Critical Care and Resuscitation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Detection and Determination of Esters
Louisiana State University LSU Digital Commons LSU Historical Dissertations and Theses Graduate School 1958 The etD ection and Determination of Esters. Mohd. Mohsin Qureshi Louisiana State University and Agricultural & Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_disstheses Recommended Citation Qureshi, Mohd. Mohsin, "The eD tection and Determination of Esters." (1958). LSU Historical Dissertations and Theses. 501. https://digitalcommons.lsu.edu/gradschool_disstheses/501 This Dissertation is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Historical Dissertations and Theses by an authorized administrator of LSU Digital Commons. For more information, please contact [email protected]. Copright by Mohcl Mohsin Qureshi 1959 THE DETECTION AND DETERMINATION OF ESTERS A Dissertation Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Doctor of Philosophy in The Department of Chemistry by Mohd. Mohsin Qureshi M.Sc., Aligarh University, 1944 August, 1958 ACKNOWLEDGMENT The author wishes to express his sincere apprecia tion and gratitude to Dr. Philip W. West under whose guidance this research was carried out. He is grateful to Dr. James G. Traynham for sup plying him with a number of esters and for his many helpful suggestions. The financial support given to him by the Continental Oil Company is gratefully acknowledged. He offers his sincere thanks to Miss Magdalena Usategul for her valuable suggestions and her ungrudging help during the course of this investigation. Dr. Anil K. -

Molecular Dynamics Simulations in Drug Discovery and Pharmaceutical Development
processes Review Molecular Dynamics Simulations in Drug Discovery and Pharmaceutical Development Outi M. H. Salo-Ahen 1,2,* , Ida Alanko 1,2, Rajendra Bhadane 1,2 , Alexandre M. J. J. Bonvin 3,* , Rodrigo Vargas Honorato 3, Shakhawath Hossain 4 , André H. Juffer 5 , Aleksei Kabedev 4, Maija Lahtela-Kakkonen 6, Anders Støttrup Larsen 7, Eveline Lescrinier 8 , Parthiban Marimuthu 1,2 , Muhammad Usman Mirza 8 , Ghulam Mustafa 9, Ariane Nunes-Alves 10,11,* , Tatu Pantsar 6,12, Atefeh Saadabadi 1,2 , Kalaimathy Singaravelu 13 and Michiel Vanmeert 8 1 Pharmaceutical Sciences Laboratory (Pharmacy), Åbo Akademi University, Tykistökatu 6 A, Biocity, FI-20520 Turku, Finland; ida.alanko@abo.fi (I.A.); rajendra.bhadane@abo.fi (R.B.); parthiban.marimuthu@abo.fi (P.M.); atefeh.saadabadi@abo.fi (A.S.) 2 Structural Bioinformatics Laboratory (Biochemistry), Åbo Akademi University, Tykistökatu 6 A, Biocity, FI-20520 Turku, Finland 3 Faculty of Science-Chemistry, Bijvoet Center for Biomolecular Research, Utrecht University, 3584 CH Utrecht, The Netherlands; [email protected] 4 Swedish Drug Delivery Forum (SDDF), Department of Pharmacy, Uppsala Biomedical Center, Uppsala University, 751 23 Uppsala, Sweden; [email protected] (S.H.); [email protected] (A.K.) 5 Biocenter Oulu & Faculty of Biochemistry and Molecular Medicine, University of Oulu, Aapistie 7 A, FI-90014 Oulu, Finland; andre.juffer@oulu.fi 6 School of Pharmacy, University of Eastern Finland, FI-70210 Kuopio, Finland; maija.lahtela-kakkonen@uef.fi (M.L.-K.); tatu.pantsar@uef.fi -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Extraction and Evaporation: Experiment 1 Separating the Components of a Mixture1 Week 1
