New Zealand Data Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmaceutical Powder Compressibility – a Science-Based Approach
Pharmaceutical powder compressibility – a science-based approach Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Nicolaos D.Gentis aus Egrigoros (Chios) Griechenland Oberkulm (AG) Schweiz Basel, 2012 Approval Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Matthias Hamburger und PD Dr. Gabriele Betz und Prof. Dr. Thierry F. Vandamme Basel, den 21. Februar 2012 Prof. Dr. Martin Spiess Dekan 2 Dedicated to my parents with love, appreciation and respect 3 Σωκράτης ―I know one thing, that I know nothing‖ Socrates c. 469 BC – 399 BC 4 Acknowledgements The work for this PhD thesis was carried out in the Industrial Pharmacy Lab, Department of Pharmaceutical Sciences, University of Basel and at the facility of Natoli Engineering Inc. in Saint Louis, Missouri (USA). I would like to express my appreciation and sincere gratefulness to PD Dr. Gabriele Betz for giving me the opportunity to do a PhD under her excellent supervision with essential, continuous support, guidance and brilliant, positive motivation. I would like to thank Prof. Dr. Matthias Hamburger for accepting to be my Faculty Responsible and for the support. My appreciation goes also to Prof. Dr. Thierry F. Vandamme for accepting to assume the co-referencing of this PhD thesis. At this point I would like to thank all former Industrial Pharmacy Research Group members for the unique support and for the great, crazy working atmosphere in the laboratory. Especially I would like to thank Mr. Branko Z. Vranic for his great collaboration and support in the research work of project 2 in this thesis. -

A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia
Korean J Pain 2015 July; Vol. 28, No. 3: 203-209 pISSN 2005-9159 eISSN 2093-0569 http://dx.doi.org/10.3344/kjp.2015.28.3.203 | Original Article | A Comparative Efficacy of Propacetamol and Ketorolac in Postoperative Patient Controlled Analgesia Department of Anesthesiology and Pain Medicine, Chonnam National University Medical School, Gwangju, Korea Bong Ha Heo, Ji Hun Park, Jung Il Choi, Woong Mo Kim, Hyoung Gon Lee, Soo Young Cho, and Myoung Ha Yoon Background: Ketorolac has been used as a postoperative analgesia in combination with opioids. However, the use of ketorolac may produce serious side effects in vulnerable patients. Propacetamol is known to induce fewer side effects than ketorolac because it mainly affects the central nervous system. We compared the analgesic effects and patient satisfaction levels of each drug when combined with fentanyl patient-controlled analgesia (PCA). Methods: The patients were divided into two groups, each with n = 46. The patients in each group were given 60 mg of ketorolac or 2 g of propacetamol (mixed with fentanyl) for 10 minutes. The patients were then given 180 mg of ketorolac or 8 g of propacetamol (mixed with fentanyl and ramosetron) through PCA. We assessed the visual analogue pain scale (VAS) at the time point immediately before administration (baseline) and at 15, 30, and 60 minutes, and 24 hours after administration. Also, the side effects of each regimen and each patient’s degree of satisfaction were assessed. Results: There was a significant decline in the VAS score in both groups (P < 0.05). However, there were no significant differences in the VAS scores between the groups at each time point. -
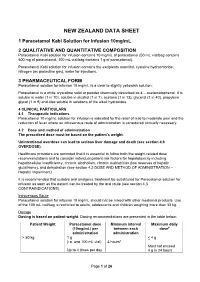
Paracetamol Kabi Data Sheet
NEW ZEALAND DATA SHEET 1 Paracetamol Kabi Solution for Infusion 10mg/mL 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Paracetamol Kabi solution for infusion contains 10 mg/mL of paracetamol (50 mL vial/bag contains 500 mg of paracetamol, 100 mL vial/bag contains 1 g of paracetamol). Paracetamol Kabi solution for infusion contains the excipients mannitol, cysteine hydrochloride, nitrogen (as protective gas), water for injections. 3 PHARMACEUTICAL FORM Paracetamol solution for infusion 10 mg/mL is a clear to slightly yellowish solution. Paracetamol is a white crystalline solid or powder chemically described as 4 – acetamidophenol. It is soluble in water (1 in 70), soluble in alcohol (1 in 7), acetone (1 in 13), glycerol (1 in 40), propylene glycol (1 in 9) and also soluble in solutions of the alkali hydroxides. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Paracetamol 10 mg/mL solution for infusion is indicated for the relief of mild to moderate pain and the reduction of fever where an intravenous route of administration is considered clinically necessary. 4.2 Dose and method of administration The prescribed dose must be based on the patient’s weight. Unintentional overdose can lead to serious liver damage and death (see section 4.9 OVERDOSE). Healthcare providers are reminded that it is essential to follow both the weight-related dose recommendations and to consider individual patient risk factors for hepatotoxicity including hepatocellular insufficiency, chronic alcoholism, chronic malnutrition (low reserves of hepatic glutathione), and dehydration (see section 4.2 DOSE AND METHOD OF ADMINISTRATION – Hepatic Impairment). It is recommended that suitable oral analgesic treatment be substituted for Paracetamol solution for infusion as soon as the patient can be treated by the oral route (see section 4.3 CONTRAINDICATIONS). -

