Al, 1979). Major P
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
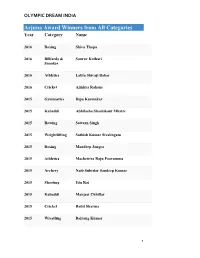
Arjuna Award Winners from All Categories Year Category Name
OLYMPIC DREAM INDIA Arjuna Award Winners from All Categories Year Category Name 2016 Boxing Shiva Thapa 2016 Billiards & Sourav Kothari Snooker 2016 Athletics Lalita Shivaji Babar 2016 Cricket Ajinkya Rahane 2015 Gymnastics Dipa Karmakar 2015 Kabaddi Abhilasha Shashikant Mhatre 2015 Rowing Sawarn Singh 2015 Weightlifting Sathish Kumar Sivalingam 2015 Boxing Mandeep Jangra 2015 Athletics Machettira Raju Poovamma 2015 Archery Naib Subedar Sandeep Kumar 2015 Shooting Jitu Rai 2015 Kabaddi Manjeet Chhillar 2015 Cricket Rohit Sharma 2015 Wrestling Bajrang Kumar 1 OLYMPIC DREAM INDIA 2015 Wrestling Babita Kumari 2015 Wushu Yumnam Sanathoi Devi 2015 Swimming Sharath M. Gayakwad (Paralympic Swimming) 2015 RollerSkating Anup Kumar Yama 2015 Badminton Kidambi Srikanth Nammalwar 2015 Hockey Parattu Raveendran Sreejesh 2014 Weightlifting Renubala Chanu 2014 Archery Abhishek Verma 2014 Athletics Tintu Luka 2014 Cricket Ravichandran Ashwin 2014 Kabaddi Mamta Pujari 2014 Shooting Heena Sidhu 2014 Rowing Saji Thomas 2014 Wrestling Sunil Kumar Rana 2014 Volleyball Tom Joseph 2014 Squash Anaka Alankamony 2014 Basketball Geetu Anna Jose 2 OLYMPIC DREAM INDIA 2014 Badminton Valiyaveetil Diju 2013 Hockey Saba Anjum 2013 Golf Gaganjeet Bhullar 2013 Athletics Ranjith Maheshwari (Athlete) 2013 Cricket Virat Kohli 2013 Archery Chekrovolu Swuro 2013 Badminton Pusarla Venkata Sindhu 2013 Billiards & Rupesh Shah Snooker 2013 Boxing Kavita Chahal 2013 Chess Abhijeet Gupta 2013 Shooting Rajkumari Rathore 2013 Squash Joshna Chinappa 2013 Wrestling Neha Rathi 2013 Wrestling Dharmender Dalal 2013 Athletics Amit Kumar Saroha 2012 Wrestling Narsingh Yadav 2012 Cricket Yuvraj Singh 3 OLYMPIC DREAM INDIA 2012 Swimming Sandeep Sejwal 2012 Billiards & Aditya S. Mehta Snooker 2012 Judo Yashpal Solanki 2012 Boxing Vikas Krishan 2012 Badminton Ashwini Ponnappa 2012 Polo Samir Suhag 2012 Badminton Parupalli Kashyap 2012 Hockey Sardar Singh 2012 Kabaddi Anup Kumar 2012 Wrestling Rajinder Kumar 2012 Wrestling Geeta Phogat 2012 Wushu M. -
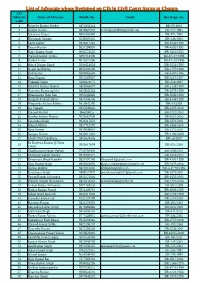
List of Advocate Whose Registred on CIS in Civil Court Saran at Chapra CIS Advocate Name of Advocate Mobile No
List of Advocate whose Registred on CIS in Civil Court Saran at Chapra CIS Advocate Name of Advocate Mobile No. Email Bar Regn. No. Code 1 Birendra Kumar Pandey 9470481114 BR-55/1992 2 Gunjan Verma 9934921847 [email protected] BR-733/1993 3 Mazharul Haque 9905403496 BR-883/1993 4 Bholanath Sharma 9546907435 BR-346/1994 5 Sunil Kumar 9835611348 BR-5740/1995 6 Pawan Kumar 9631594900 BR-4363/1995 7 Rajiv Kumar Singh 8002574542 BR-5310/1995 8 Pramod Kumar Verma 8651814306 BR-10127/1996 9 Pankaj Verma 9835075266 BR-10128/1996 10 Ashok Kumar Singh 9304014624 BR-2631/1996 11 Gopal Jee Pandey 9852088205 BR-2177/1996 12 Kishun Rai 9097962645 BR-8407/1996 13 Renu Kumari 9835268997 BR-3317/1997 14 Tripurari Singh 8292621173 BR-316/1997 15 Birendra Kumar Sharma 8409066877 BR-2124/1998 16 Narendra Kumar pandey 9430945334 BR-3879/1999 17 Dharmendra Nath Sah 9905266646 BR-6243/1999 18 Durgesh Prakash Bihari 9431406306 BR-4144/1999 19 Bhupendra Mohan Mishra 9430945395 BR-68/2009 20 Jay Prakash 9835649645 BR-2397/2010 21 Praveen Kumar 966194025 BR-3132/2003 22 Kundan Kumar Sharma 9525661909 BR-2023/2002 23 Satyendra Singh 9934217633 BR-2870/2001 24 Rakesh Milton 8507718379 BR-1861/2005 25 Ajay Kumar 9939849041 BR-1372/2001 26 Sanjeev Kumar 9430011002 BR-1196/2000 27 Shashi Nath Upadhyay 9430624506 BR-26/1999 Dr Rajeewa Kumar @ Pintu 28 9835617674 BR-951/2000 Tiwari 29 Shashiranjan Kumar Pathak 7739791080 BR-3590/2001 30 Mritunjay Kumar Pandey 9835843533 BR-3316/2003 31 Dineshwer SIngh Kaushik 9931807349 [email protected] BR-4761/1999 32 Ajay -