Organic Chemistry I Laboratory Extraction and Evaporation: Experiment 1 Separating the Components of a Mixture1 Week 1 Background Reading Zubrick, J. W. The Organic Chem Lab Survival Manual, 4th edition, Wiley & Sons, Inc., New York, 1997. Keeping a Notebook: Pg 12-24. Interpreting Handbooks: Pg 26-31, 34-44. Extraction and Washing: Pg 148-168. Background Senario One of the many places organic chemists are employed is in private laboratories associated with consulting firms. The purpose of these labs is generally to provide chemical analysis or synthesis of material for customers. The first few labs in CHM 220 will teach you the basic techniques needed to analyze and purify mixtures to determine the individual components. This first lab will involve determining the composition of a possible pharmaceutical preparation. Watchdog agencies exist which monitor the pharmaceuticals sold over the counter in the United States. These agencies will use private laboratory firms to analyze products suspected of violating enforced standards. For example, a new brand of analgesic may appear on drugstore shelves at a low price. The label indicates that the tablets were manufactured in the United States by a legitimate pharmaceutical company. However, the labels may reveal discrepancies and the appearance/quality of the tablets could lead an investigator to suspect that they might be counterfeit. Such knockoffs of a domestic product can be manufactured cheaply elsewhere and smuggled into the US, where they are sold for high profits. This laboratory exercise places you in the position of analyzing a suspected counterfeit analgesic preparation. The label on the suspected bottle lists the ingredients per tablet as aspirin (200 mg), acetaminophen (250 mg), and sucrose (50 mg). -

Actarit (Rinn) Severe, Active Rheumatoid Arthritis and Active and Ацеметацин Actaritum; MS-932
Abatacept/Adalimumab 15 Preparations Acetanilide concentrations are reached in about 3 to 8 days and bio- Proprietary Preparations (details are given in Part 3) Acetanilida; Antifebrin. N-Phenylacetamide. availability is estimated to be 64%. The mean terminal Arg.: Berlofen; Bristaflam†; Austria: Beofenac†; Belg.: Air-Tal; Biofenac; Антифебрин; Ацетанилид half-life is about 2 weeks. Braz.: Aceflan†; Cecoflan†; Proflam; Chile: Airtal†; Bristaflam†; Denm.: C8H9NO = 135.2. ◊ References. Barcan; Fin.: Barcan; Fr.: Cartrex; Ger.: Beofenac; Gr.: Aceclonac; Arlina; CAS — 103-84-4. Biofenac; Sovipan; Hung.: Aflamin; India: Aceclo; Arrestin; Movon; Zero- 1. Nestorov I. Clinical pharmacokinetics of tumor necrosis factor dol; Ital.: Airtal; Gladio; Kafenac; Mex.: Bristaflam; Neth.: Biofenac; Norw.: antagonists. J Rheumatol 2005; 74 (suppl): 13–18. Barcan; Philipp.: Clanza; Port.: Airtal; Biofenac; Rus.: Airtal (Аэртал); Spain: Airtal; Airtal Difucrem; Falcol; Gerbin; Sanein; Swed.: Barcan; Switz.: Locomin†; UAE: Aceclofar; UK: Preservex; Venez.: Airtal†; Brista- O Uses and Administration flam. Adalimumab is a recombinant human monoclonal tumour necrosis factor (TNF) antibody that binds Multi-ingredient: India: Kinectine; Kinectine P; Kinectine-MR; Movon- N CH3 MR; Movon-P†; Zerodol-MR; Zerodol-P. H specifically to TNF-α and blocks its interaction with endogenous cell-surface TNF receptors. It also modu- Pharmacopoeias. In Fr. lates biological responses that are induced or regulated Profile by TNF. Elevated levels of TNF have been found in the Acemetacin (BAN, rINN) Acetanilide, a para-aminophenol derivative related to paraceta- affected tissues and fluids of patients with rheumatoid Acemetacina; Acémétacine; Acemetacinum; Asemetasin; Bay-f- mol (p.108), has analgesic and antipyretic properties. It was re- placed by safer analgesics. -

Thermodynamics of Mixing of Sodium Naproxen and Procaine Hydrochloride in Ethanol + Water Cosolvent Mixtures
