1- Anticholinergic Drugs.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Table 2. 2012 AGS Beers Criteria for Potentially
Table 2. 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults Strength of Organ System/ Recommendat Quality of Recomm Therapeutic Category/Drug(s) Rationale ion Evidence endation References Anticholinergics (excludes TCAs) First-generation antihistamines Highly anticholinergic; Avoid Hydroxyzin Strong Agostini 2001 (as single agent or as part of clearance reduced with e and Boustani 2007 combination products) advanced age, and promethazi Guaiana 2010 Brompheniramine tolerance develops ne: high; Han 2001 Carbinoxamine when used as hypnotic; All others: Rudolph 2008 Chlorpheniramine increased risk of moderate Clemastine confusion, dry mouth, Cyproheptadine constipation, and other Dexbrompheniramine anticholinergic Dexchlorpheniramine effects/toxicity. Diphenhydramine (oral) Doxylamine Use of diphenhydramine in Hydroxyzine special situations such Promethazine as acute treatment of Triprolidine severe allergic reaction may be appropriate. Antiparkinson agents Not recommended for Avoid Moderate Strong Rudolph 2008 Benztropine (oral) prevention of Trihexyphenidyl extrapyramidal symptoms with antipsychotics; more effective agents available for treatment of Parkinson disease. Antispasmodics Highly anticholinergic, Avoid Moderate Strong Lechevallier- Belladonna alkaloids uncertain except in Michel 2005 Clidinium-chlordiazepoxide effectiveness. short-term Rudolph 2008 Dicyclomine palliative Hyoscyamine care to Propantheline decrease Scopolamine oral secretions. Antithrombotics Dipyridamole, oral short-acting* May -

Appendix A: Potentially Inappropriate Prescriptions (Pips) for Older People (Modified from ‘STOPP/START 2’ O’Mahony Et Al 2014)
Appendix A: Potentially Inappropriate Prescriptions (PIPs) for older people (modified from ‘STOPP/START 2’ O’Mahony et al 2014) Consider holding (or deprescribing - consult with patient): 1. Any drug prescribed without an evidence-based clinical indication 2. Any drug prescribed beyond the recommended duration, where well-defined 3. Any duplicate drug class (optimise monotherapy) Avoid hazardous combinations e.g.: 1. The Triple Whammy: NSAID + ACE/ARB + diuretic in all ≥ 65 year olds (NHS Scotland 2015) 2. Sick Day Rules drugs: Metformin or ACEi/ARB or a diuretic or NSAID in ≥ 65 year olds presenting with dehydration and/or acute kidney injury (AKI) (NHS Scotland 2015) 3. Anticholinergic Burden (ACB): Any additional medicine with anticholinergic properties when already on an Anticholinergic/antimuscarinic (listed overleaf) in > 65 year olds (risk of falls, increased anticholinergic toxicity: confusion, agitation, acute glaucoma, urinary retention, constipation). The following are known to contribute to the ACB: Amantadine Antidepressants, tricyclic: Amitriptyline, Clomipramine, Dosulepin, Doxepin, Imipramine, Nortriptyline, Trimipramine and SSRIs: Fluoxetine, Paroxetine Antihistamines, first generation (sedating): Clemastine, Chlorphenamine, Cyproheptadine, Diphenhydramine/-hydrinate, Hydroxyzine, Promethazine; also Cetirizine, Loratidine Antipsychotics: especially Clozapine, Fluphenazine, Haloperidol, Olanzepine, and phenothiazines e.g. Prochlorperazine, Trifluoperazine Baclofen Carbamazepine Disopyramide Loperamide Oxcarbazepine Pethidine -