Athletics, Badminton, Gymnastics, Judo, Swimming, Table Tennis, and Wrestling
INDIVIDUAL GAMES 4 Games and sports are important parts of our lives. They are essential to enjoy overall health and well-being. Sports and games offer numerous advantages and are thus highly recommended for everyone irrespective of their age. Sports with individualistic approach characterised with graceful skills of players are individual sports. Do you like the idea of playing an individual sport and be responsible for your win or loss, success or failure? There are various sports that come under this category. This chapter will help you to enhance your knowledge about Athletics, Badminton, Gymnastics, Judo, Swimming, Table Tennis, and Wrestling. ATHLETICS Running, jumping and throwing are natural and universal forms of human physical expression. Track and field events are the improved versions of all these. These are among the oldest of all sporting competitions. Athletics consist of track and field events. In the track events, competitions of races of different distances are conducted. The different track and field events have their roots in ancient human history. History Ancient Olympic Games are the first recorded examples of organised track and field events. In 776 B.C., in Olympia, Greece, only one event was contested which was known as the stadion footrace. The scope of the games expanded in later years. Further it included running competitions, but the introduction of the Ancient Olympic pentathlon marked a step towards track and field as it is recognised today. There were five events in pentathlon namely—discus throw, long jump, javelin throw, the stadion foot race, and wrestling. 2021-22 Chap-4.indd 49 31-07-2020 15:26:11 50 Health and Physical Education - XI Track and field events were also present at the Pan- Activity 4.1 Athletics at the 1960 Summer Hellenic Games in Greece around 200 B.C. -

VACANCY No.16020311313 Roll No
VACANCY No.16020311313 Roll No. Name Father Name DOB community 1 AASHUTOSH TIWARI RAMESH CHANDRA TIWARI 29-09-1982 GEN 2 ABHA MALIK JITENDRA MALIK 29-05-1989 GEN 3 ABHILASHA SINGH PRAMOD KUMAR SINGH 10-07-1988 GEN 4 ABHINAV VIKRAM BALESHWAR SINGH 27-09-1983 GEN 5 ABHISHEK SINGH PRAHLAD SINGH 18-02-1987 GEN 6 ABHISHEK UPADHYAY BANARASI UPADHYAY 20-12-1988 GEN 7 ABHISHEK KUMAR SINGH ASHOK KUMAR SINGH 02-08-1987 GEN 8 ABHISHEK PRATAP SINGH RAM SINGH 20-04-1986 GEN 9 ABUSAD AHAMAD IMTIYAZ AHAMAD 13-05-1991 GEN 10 AJAY KUMAR MISHRA NIRBHAY NATH MISHRA 10-03-1988 GEN 11 AJAY KUMAR MISHRA NIRBHAY NATH MISHRA 10-03-1988 GEN 12 AJAY VEERBIKRAM SINGH JAY SINGHBAHADUR SINGH 12-09-1988 GEN 13 AJEET KUMAR RAI SAHAJA NAND RAI 12-07-1981 GEN 14 AJIT KUMAR TIWARI SURENDRA NATH TIWARI 09-07-1984 GEN 15 ALKA BAJPAI SUSHIL KUMAR BAJPAI 30-12-1987 GEN 16 ALKA TIWARI AWADHESH TIWARI 03-06-1988 GEN 17 ALKA DNYANESHWAR GHODAKE DNYANESHWAR RAMCHANDRA GHODAKE 01-01-1987 GEN 18 ALOK CHAND SATYA NARAYAN GUPTA 26-08-1988 GEN 19 ALOK MISHRA TRIBHUVAN MISHRA 25-08-1984 GEN 20 ALOK SHARMA MADHAVA PRASAD SHARMA 05-10-1979 GEN 21 ALOK TIWARI AWADHESH TIWARI 05-09-1980 GEN 22 ALOK KUMAR SINGH JANARDAN SINGH 01-10-1986 GEN 23 ALOK KUMAR TIWARI KAPIL DEV TIWARI 10-02-1989 GEN 24 ALOK RANJAN SRIVASTAVA VIJAY PRATAPNARAYAN SRIVASTAVA 11-07-1988 GEN 25 AMAR KUMAR CHOUDHARY RAMANAND CHOUDHARY 02-05-1985 GEN 26 AMARENDRA KUMAR PANDEY RAMESH PRASAD PANDEY 01-09-1985 GEN 27 AMARENDRA KUMAR SRIVASTAVA ISHWAR SHARAN SRIVASTAVA 01-07-1981 GEN 28 AMIT PANDEY PAWAN KUMAR PANDEY 27-01-1992 -

