was found to be the annular pancreas. -

RD-Action Matchmaker – Summary of Disease Expertise Recorded Under
Summary of disease expertise recorded via RD-ACTION Matchmaker under each Thematic Grouping and EURORDIS Members’ Thematic Grouping Thematic Reported expertise of those completing the EURORDIS Member perspectives on Grouping matchmaker under each heading Grouping RD Thematically Rare Bone Achondroplasia/Hypochondroplasia Achondroplasia Amelia skeletal dysplasia’s including Achondroplasia/Growth hormone cleidocranial dysostosis, arthrogryposis deficiency/MPS/Turner Brachydactyly chondrodysplasia punctate Fibrous dysplasia of bone Collagenopathy and oncologic disease such as Fibrodysplasia ossificans progressive Li-Fraumeni syndrome Osteogenesis imperfecta Congenital hand and fore-foot conditions Sterno Costo Clavicular Hyperostosis Disorders of Sex Development Duchenne Muscular Dystrophy Ehlers –Danlos syndrome Fibrodysplasia Ossificans Progressiva Growth disorders Hypoparathyroidism Hypophosphatemic rickets & Nutritional Rickets Hypophosphatasia Jeune’s syndrome Limb reduction defects Madelung disease Metabolic Osteoporosis Multiple Hereditary Exostoses Osteogenesis imperfecta Osteoporosis Paediatric Osteoporosis Paget’s disease Phocomelia Pseudohypoparathyroidism Radial dysplasia Skeletal dysplasia Thanatophoric dwarfism Ulna dysplasia Rare Cancer and Adrenocortical tumours Acute monoblastic leukaemia Tumours Carcinoid tumours Brain tumour Craniopharyngioma Colon cancer, familial nonpolyposis Embryonal tumours of CNS Craniopharyngioma Ependymoma Desmoid disease Epithelial thymic tumours in