Ketamine As a General Anesthesia Adjunct Michaela Wilcox, DNP
Ketamine as a General Anesthesia Adjunct Michaela Wilcox, DNP (c), RN Dept. of Nurse Anesthesia, Moffett & Sanders School of Nursing, Samford University Structured Abstract Background Ketamine is a unique anesthetic agent with both anesthetic and analgesic properties. Ketamine is primarily a N-Methyl-D-Aspartic acid (NMDA) antagonist that also works on glutamine, nicotinic, muscarinic, monoaminergic and opioid receptors. The uses of ketamine are numerous and include treatment of chronic pain, acute pain, depression, as a multimodal pain adjunct, opioid-sparing agent and as an adjunct in enhanced recovery after surgery (ERAS) protocols. A 49-year-old female presented for a lumbar lateral interbody fusion extreme, anterior lumbar spine arthrodesis L3/4 with revision and instrumentation. Based on the surgical need for both sensory and motor nerve monitoring intraoperatively, the anesthetic plan included minimal sevoflurane, succinylcholine for induction and a propofol intravenous (IV) infusion with boluses of ketamine to maintain unconsciousness. A bispectral index (BIS) monitor (Aspect Medical Systems, Natick, MA) was placed on the patient’s forehead prior to induction and utilized intraoperatively to maintain a goal of 40-60. General anesthesia was achieved with fentanyl 100 mcg, lidocaine 100 mg, propofol 200 mg, ketamine 50 mg and succinylcholine 160 mg IV. Laryngoscopy was successfully performed using a McGrath MAC video laryngoscope (Medtronic, Minneapolis, MN). Following induction, a propofol IV infusion was initiated and sevoflurane maintained at 0.3 minimum alveolar concentration. Ketamine 10 mg IV was administered every hour. Upon conclusion of the procedure, the patient was extubated and transported to postoperative recovery unit, where she had no complaints of nausea, vomiting or pain. -

(Antimuscarinic) Drugs?
© July - August 2018 How well do you know your anticholinergic (antimuscarinic) drugs? nticholinergic drugs, prescribed for a variety of clini- Acal conditions, are amongst the most frequently used prescription drugs in BC (Table 1). Also referred to as “an- timuscarinics,” such drugs specifically block muscarinic receptors for acetylcholine (ACh).1 Muscarinic ACh recep- tors are important in the parasympathetic nervous system that governs heart rate, exocrine glands, smooth muscles, clude drugs whose active metabolites are potent- as well as brain function. In contrast, nicotinic ACh recep- ly antimuscarinic,5 or which often cause typical tors stimulate contraction of striated muscles. This Letter is AC adverse effects such as dry mouth or urinary intended to remind clinicians of commonly used drugs that retention.6 People taking antihistamines, antide- have anticholinergic (AC), or technically, antimuscarinic pressants, antipsychotics, opioids, antimuscarinic properties, and of their potential adverse effects. inhalers, or many other drugs need to know that Beneficial and harmful effects of anticholinergic drugs have blockade of ACh receptors can cause bothersome been known for centuries. In Homer’s Odyssey, the nymph or even dangerous adverse effects (Table 3). pharmacologist Circe utilized central effects of atropinics Subtle and not-so-subtle toxicity in the common plant jimson weed (Datura stramonium) to cause delusions in the crew of Odysseus. Believing they Students often learn the adverse effects of anticho- had been turned into pigs, they could be herded.2 linergics from a mnemonic, e.g.: “Blind as a bat, Sometimes a drug is recommended specifically for its an- mad as a hatter, red as a beet, hot as a hare, dry as ticholinergic potency. -

Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5
ANTICHOLINERGICS: Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5 J Bareham BSP © www.RxFiles.ca Aug 2021 WHENEVER POSSIBLE, AVOID DRUGS WITH MODERATE TO HIGH ANTICHOLINERGIC ACTIVITY IN OLDER ADULTS (>65 YEARS OF AGE) Low Anticholinergic Activity; Moderate/High Anticholinergic Activity -B in combo Beers Antibiotics Antiparkinsonian Cardiovascular Agents Immunosuppressants ampicillin *ALL AVAILABLE AS amantadine SYMMETREL atenolol TENORMIN azaTHIOprine IMURAN cefOXitin GENERIC benztropine mesylate COGENTIN captopril CAPOTEN cyclosporine NEORAL clindamycin bromocriptine PARLODEL chlorthalidone GENERIC ONLY hydrocortisone CORTEF gentamicin (Oint & Sol’n NIHB covered) carbidopa/levodopa SINEMET digoxin LANOXIN, TOLOXIN methylprednisolone MEDROL piperacillin entacapone COMTAN dilTIAZem CARDIZEM, TIAZAC prednisone WINPRED dipyridamole PERSANTINE, ethopropazine PARSITAN vancomycin phenelzine NARDIL AGGRENOX disopyramide RYTHMODAN Muscle Relaxants pramipexole MIRAPEX Antidepressants baclofen LIORESAL ( on intrathecal only) procyclidine KEMADRIN furosemide LASIX amitriptyline ELAVIL cyclobenzaprine FLEXERIL selegiline ELDEPRYL hydrALAZINE APRESOLINE clomiPRAMINE ANAFRANIL isosorbide ISORDIL methocarbamol ROBAXIN OTC trihexyphenidyl ARTANE desipramine NORPRAMIN metoprolol LOPRESOR orphenadrine NORFLEX OTC doxepin >6mg SINEQUAN Antipsychotics NIFEdipine ADALAT tiZANidine ZANAFLEX A imipramine TOFRANIL quiNIDine GENERIC ONLY C ARIPiprazole ABILIFY & MAINTENA -

The Role of Antispasmodics in Managing Irritable Bowel Syndrome
DOI: https://doi.org/10.22516/25007440.309 Review articles The role of antispasmodics in managing irritable bowel syndrome Valeria Atenea Costa Barney,1* Alan Felipe Ovalle Hernández.1 1 Internal Medicine and Gastroenterology specialist Abstract in San Ignacio University Hospital, Pontificia Universidad Javeriana, Bogotá, Colombia. Although antispasmodics are the cornerstone of treating irritable bowel syndrome, there are a number of an- tispasmodic medications currently available in Colombia. Since they are frequently used to treat this disease, *Correspondence: [email protected] we consider an evaluation of them to be important. ......................................... Received: 26/10/18 Keywords Accepted: 11/02/19 Antispasmodic, irritable bowel syndrome, pinaverium bromide, otilonium bromide, Mebeverin, trimebutine. INTRODUCTION consistency. The criteria must be met for three consecutive months prior to diagnosis and symptoms must have started Irritable bowel syndrome (IBS) is one of the most fre- a minimum of six months before diagnosis. (3, 4) quent chronic gastrointestinal functional disorders. It is There are no known structural or anatomical explanations characterized by recurrent abdominal pain associated with of the pathophysiology of IBS and its exact cause remains changes in the rhythm of bowel movements with either or unknown. Nevertheless, several mechanisms have been both constipation and diarrhea. Swelling and bloating are proposed. Altered gastrointestinal motility may contribute frequent occurrences. (1) to changes in bowel habits reported by some patients, and a IBS is divided into two subtypes: predominance of cons- combination of smooth muscle spasms, visceral hypersen- tipation (20-30% of patients) and predominance of dia- sitivity and abnormalities of central pain processing may rrhea (20-30% of patients). -
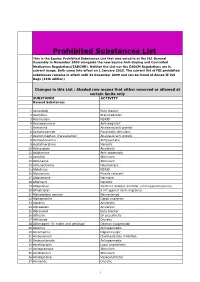
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Anesthesia and Analgesia in Laboratory Animals
GUIDELINES ON ANESTHESIA AND ANALGESIA IN LABORATORY ANIMALS University of South Florida provides the following guidelines for use by IACUC-certified faculty and staff. CONTENTS PAGE A. Background……………………………………………………….…………………………… 1 B. Definitions....……………………………………………………..…………………………….. 2 C. General Considerations……………………………………….,…………………………….. 3 D. Controlled Substances……………………………………….……………………………… 3 E. Pre-Anesthetic Treatments………………………………….………………………………. 4 F. General Anesthetics………………………………………….………………………………. 4 G. Neuromuscular Blocking Agents………………………….……………………………….. 5 H. Monitoring Anesthesia…………………………………….…………………………………. 6 I. Analgesics……………………………………………………………………………………… 7 J. Comments regarding Anesthetics and Analgesics……………………………………... 7 REFERENCE TABLES PAGE I. Signs of Pain and Distress in Laboratory Animals………………………………………… 10 II. Commonly Used Anesthetics and Analgesics for Mice….………..…...….………...…… 11 III. Commonly Used Anesthetics and Analgesics for Rats……………………………...…… 12 IV. Commonly Used Anesthetics and Analgesics for Gerbils……….……………..…….. 13 V. Commonly Used Anesthetics and Analgesics for Hamsters…….……………..……. 14 VI. Commonly Used Anesthetics and Analgesics for Guinea Pigs….…………….….……. 15 VII. Commonly Used Anesthetics and Analgesics for Rabbits.……...…………….………… 16 VIII. Commonly Used Anesthetics and Analgesics for Dogs.…………………….…………… 17 IX. Commonly Used Anesthetics and Analgesics for Cats.……………………..…………… 18 X. Commonly Used Anesthetics and Analgesics for Pigs ..……………..….………………..19 XI. Commonly Used Anesthetics and Analgesics -