History of Indian Athletics
International Association of Athletics Federations International Association of Athletics Federations Formation 1912 Type Sports federation Headquarters Monaco Membership 212 member federations President Lamine Diack Website http://www.iaaf.org/ The International Association of Athletics Federations (IAAF) is the international governing body for the sport of athletics. It was founded in 1912 at its first congress in Stockholm, Sweden by representatives from 17 national athletics federations as the International Amateur Athletics Federation. Since October 1993 it has been headquartered in Monaco. Beginning in 1982, the IAAF has passed several amendments to its rules allowing athletes to receive compensation for participation in international athletics competitions. However, the IAAF retained the word "amateur" in its name until its 2001 Congress at which the IAAF's title was changed to its current form. The IAAF's current president is Lamine Diack of Senegal. He became Acting President shortly after the death of the previous president, Primo Nebiolo of Italy in November 1999, and was elected IAAF President at the IAAF's 2001 Congress. Presidents Since the establishment of the IAAF, it has had five presidents: Name Country Presidency Sigfrid Edström Sweden 1912±1946 Lord Burghley United Kingdom 1946±1976 Adriaan Paulen Netherlands 1976±1981 Primo Nebiolo Italy 1981±1999 Lamine Diack Senegal 1999± The IAAF has a total of 213 member federations divided into 6 area associations. AAA ± Asian Athletics Association in Asia CAA ± Confédération africaine d'athlétisme in Africa CONSUDATLE ± Confederación Sudamericana de Atletismo in South America EAA ± European Athletic Association in Europe NACACAA ± North American, Central American and Caribbean Athletic Association in North America OAA ± Oceania Athletics Association in Oceania Competitions Included in its charge are the standardization of timekeeping methods and world records. -

1 111130001 Mamata 7739 Bal Vir Singh 38 2 111130002 Mamta
Steno_6952_Stage1 Appeared Srl.No. Roll Number Applicant Full Name Application Seq No Father Full Name Marks Obtained in Written Examination 1 111130001 MAMATA 7739 BAL VIR SINGH 38 2 111130002 MAMTA RAJPUT 4071 PARAM SINGH 41 3 111130003 NAMITA BHATT 10475 VIRENDRA KUMAR BHATT ABSENT 4 111130004 PRIYANKA 633 RAJVEER SINGH 25 5 111130005 DIVYA CHAUHAN 1000 NAPAL SINGH CHAUHAN 48 6 111130006 NEERJA VERMA 8022 VIDHYA SAGAR VERMA 33 7 111130007 ANKITA GAUTAM 2924 SURESH CHAND GAUTAM ABSENT 8 111130008 REKHA SIKARWAR 10676 MOHAR SINGH SIKARWAR 37 9 111130009 ASHU RATHOUR 5506 KAILASH NATH 42 10 111130010 SUNITA YADAV 9797 GABBAR SINGH 39 11 111130011 RASHMI GAUTAM 2907 MOOL CHANDRA 36 12 111130012 ARSHI NOOR 9754 NOORUL HASAN ABSENT 13 111130013 KIRAN 7180 RAMAN PRAKASH 39 14 111130014 KAVITA CHAUDHARY 5406 BHOOP SINGH CHAUDHARY 25 15 111130015 SWATI YADAV 4459 APS YADAV 42 16 111130016 SAPNA YADAV 9536 OM PRAKASH YADAV 31 17 111130017 SEEMA UPRAITI 2473 SATISH