Rev. Colomb. Cienc. Quím. Farm., Vol. 39 (2), 132-148, 2010 www.farmacia.unal.edu.co Artículo de investigación científica Thermodynamics of mixing of sodium naproxen and procaine hydrochloride in ethanol + water cosolvent mixtures Daniel R. Delgado1, Reinaldo G. Sotomayor2, Diego R. Monterroza2, Carolina P. Mora3, Edgar F. Vargas4, Fleming Martínez5* 1 Centro de Investigaciones, Corporación Universitaria Iberoamericana, Bogotá, D. C., Colombia. 2 Laboratorios Procaps, Barranquilla, Colombia. 3 Grupo de Investigaciones Natura, Departamento de Química Farmacéutica, Facultad de Ciencias Naturales, Universidad Icesi, Santiago de Cali, Colombia. 4 Grupo de Termodinámica de Soluciones, Departamento de Química, Facultad de Ciencias, Universidad de los Andes, Bogotá, D. C., Colombia. 5 Grupo de Investigaciones Farmacéutico-Fisicoquímicas, Departamento de Farmacia, Facultad de Ciencias, Universidad Nacional de Colombia, A. A. 14490, Bogotá, D. C., Colombia. * Corresponding Author: E-mail: [email protected]. Recibido para evaluación: 25 de septiembre de 2010 Aceptado para publicación: 15 de octubre de 2010 Summary Thermodynamic functions Gibbs energy, enthalpy, and entropy of mixing of sodium naproxen and procaine hydrochloride were evaluated. Mixing quantities were calculated based on fusion calorimetric values obtained from differential scan- ning calorimetry measurements and equilibrium solubility values reported in the literature for both drugs in ethanol + water mixtures. By means of enthalpy-entropy 0 0 compensation analysis, non-linear ∆H mix vs. Gmix plots were obtained which indi- cates different mechanisms involved in the dissolution of these drugs according to mixtures composition. Nevertheless, the molecular and ionic events involved in the dissolution of this drug in this cosolvent system are unclear. Keywords: sodium naproxen, procaine hydrochloride, mixing process, cosolvency, ethanol, solution thermodynamics. -
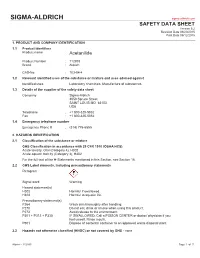
SIGMA-ALDRICH Sigma-Aldrich.Com SAFETY DATA SHEET Version 5.2 Revision Date 03/20/2015 Print Date 05/12/2015
SIGMA-ALDRICH sigma-aldrich.com SAFETY DATA SHEET Version 5.2 Revision Date 03/20/2015 Print Date 05/12/2015 1. PRODUCT AND COMPANY IDENTIFICATION 1.1 Product identifiers Product name : Acetanilide Product Number : 112933 Brand : Aldrich CAS-No. : 103-84-4 1.2 Relevant identified uses of the substance or mixture and uses advised against Identified uses : Laboratory chemicals, Manufacture of substances 1.3 Details of the supplier of the safety data sheet Company : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 1.4 Emergency telephone number Emergency Phone # : (314) 776-6555 2. HAZARDS IDENTIFICATION 2.1 Classification of the substance or mixture GHS Classification in accordance with 29 CFR 1910 (OSHA HCS) Acute toxicity, Oral (Category 4), H302 Acute aquatic toxicity (Category 3), H402 For the full text of the H-Statements mentioned in this Section, see Section 16. 2.2 GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. H402 Harmful to aquatic life. Precautionary statement(s) P264 Wash skin thoroughly after handling. P270 Do not eat, drink or smoke when using this product. P273 Avoid release to the environment. P301 + P312 + P330 IF SWALLOWED: Call a POISON CENTER or doctor/ physician if you feel unwell. Rinse mouth. P501 Dispose of contents/ container to an approved waste disposal plant. 2.3 Hazards not otherwise classified (HNOC) or not covered by GHS - none Aldrich - 112933 Page 1 of 7 3. COMPOSITION/INFORMATION ON INGREDIENTS 3.1 Substances Synonyms : N-Phenylacetamide Formula : C8H9NO Molecular weight : 135.16 g/mol CAS-No. -

Laboratory Manual