Metered-Dose Inhalers (Mdis): Anti-Cholinergic Drugs
Texas Vendor Drug Program Drug Use Criteria: Aerosolized Agents - Metered-Dose Inhalers (MDIs): Anti-Cholinergic Drugs Publication History 1. Developed January 1995. 2. Revised April 2021; March 2019; March 2017; November 2015; March 2014; August 2012; June 2012; October 2010; January 2008; January 2003; January 2002; January 2001; March 2000; January 2000; February 1999; February 1998; February 1997; August 1995. Notes: All criteria may be applied retrospectively. The information contained is for the convenience of the public. The Texas Health and Human Services Commission is not responsible for any errors in transmission or any errors or omissions in the document. Medications listed in the tables and non-FDA approved indications included in these retrospective criteria are not indicative of Vendor Drug Program formulary coverage. Prepared by: • Drug Information Service, UT Health San Antonio. • The College of Pharmacy, The University of Texas at Austin 1 1 Dosage 1.1 Adults Ipratropium (Atrovent®), a short-acting, inhalational anticholinergic agent, is FDA- approved to manage bronchospasm associated with chronic bronchitis and emphysema, collectively known as chronic obstructive pulmonary disease (COPD). Ipratropium is considered a second-line agent in the treatment of asthma as the bronchodilatory effects seen with ipratropium are less than those seen with beta- adrenergic drugs. While not FDA approved, the Expert Panel 3 guidelines from the National Heart Lung and Blood Institute document benefit when multiple ipratropium doses are administered adjunctively with beta2-agonists in the emergency department to manage more severe acute asthma exacerbations, and the Global Initiative for Asthma (GINA) guidelines state that ipratropium may be considered an alternative bronchodilator in patients who experience adverse effects to short-acting beta2-agonists (e.g., tachycardia, arrhythmia, tremor). -

CONTRAINDICATIONS ------Pediatric Patients (486 on DETROL LA, 224 on Placebo) Is Available
HIGHLIGHTS OF PRESCRIBING INFORMATION • Controlled Narrow-Angle Glaucoma: use caution in patients being These highlights do not include all the information needed to use Detrol® treated for narrow-angle glaucoma. (5.3) LA safely and effectively. See full prescribing information for Detrol LA. • Myasthenia Gravis: use caution in patients with myasthenia gravis. (5.6) • QT Prolongation: Consider observations from the thorough QT study in ® Detrol LA (tolterodine tartrate extended release capsules) clinical decisions to prescribe DETROL LA to patients with a known For oral administration history of QT prolongation or to patients who are taking Class IA (e.g., Initial U.S. Approval: December 2000 quinidine, procainamide) or Class III (e.g., amiodarone, sotalol) antiarrhythmic medications (5.7) ----------------------------INDICATIONS AND USAGE--------------------------- Detrol LA is an antimuscarinic indicated for the treatment of overactive ------------------------------ADVERSE REACTIONS------------------------------- bladder with symptoms of urge urinary incontinence, urgency, and frequency. The most common adverse reactions (incidence >4% and >placebo) were dry (1) mouth , headache, constipation and abdominal pain. (6.1) ----------------------DOSAGE AND ADMINISTRATION----------------------- • 4 mg capsules taken orally once daily with water and swallowed To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at whole. (2.1) 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. • 2 mg capsules taken orally once daily with water and swallowed whole in the presence of: ------------------------------DRUG INTERACTIONS------------------------------- o mild to moderate hepatic impairment (Child-Pugh • Potent CYP3A4 inhibitors: Co-administration may increase systemic class A or B) (2.2) exposure to DETROL LA. Reduce DETROL LA dose to 2 mg once o severe renal impairment [Creatinine Clearance (CCr) daily. -