UPRAITI 46 18 111130018 SONIYA PATHAK 6466 RAJEEV PATHAK ABSENT 19 111130019 ANSHU RANI 4532 MUKESH BABU 35 20 111130020 KM CHANDRA KALA 6623 CHANDRA PAL SINGH 39 21 111130021 NEETU 5536 SUGHAR SINGH 42 22 111130022 KHUSHBOO JAIN 6963 PRAMOD KUMAR JAIN 41 23 111130023 SANGEETA 10748 RAM PRASAD 40 24 111130024 PRIYANKA YADAV 8413 SUKARAN PAL SINGH 44 25 111130025 KM CHITRA 2872 BHOOPAL SINGH 33 26 111130026 NEELAM KUMARI 2801 UMA SHANKAR 39 27 111130027 PRACHI YADAV 10821 GAYENDRA SINGH YADAV 48 28 111130028 KM RAJNEESH 9453 SONE LAL ABSENT 29 111130029 REKHA RANI VERMA 8648 SHIV DAYAL -

Jabir, Dutee Chand Secure Most World
ATHLETICS FEDERATION OF INDIA NEWSLETTER/Vol.2/AUGUST 2019 AFI honours Dr. Batra Athletics Federation of India became the first body to honour Indian Olympic Association President Dr. Narinder Dhruv Batra for being elected as an International Olympic Committee member. AFI presented him a memento during its annual general meeting in Agra last month. He launched the new-look website of AFI. It has been re-designed for greater navigation comfort and easier access. The Federation asked its members units from States and Union Territories to step up their activities to make track and field sport a more visible option for young athletes. Track & Field legends Sriram Singh & Anju Bobby George unveil Indian Team uniform Indian track and field legends, Sriram Singh and Anju Bobby George were the first to sport the new Team India uniforms at the Athletics Federation of India annual general meeting in Agra on July 18, 2019 Jabir, Dutee Chand secure most World ranking points There can be no doubt that he IAAF World Athletics Championships 2019 in Doha is a key milestone, but the major target for the present lot of athletes is to do well in the Olympic Games and perhaps be among the first to win medals in the greatest celebration of sport. With the relentless support of the Ministry of Youth Affairs and Sports as well as its field arm, Sports Authority of India, the Federation is confident that India’s athletes will get the sustained training and support to reward the country with multiple medals in track and field sport in the Olympic Games in Tokyo next year. -
Doctor of Philosophy
A COMPARATIVE STUDY OF STATE ANXIETY AND SELF-EFFICACY AMONG ATHLETES THESIS SUBMITTED FOR THE AWARD OF THE DEGREE OF Doctor of Philosophy IN PHYSICAL EDUCATION By DILSHAD ALI Under the Supervision of Dr. Kabir Shah Khan DEPARTMENT OF PHYSICAL HEALTH AND SPORTS EDUCATION, ALIGARH MUSLIM UNIVERSITY, ALIGARH-202002, INDIA. 2012 Dedicated to My Parents Department of Physical Health & Sports Education Aligarh Muslim University, Aligarh-202002 (U.P.) Mob. No. 09837265848 Dr. Kabir Shah Khan Associate Professor E-mail: [email protected] Date:……………………….. Certificate This is to certify that the thesis entitled “A COMPARATIVE STUDY OF STATE ANXIETY AND SELF-EFFICACY AMONG ATHLETES” carried out by Mr. Dilshad Ali for the degree of Doctorate of Philosophy in Physical Education under my supervision, is an original contribution and adds substantially to the existing treasure of knowledge in the discipline of physical education and allied sciences. The thesis is fit for submission to the examiners for evaluation. It is further certified that Mr. Dilshad Ali has fulfilled the prescribed conditions of duration and nature given in the Statutes and Ordinances of the Aligarh Muslim University, Aligarh. (Dr. Kabir Shah Khan) Supervisor Acknowledgments