(8) No. 1 March 2005 Alexandria Journal of Anaesthesia and Intensive Care 50
Alexandria Journal of Anaesthesia and Intensive Care 49 Propacetamol Versus Placebo for Management of Acute Postoperative Pain After Elective Tonsillectomy in Children. Mahmoud A Nassef, MD*. Ashraf M Moustafa, MD**. Ashraf A Moussa, MD***. *Department of Anesthesia, Beni-Suef Faculty of Medicine, Cairo University **Department of Anesthesia, Menoufiya University ***Department of Anesthesia,Menoufiya Liver Institute, Menoufiya University ABSTRACT The analgesic efficacy and safety of propacetamol, an injectable prodrug of acetaminophen, was assessed versus placebo after elective tonsillectomy operation in children. Using a double-blind, randomized parallel group design, 70 children aged 6-12 years were included to evaluate the effect of a single iv infusion of 40 mg/kg propacetamol versus a single infusion of 100 ml normal saline ( placebo ) given at the recovery room. Analgesic efficacy was assessed on pain scores rated on a four-points verbal scale, a five-points visual scale ( faces ) and a four-points pain relief verbal scale; before administration ( T0 ) and 0.25, 0.5, 1, 2, 3, 4, 5 and 6 hours after the infusion. The global efficacy was rated on a five-point scale at the end of the study. Rescue medication was allowed freely and the time for re-medication as well as the occurrence of any side effects was recorded. Propacetamol was statistically superior to placebo on all assessment criteria. The global final efficacy evaluation demonstrated 12 patients in the propacetamol group with good and very good scores compared to only one patient in the placebo group. Rescue medication was used in 40% of patients in the propacetamol group versus 83% in the placebo group. -

Treatment for Acute Pain: an Evidence Map Technical Brief Number 33
Technical Brief Number 33 R Treatment for Acute Pain: An Evidence Map Technical Brief Number 33 Treatment for Acute Pain: An Evidence Map Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. 290-2015-0000-81 Prepared by: Minnesota Evidence-based Practice Center Minneapolis, MN Investigators: Michelle Brasure, Ph.D., M.S.P.H., M.L.I.S. Victoria A. Nelson, M.Sc. Shellina Scheiner, PharmD, B.C.G.P. Mary L. Forte, Ph.D., D.C. Mary Butler, Ph.D., M.B.A. Sanket Nagarkar, D.D.S., M.P.H. Jayati Saha, Ph.D. Timothy J. Wilt, M.D., M.P.H. AHRQ Publication No. 19(20)-EHC022-EF October 2019 Key Messages Purpose of review The purpose of this evidence map is to provide a high-level overview of the current guidelines and systematic reviews on pharmacologic and nonpharmacologic treatments for acute pain. We map the evidence for several acute pain conditions including postoperative pain, dental pain, neck pain, back pain, renal colic, acute migraine, and sickle cell crisis. Improved understanding of the interventions studied for each of these acute pain conditions will provide insight on which topics are ready for comprehensive comparative effectiveness review. Key messages • Few systematic reviews provide a comprehensive rigorous assessment of all potential interventions, including nondrug interventions, to treat pain attributable to each acute pain condition. Acute pain conditions that may need a comprehensive systematic review or overview of systematic reviews include postoperative postdischarge pain, acute back pain, acute neck pain, renal colic, and acute migraine. -