International Program UAM-Boston University Laboratory Manual Organic Chemistry I 2013-2014 Departamento de Química Orgánica Ernesto Brunet Romero Ana María Martín Castro Ramón Gómez Arrayás Laboratory Manual Table of Contents ............................................................................... 1 Introduction ............................................................................... 2 Prelab preparation ............................................................................... 2 Notebook ............................................................................. 3 Safety .............................................................................. 3 Laboratory Practices and Safety Rules ............................................................. 4 Accidents and injuries ........................................................................... 5 Fires ............................................................................. 5 Chemical Wastes ............................................................................. 6 Cleaning Responsibilities ............................................................................. 6 Lab cleanliness ............................................................................. 6 Laboratory Equipment ............................................................................. 7 Proper use of glassware ............................................................................. 8 Some techniques in lab experiments Heating, cooling and stirring ............................................................................ -

The Replacement of a Phenol Group by an Aniline Or Acetanilide Group
The replacement of a phenol group by an aniline or acetanilide group enhances the cytotoxicity of 2-ferrocenyl-1,1-diphenyl-but-1-ene compounds against breast cancer cells Pascal Pigeon, Siden Top, Ouardia Zekri, Elisabeth A. Hillard, Anne Vessieres, M.A. Plamont, Olivier Buriez, Eric Labbé, Michel Huché, Sultana Boutamine, et al. To cite this version: Pascal Pigeon, Siden Top, Ouardia Zekri, Elisabeth A. Hillard, Anne Vessieres, et al.. The replacement of a phenol group by an aniline or acetanilide group enhances the cytotoxicity of 2-ferrocenyl-1,1- diphenyl-but-1-ene compounds against breast cancer cells. Journal of Organometallic Chemistry, Elsevier, 2009, 694, pp.895-901. 10.1016/j.jorganchem.2008.11.035. hal-00376093 HAL Id: hal-00376093 https://hal.archives-ouvertes.fr/hal-00376093 Submitted on 14 Oct 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. The replacement of a phenol group by an aniline or acetanilide group enhances the cytotoxicity of 2-ferrocenyl-1,1-diphenyl-but-l-ene compounds against breast cancer cells Pascal Pigeon a, -
Aspirin a Curriculum Resource for Post-16 Chemistry and Science Courses
Aspirin A curriculum resource for post-16 chemistry and science courses 1 Aspirin (2nd edition) Compiled by David Lewis Edited by Colin Osborne and Maria Pack Designed by Imogen Bertin and Sara Roberts First published by the Royal Society of Chemistry in 1998 Second edition published by the Royal Society of Chemistry in 2003 Printed by the Royal Society of Chemistry Copyright © Royal Society of Chemistry 2003 Registered charity No. 207890 Apart from any fair dealing for the purposes of research or private study, or criticism or review, as permitted under the UK Copyright Designs and Patents Act, 1988, this publication may not be reproduced, stored, or transmitted, in any form or by any means, without the prior permission in writing of the publishers, or in the case of reprographic reproduction, only in accordance with the terms of the licences issued by the Copyright Licensing Agency in the UK, or in accordance with the terms of licences issued by the appropriate Reproduction Rights Organisation outside the UK. Enquiries concerning reproduction outside the terms stated here should be sent to the Royal Society of Chemistry at the London address printed on this page. Notice to all UK Educational Institutions. The material in this book may be reproduced by photocopying for distribution and use by students within the purchasing institution providing no more than 50% of the work is reproduced in this way for any one purpose. Tutors wishing to reproduce material beyond this limit or to reproduce the work by other means such as electronic should first seek the permission of the Society. -