First, and foremost, I would like to thank Almighty Allah, for his grace and blessings blustered upon me during this period. Without Him, nothing is possible in the world. No words are adequate to express my sentiments of everlasting gratitude to my venerable teacher and intellectual supervisor Dr. Kabir Shah Khan, Associate Professor, Department of Physical Health & Sports Education, Aligarh Muslim University, Aligarh, under whose continuous guidance, valuable suggestions and encouragement in my work, I am able to complete this thesis. -

SECRETS of PT USHA John Samuel
I AM A WOMAN – SECRETS OF PT USHA John Samuel It was a bright breezy Wednesday in August. Weather in Los Angeles was simply inviting. As the temperature cozily hovered around 20°C the city seemed to be waking up to the audacious dream of an Indian sprinter who had begun life running down the village dust track in coastal Kerala. There was hope in the air and a rugged rhyme in her feet. Exactly at 3.45 p.m. local time, history was in the making at Memorial Coliseum Stadium. Well – almost. Her long strides, fierce pace, the smell of earth all around her and the rhyme from the nearby sea that she had imbibed growing up on the coast – all this conspired to etch her name on the tablet of history as the first Indian woman to win an Olympic medal that languid afternoon. And Pilavullakandi Thekkeparambil Usha of Payyoli fired up the track, timing a career-best 55.42 secs in the 400 m. hurdles. This despite a false start by another competitor jerking her rhythm. Still she missed the bronze by one hundredth of a second. The 20-year-old who tore down the track like a black panther, closed her eyes wiping away tears from her thick eyelashes. Before she knew the whole of India wept for her. She came home without a medal but with new recognition: the queen of the Indian track. Had the judges at the Olympics known that the 12-year-old village girl noticed by coach OM Nambiar at a prize-giving ceremony could not dream of the facilities sprinters else- where in the world took for granted, perhaps they would have given her the medal. -

Physical Education Worksheet 1 Q1
CLASS XI Physical Education Worksheet 1 Q1. Where was the first World Cup Football held? (a) Uruguay (b) France (c) Canada (d) Brazil Q2. Where was the 1998 World Cup Football held? (a) England (b) France (c) Canada (d) South Korea. Q3. In which of the following World Cup Soccer tournaments did maximum number of nations participate? (a) Uruguay 1930 (b) France1998 (c) Both a & b (d) None of the above. Q4. Which two countries have hosted the World Cup Football tournament twice? (a) France and Brazil (b) Mexico and Italy (c) Germany and Japan (d) Argentina and Mexico. Q5. Which country, in the history of hockey, scored maximum number of goals against their opponents? (a) India (b) Pakistan (c) Holland (d) Germany. Q6. In which year was Hockey introduced in the Olympics? (a) 1908, London (b) 1920, Antwerp(c) 1936, Berlin(d) 1956, Melbourne. Q7. When was Hockey introduced in the Asian Games? (a) 1951, Delhi (b) 1954, Manila (c) 1958, Tokyo (d) 1962, Jakarta. Q8. Where are the nest (17th) Commonwealth Games scheduled? (a) Manchester, England(b) Victoria, Canada(c) Kathmandu, Nepal (d) Pusan, S. Korea. Q9. Name of the German game on which the modern basketball has been based is (a) Handball (b) korfball (c) Hockey (d) volleyball. Q10. Which of the following stadiums was known as Irwin Amphitheatre? (a) National Stadium, Delhi (b) Yuba Bharti Kridangan, Calcutta (c) Jawaharlal Lai Nehru Stadium, Delhi (d) None of the above. Q11. Sport Authority of India was formed in (a) 1983 (b) 1984 (c) 1985 (d) 1986. Q12. ‘Michael Ferreira’ is associated with the game of (a) Snooker (b) billiards (c) Golf (d) equestrian. -