022450Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 022450Orig1s000 PHARMACOLOGY REVIEW(S) 5 Page(s) of Draft Labeling have been Withheld in Full as b4 (CCI/TS) immediately following this page (b) (4) (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL (b) (4) (b) (4) COPYRIGHT MATERIAL (b) (4) (b) (4) COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) (b) (4) COPYRIGHT MATERIAL COPYRIGHT MATERIAL (b) (4) (b) (4) (b) (4) (b) (4) Pharmacology Toxicology Review Addendum Executive Summary I. Recommendations A. Recommendation on approvability From the nonclinical pharmacology perspective, NDA 22-450 is recommended for approval. B. Recommendation for nonclinical studies At this time, there are no nonclinical studies needed that will impact approvability. C. Recommendation on labeling The table below contains the draft labeling submitted by the sponsor, the proposed changes and the rationale for the proposed changes for the nonclinical toxicology section only. Please see the secondary review for final labeling recommendations. (b) (4) 1 Reviewer: Carlic K. Huynh, Ph.D. NDA No. 22-450 (b) (4) II. Summary of nonclinical findings A. Brief overview of nonclinical findings From the previous pharmacology toxicology review of this NDA, acetaminophen is not a mutagen (as demonstrated by negative results in the bacterial Ames test) but is a clastogen (as demonstrated by positive results in the chromosomal aberration assay in cultured human peripheral blood lymphocytes). -

Old Drug, New Route: a Systematic Review of Intravenous Acetaminophen After Adult Cardiac Surgery
REVIEW ARTICLE Paul G. Barash, MD Giovanni Landoni, MD Section Editors Old Drug, New Route: A Systematic Review of Intravenous Acetaminophen After Adult Cardiac Surgery Daniel J. Douzjian, MD, and Alexander Kulik, MD, MPH HE MANAGEMENT OF postoperative pain after cardiac first discovered in 1877, but it was not until 1950 that it was Tsurgery remains clinically challenging. Well-controlled marketed for clinical use as a pain reliever.18 While it is less pain is critical to maintaining the physical and psychologic potent in its analgesic properties, unlike opiates, acetaminophen well-being of each patient and can help facilitate timely has no respiratory depressant action and does not cause nausea extubation, comfortable breathing, and early postoperative ambu- or vomiting.18,19 It has a minimal hemodynamic effect, and the lation. On the other hand, left poorly managed, postoperative pain only contraindications to its use are severe hepatic impairment, can lead to rising catecholamine levels, ultimately triggering allergy, or hypersensitivity. Given its safety profile, it has myocardial ischemia, stroke, or bleeding complications.1-3 Insuf- become a common household drug and has been available in ficient pain control also can limit patient mobility, increasing the oral form without prescription since 1959.18 To date, the risk of deep vein thrombosis and pneumonia, in addition to the mechanism of action of acetaminophen is not understood harmful psychologic consequences of insomnia and demoraliza- completely, although it is believed to involve -