Bulk Drug Substances Under Evaluation for Section 503A
Updated July 1, 2020 Bulk Drug Substances Nominated for Use in Compounding Under Section 503A of the Federal Food, Drug, and Cosmetic Act Includes three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Concerns • Category 3: Bulk Drug Substances Nominated Without Adequate Support Updates to Section 503A Categories • Removal from category 3 o Artesunate – This bulk drug substance is a component of an FDA-approved drug product (NDA 213036) and compounded drug products containing this substance may be eligible for the exemptions under section 503A of the FD&C Act pursuant to section 503A(b)(1)(A)(i)(II). This change will be effective immediately and will not have a waiting period. For more information, please see the Interim Policy on Compounding Using Bulk Drug Substances Under Section 503A and the final rule on bulk drug substances that can be used for compounding under section 503A, which became effective on March 21, 2019. 1 Updated July 1, 2020 503A Category 1 – Bulk Drug Substances Under Evaluation • 7 Keto Dehydroepiandrosterone • Glycyrrhizin • Acetyl L Carnitine/Acetyl-L- carnitine • Kojic Acid Hydrochloride • L-Citrulline • Alanyl-L-Glutamine • Melatonin • Aloe Vera/ Aloe Vera 200:1 Freeze Dried • Methylcobalamin • Alpha Lipoic Acid • Methylsulfonylmethane (MSM) • Artemisia/Artemisinin • Nettle leaf (Urtica dioica subsp. dioica leaf) • Astragalus Extract 10:1 • Nicotinamide Adenine Dinucleotide (NAD) • Boswellia • Nicotinamide -

Quantitative Assessment of Population Variability in Hepatic Drug Metabolism Using a Perfused Three-Dimensional Human Liver Microphysiological System S
Quantitative Assessment of Population Variability in Hepatic Drug Metabolism Using a Perfused Three- Dimensional Human Liver Microphysiological System The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Tsamandouras, N., T. Kostrzewski, C. L. Stokes, L. G. Griffith, D. J. Hughes, and M. Cirit. “Quantitative Assessment of Population Variability in Hepatic Drug Metabolism Using a Perfused Three- Dimensional Human Liver Microphysiological System.” Journal of Pharmacology and Experimental Therapeutics 360, no. 1 (October 19, 2016): 95–105. As Published http://dx.doi.org/10.1124/JPET.116.237495 Publisher American Society for Pharmacology & Experimental Therapeutics (ASPET) Version Final published version Citable link http://hdl.handle.net/1721.1/117617 Terms of Use Creative Commons Attribution-NonCommercial 4.0 International Detailed Terms http://creativecommons.org/licenses/by-nc/4.0/ Downloaded from jpet.aspetjournals.org at ASPET Journals on August 30, 2018 95 105, January 2017 – and the associ- ” http://dx.doi.org/10.1124/jpet.116.237495 c clearance, as assessed in vitro, g metabolism in the context of a J Pharmacol Exp Ther 360:95 average individual, “ Several in vitro systems have been traditionally applied to ated interindividual variability is not obtained. variability in intrinsic metaboli needstobecoupledwiththepopulationvariabilityassociated with other physiologic processes indrug vivo binding (e.g., to hepatic plasma bloodpredictions proteins, flow, etc.). at Thus, to theapproach perform population (Trame in vivo et level,results al., a are 2016) integrated systems is into pharmacology desirable,pharmacokinetic population physiologically (PBPK) where based models the (Rostami-Hodjegan, inJones and 2012; vitro Rowland-Yeo, 2013; Tsamandouras et al., 2015a,b).