57Th National Open Athletics Championships 2017 LICENSED TO
LICENSED TO: ATHLETICS FEDERATION OF INDIA Page 1 of 23 57th National Open Athletics Championships 2017 CHENNAI, TAMILNADU 28-Sep-17 9/25/17 - 9/28/17 25-28 SEPTEMBER 2017 Event # 1 MENS 100m Run #NR:A.KUMAR MALLICK NEW DELHI # 10.26 28/04/2016 % MR:ANIL KUMAR CHENNAI 10.37 2001 RESULTS OF FINALS 1 MD SADATH 842 30-03-97 SERVICES +0.0m/s 10.57 10.565 2 ELAKKIYADASAN . 899 31-01-95 TAMILNADU +0.0m/s 10.57 10.570 3 VIDYA SAGAR 843 10-06-92 SERVICES +0.0m/s 10.60 4 ANUROOP JOHN 455 15-02-91 KERALA +0.0m/s 10.64 5 SATNAM SINGH 856 27-03-91 SERVICES +0.0m/s 10.65 10.644 6 PRAVEEN MUTHU KUMAR 920 15-03-93 TAMILNADU +0.0m/s 10.65 10.649 7 CH SUDHAKAR 626 18-05-97 ONGC +0.0m/s 10.67 8 MOHIT K 742 RAILWAYS +0.0m/s 10.99 Event # 2 MENS 200m Run # NR:DHARAMBIR SINGH WUHAN 20.66 07/06/2015 % MR:S. ARUNJITH JAMSHEDPUR 20.92 2007 RESULTS OF FINALS 1 VIDYA SAGAR 843 10-06-92 SERVICES 21.46 2 PARVEEN . 333 19-02-90 HARYANA 21.49 3 K ASHOK 817 10-04-93 SERVICES 21.53 4 NITHIN . 906 04-12-99 TAMILNADU 21.87 5 SIVAKUMAR . 910 13-10-94 TAMILNADU 22.06 6 MOHIT K 742 RAILWAYS 22.21 7 SAFIKUL MONDAL 1036 08-07-96 WEST BENGAL 22.28 8 MOHAN KUMAR 603 14-12-96 ONGC 22.77 Event # 3 MENS 400m Run # NR:MUHAMMED ANAS NEW DELHI # 45.32 15/05/2017 % MR:AROCKYA RAJIV KOLKATA 45.70 2015 RESULTS OF FINALS 1 JITHU BABY 822 01-04-93 SERVICES 47.08 2 MOHAN KUMAR 603 14-12-96 ONGC 47.17 3 RAVINDER. -

Sports in India Introduction the History of Sports in India Dates Back to the Vedic Era
Sports in India Introduction The history of sports in India dates back to the Vedic era. Physical culture in ancient India was important and is mentioned in our great epics. In the Ramayana and Mahabharata warriors were trained as archers and were also adept at physical contact sports like wrestling. Today, sports are an important part of theIndian culture and contribute in many ways to the Indian economy. While India excels in many sports that originated outside the subcontinent, such as cricket and football, there are also sports that were invented in India that India frequently participates in. Even though the leading sport in the country remains cricket, the establishment of new leagues in football, hockey, kabaddi and other less popular sports has helped players to get global exposure. International Sporting Events organised in India In 1951 the very first Asian Games were organised in Delhi. Subsequently the Asian Games were held in New Delhi again in 1982. The Commonwealth Games were organised at Delhi in 2010. The Cricket World Cup was held in India in 1987 and 1996 (jointly with Pakistan and Sri Lanka) and in 2011 (jointly with Bangladesh and Sri Lanka). The FIFA Under-17World Cup for men was held at Delhi in 2017. Individual Sports Athletics The Athletics Federation of India is the apex body for running and managing athletics in India and affiliated to the IAAF, AAA and Indian Olympic Association. Indian athletics has a rich heritage and an enviable track record in more than 75 years of its existence. The sport has contributed the bulk of the medal haul for the Indian contingent at the Asian Games since 1951.