ASDERA – Overview
ASDERA – Overview Develop novel drugs for high unmet needs Mission by utilizing a computational biostatistics platform (US 7,664,616), the first to identify genetic risk factors for complex diseases 1800 Gauss-Legendre 1948 Hoeffding Drug 1900 1965 1985 2001 Discovery Ohdner IBM PC GPU Platform 9 Byte 256 kB 16 MB 4 GB ANOVA PCA Bayes u-Stat Validation: Confirmation of known drug targets in epilepsy Proof-of-Concept: L-fucose in Crohn’s disease (in phase 3) Time-Pipeline Current lead: lead: ASD-002 Mefenamic against acid against mutism mutism in autism in autism (phase(phase 3 ready) 3 ready) Next drug: Preventing metastases in breast cancer (pat. pending) Outlook: Delaying Alzheimer ’s and Parkinson ’s (pat. pending) © ASDERA (2017) Confidential Information 1 ASDERA – Overview Develop the first drug to prevent lack-of-language in autism ( unmet need ) Focus by utilizing a computational biostatistics platform (US 7,664,616), the first platform to identify genetic risk factors for complex diseases Disruption of Active Language Development (DALD) Lead Indication: in toddlers developing Autism Spectrum Disorders (ASD) by childhood migraines causing them to Mutism • become non-verbal (primary outcome) and in Autism • develop life-long intellectual disability (ID) Children will still develop autism, but will be verbal (“Asperger’s”). Product ASD-002: Market-exclusive ester-prodrug of mefenamic acid (MFA) Patent filed in US and EU. Orphan Drug Designation for MFA pending Status Preparing CMC / manufacturing for a short 505(b)(2) regulatory -

WO 2013/020527 Al 14 February 2013 (14.02.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2013/020527 Al 14 February 2013 (14.02.2013) P O P C T (51) International Patent Classification: (74) Common Representative: UNIVERSITY OF VETER¬ A61K 9/06 (2006.01) A61K 47/32 (2006.01) INARY AND PHARMACEUTICAL SCIENCES A61K 9/14 (2006.01) A61K 47/38 (2006.01) BRNO FACULTY OF PHARMACY; University of A61K 47/10 (2006.01) A61K 9/00 (2006.01) Veterinary and Pharmaceutical Sciences Brno Faculty Of A61K 47/18 (2006.01) Pharmacy, Palackeho 1/3, CZ-61242 Brno (CZ). (21) International Application Number: (81) Designated States (unless otherwise indicated, for every PCT/CZ20 12/000073 kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (22) Date: International Filing BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, 2 August 2012 (02.08.2012) DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (25) Filing Language: English HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (26) Publication Language: English ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (30) Priority Data: NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, 201 1-495 11 August 201 1 ( 11.08.201 1) SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, 2012- 72 1 February 2012 (01.02.2012) TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, 2012-5 11 26 July 2012 (26.07.2012) ZW. -

Propacetamol-Induced Injection Pain Is Associated with Activation of Transient Receptor Potential Vanilloid 1 Channels S
Supplemental material to this article can be found at: http://jpet.aspetjournals.org/content/suppl/2016/07/25/jpet.116.233452.DC1 1521-0103/359/1/18–25$25.00 http://dx.doi.org/10.1124/jpet.116.233452 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 359:18–25, October 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Propacetamol-Induced Injection Pain Is Associated with Activation of Transient Receptor Potential Vanilloid 1 Channels s Florian Schillers, Esther Eberhardt, Andreas Leffler, and Mirjam Eberhardt Department of Anaesthesiology and Intensive Care Medicine, Hannover Medical School, Hannover, Germany (F.S., A.L., M.E.); and Department of Anaesthesiology, Friedrich-Alexander University Erlangen-Nuremberg, Erlangen, Germany (E.E.) Received March 8, 2016; accepted July 22, 2016 ABSTRACT Downloaded from Propacetamol (PPCM) is a prodrug of paracetamol (PCM), were expressed in human embryonic kidney 293 cells and which was generated to increase water solubility of PCM for investigated by means of whole-cell patch clamp and ratio- intravenous delivery. PPCM is rapidly hydrolyzed by plasma metric calcium imaging. PPCM (but not PCM) activated esterases to PCM and diethylglycine and shares some struc- TRPV1, sensitized heat-induced currents, and caused an tural and metabolic properties with lidocaine. Although PPCM increase in intracellular calcium. In TRPA1-expressing cells is considered to be comparable to PCM regarding its analgesic however, both PPCM and PCM evoked calcium responses but properties, injection pain is a common side effect described for failed to induce inward currents. Intracutaneous injection of jpet.aspetjournals.org PPCM but not PCM. -