Anticholinergic Drugs Toxicity
Prescription drug toxicity Anticholinergic drug toxicity Anticholinergic syndrome is produced by the inhibition of cholinergic neurotransmission at muscarinic receptor sites. It commonly follows the ingestion of a wide variety of prescription and over-the-counter medications. Signs and symptoms Clinical manifestations are caused by CNS effects, peripheral nervous system effects, or both. Common manifestations are as follows: Flushing Dry skin and mucous membranes Mydriasis with loss of accommodation Altered mental status Fever Additional manifestations include the following: Sinus tachycardia Decreased bowel sounds Urinary retention Hypertension Pathophysiology Substances with anticholinergic properties competitively antagonize acetylcholine muscarinic receptors; this predominantly occurs at peripheral (eg, heart, salivary glands, sweat glands, GI tract, urinary tract) postganglionic parasympathetic muscarinic receptors. Anticholinergic substances minimally compete with acetylcholine at other sites (eg, autonomic ganglia). Central nervous system manifestations result from central cortical and subcortical muscarinic receptor antagonism. The degree of CNS manifestation is related to the drug's ability to cross the blood-brain barrier. 1 Agents with anticholinergic properties are as follows: Anticholinergics o Atropine, scopolamine Antihistamines o Chlorpheniramine o Cyproheptadine o Diphenhydramine o Promethazine Antipsychotics o Chlorpromazine o Clozapine o Thioridazine Antispasmodics o Clidinium o Hyoscyamine o Propantheline -

(Cholinergic Antagonists) (Anticholinergic ) (Cholinergic
Parasympathlytic (Cholinergic antagonists) (Anticholinergic ) (Cholinergic Blockers) A- antimuscarinic agents (Muscarinic Antagonists): " Agents with high binding affinity for muscarinic receptors but no intrinsic activity. Pharmacologic effects opposite of the muscarinic agonists. " Competitive (reversible) antagonists of ACh " Antagonistic responses include: decreased contraction of GI and urinary tract smooth muscles, dilation of pupils, reduced gastric secretion, decreased saliva secretion. A- antimuscarinic agents (Muscarinic Antagonists): 1-Atropine (belladonna alkaloid) " (Competitive inhibitors) . -bind to muscarinic receptors and prevent Ach binding. " reversible blockade of ACh at muscarinic receptors by competitive binding! -reversal effect of atropine by increasing ACh or agonist ----> decreased blockade -atropine is central & peripheral muscarinic blocker. Muscarinic receptor blockade does not interfere with transmission at autonomic ganglionic sites, the adrenal medulla, or skeletal muscle fibers. Sympathetic adrenergic functions are not affected. X X MUSCARINIC RECEPTOR BLOCKADE ALLOWS SYMPATHETIC DOMINANCE IN DUAL INNERVATED ORGANS X Atropine actions "Eye: *mydriasis *unresponsiveness to light *cycloplegia *increase IOP " GIT: reduce activity of GIT. " Urinary system: reduce hyper motility. " Cardiovascular system: at low dose bradycardia at high dose tachycardia " Secretions: reduce secretions Therapeutic uses of atropine 1-Ophthalmic: Ophthalmologic examinations. mydriatic & cycloplegic effects. 2-antispasmotic agent