The Antipyretic Efficacy and Safety of Propacetamol Compared With
Choi et al. BMC Pediatrics (2018) 18:201 https://doi.org/10.1186/s12887-018-1166-z RESEARCHARTICLE Open Access The antipyretic efficacy and safety of propacetamol compared with dexibuprofen in febrile children: a multicenter, randomized, double-blind, comparative, phase 3 clinical trial Seung Jun Choi1,2, Sena Moon3, Ui Yoon Choi3, Yoon Hong Chun3, Jung Hyun Lee3, Jung Woo Rhim3, Jin Lee4, Hwang Min Kim5 and Dae Chul Jeong3,6* Abstract Background: We aimed to compare the antipyretic efficacy, safety, and tolerability between oral dexibuprofen and intravenous propacetamol in children with upper respiratory tract infection (URTI) presenting with fever. Methods: Patients aging from 6 months to 14 years admitted for URTI with axillary body temperature ≥ 38.0 °C were enrolled and randomized into the study or control group. Patients in the study group were intravenously infused with propacetamol and subsequently oral placebo medication was administered. Patients in the control group were intravenously infused with 100 mL of 0.9% sodium chloride solution without propacetamol and then oral dexibuprofen was administered. We checked the body temperature of all patients at 0.5 h (hr), 1 h, 1.5 h, 2 h, 3 h, 4 h, and 6 h after oral placebo or dexibuprofen had been applied. Results: A total of 263 patients (125 in the study group) were finally enrolled. The body temperatures of patients in the study group were significantly lower until 2 h after administration (37.73 ± 0.58 vs 38.36 ± 0.69 °C (p < 0.001), 37. 37 ± 0.53 vs 37.88 ± 0.69 °C (p < 0.001), 37.27 ± 0.60 vs 37.62 ± 0.66 °C (p < 0.001), 37.25 ± 0.62 vs 37.40 ± 0.60 °C (p = 0.0452), at 0.5 h, 1 h, 1.5 h, and 2 h, respectively). -

Australian Product Information- Paracetamol Kabi (Paracetamol)
AUSTRALIAN PRODUCT INFORMATION- PARACETAMOL KABI (PARACETAMOL) 1. NAME OF MEDICINE Paracetamol 2. QUALITATIVE AND QUANTATIVE COMPOSITION Paracetamol Kabi solution for infusion contains 10 mg/mL of paracetamol (50 mL vial/ bag contains 500 mg of paracetamol, 100 mL vial/bag contains 1 g of paracetamol). Paracetamol Kabi solution for infusion contains the excipients mannitol, cysteine hydrochloride, nitrogen (as protective gas), water for injections. For the full list of excipients, see Section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Paracetamol solution for infusion 10 mg/mL is a clear to slightly yellowish solution. Paracetamol is a white crystalline solid or powder chemically described as 4 – acetamidophenol. It is soluble in water (1 in 70), soluble in alcohol (1 in 7), acetone (1 in 13), glycerol (1 in 40), propylene glycol (1 in 9) and also soluble in solutions of the alkali hydroxides. 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications Paracetamol 10 mg/mL solution for infusion is indicated for the relief of mild to moderate pain and the reduction of fever where an intravenous route of administration is considered clinically necessary. 4.2 Dose and Method of Administration The prescribed dose must be based on the patient’s weight. Unintentional overdose can lead to serious liver damage and death (see section 4.9 Overdose). Healthcare providers are reminded that it is essential to follow both the weight-related dose recommendations and to consider individual patient risk factors for hepatotoxicity including hepatocellular insufficiency, chronic alcoholism, chronic malnutrition (low reserves of hepatic glutathione), and dehydration (see section 4.2 Dose method and Administration – Hepatic Impairment).