Supplementary Appendix
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao Et Al
USOO9498481 B2 (12) United States Patent (10) Patent No.: US 9,498,481 B2 Rao et al. (45) Date of Patent: *Nov. 22, 2016 (54) CYCLOPROPYL MODULATORS OF P2Y12 WO WO95/26325 10, 1995 RECEPTOR WO WO99/O5142 2, 1999 WO WOOO/34283 6, 2000 WO WO O1/92262 12/2001 (71) Applicant: Apharaceuticals. Inc., La WO WO O1/922.63 12/2001 olla, CA (US) WO WO 2011/O17108 2, 2011 (72) Inventors: Tadimeti Rao, San Diego, CA (US); Chengzhi Zhang, San Diego, CA (US) OTHER PUBLICATIONS Drugs of the Future 32(10), 845-853 (2007).* (73) Assignee: Auspex Pharmaceuticals, Inc., LaJolla, Tantry et al. in Expert Opin. Invest. Drugs (2007) 16(2):225-229.* CA (US) Wallentin et al. in the New England Journal of Medicine, 361 (11), 1045-1057 (2009).* (*) Notice: Subject to any disclaimer, the term of this Husted et al. in The European Heart Journal 27, 1038-1047 (2006).* patent is extended or adjusted under 35 Auspex in www.businesswire.com/news/home/20081023005201/ U.S.C. 154(b) by Od en/Auspex-Pharmaceuticals-Announces-Positive-Results-Clinical M YW- (b) by ayS. Study (published: Oct. 23, 2008).* This patent is Subject to a terminal dis- Concert In www.concertpharma. com/news/ claimer ConcertPresentsPreclinicalResultsNAMS.htm (published: Sep. 25. 2008).* Concert2 in Expert Rev. Anti Infect. Ther. 6(6), 782 (2008).* (21) Appl. No.: 14/977,056 Springthorpe et al. in Bioorganic & Medicinal Chemistry Letters 17. 6013-6018 (2007).* (22) Filed: Dec. 21, 2015 Leis et al. in Current Organic Chemistry 2, 131-144 (1998).* Angiolillo et al., Pharmacology of emerging novel platelet inhibi (65) Prior Publication Data tors, American Heart Journal, 2008, 156(2) Supp. -

Nimesulide: Patients Still Exposed to a Risk of Severe Hepatitis
Translated from Rev Prescrire January 2011; 31 (327): 22-23 Nimesulide: patients still exposed to a risk of severe hepatitis Abstract imesulide, a nonsteroidal anti- Severe liver damage at standard N inflammatory drug (NSAID), has doses, especially in young women. In Nimesulide, a nonsteroidal anti- been on the French market since 2007, the Italian Medicines Agency inflammatory drug (NSAID) that has 1998 (1). It is neither more effective nor released Italian pharmacovigilance data been marketed in France since 1998, is better tolerated than many other showing that hepatic adverse effects rep- neither more effective nor better tol- NSAIDs, and has been shown to cause resented 13.8% of reports implicating erated than other NSAIDs. potentially life-threatening liver da- nimesulide, compared to only 1.4% for mage (1-5). ibuprofen and 2.8% for diclofenac (3). Many reports and reviews published What is known concerning the hepatic The CHMP report published in 2008 by drug regulatory agencies in Spain, adverse effects of nimesulide in early included similar findings. Among the Ireland and Italy have warned of the 2011? 574 reports implicating nimesulide record- hepatic adverse effects of nimesulide. ed in the European EudraVigilance phar- In early 2008, 17 cases of nimesulide- An increasing number of reports of macovigilance database, the proportion of induced liver damage requiring trans- liver damage. Soon after it was first mar- hepatic disorders (cholestasis, jaundice, plantation had been reported in Ire- keted, cases of hepatitis were attributed liver failure, and hepatitis) was higher land, Italy, Spain, Finland and France. to nimesulide, including a case of fulmi- than with cox-2 inhibitors. -

Specifications of Approved Drug Compound Library
Annexure-I : Specifications of Approved drug compound library The compounds should be structurally diverse, medicinally active, and cell permeable Compounds should have rich documentation with structure, Target, Activity and IC50 should be known Compounds which are supplied should have been validated by NMR and HPLC to ensure high purity Each compound should be supplied as 10mM solution in DMSO and at least 100µl of each compound should be supplied. Compounds should be supplied in screw capped vial arranged as 96 well plate format. -

Pharmaceutical Powder Compressibility – a Science-Based Approach
Pharmaceutical powder compressibility – a science-based approach Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Nicolaos D.Gentis aus Egrigoros (Chios) Griechenland Oberkulm (AG) Schweiz Basel, 2012 Approval Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Matthias Hamburger und PD Dr. Gabriele Betz und Prof. Dr. Thierry F. Vandamme Basel, den 21. Februar 2012 Prof. Dr. Martin Spiess Dekan 2 Dedicated to my parents with love, appreciation and respect 3 Σωκράτης ―I know one thing, that I know nothing‖ Socrates c. 469 BC – 399 BC 4 Acknowledgements The work for this PhD thesis was carried out in the Industrial Pharmacy Lab, Department of Pharmaceutical Sciences, University of Basel and at the facility of Natoli Engineering Inc. in Saint Louis, Missouri (USA). I would like to express my appreciation and sincere gratefulness to PD Dr. Gabriele Betz for giving me the opportunity to do a PhD under her excellent supervision with essential, continuous support, guidance and brilliant, positive motivation. I would like to thank Prof. Dr. Matthias Hamburger for accepting to be my Faculty Responsible and for the support. My appreciation goes also to Prof. Dr. Thierry F. Vandamme for accepting to assume the co-referencing of this PhD thesis. At this point I would like to thank all former Industrial Pharmacy Research Group members for the unique support and for the great, crazy working atmosphere in the laboratory. Especially I would like to thank Mr. Branko Z. Vranic for his great collaboration and support in the research work of project 2 in this thesis. -

Emerging Drug List PARECOXIB SODIUM
Emerging Drug List PARECOXIB SODIUM NO. 10 MAY 2001 Generic (Trade Name): Parecoxib sodium Manufacturer: Pharmacia & Upjohn Inc. Indication: For peri-operative pain relief Current Regulatory Parecoxib is currently under review at Health Canada and the Food and Drug Status: Administration in the U.S. They are expecting approval in the fourth quarter of 2001. It is not marketed in any country at this time Description: Parecoxib is the first parenteral cyclooxygenase-2 (COX-2) selective inhibitor to be developed. It is a water-soluble prodrug that is rapidly hydrolyzed to valdecoxib (the active COX-2 inhibitor). Valdecoxib's affinity for COX-2 versus COX-1 is 90 times greater than celecoxib and 34,000 times greater than ketorolac. Once injected, peak concentrations of valdecoxib are attained in 10 to 20 minutes. Valdecoxib has a half-life of eight to 10 hours. Current Treatment: Currently, the only other nonsteroidal anti-inflammatory agent that is available as an injection is ketorolac. Ketorolac is used in some centres for peri-operative pain management, however opioids are the main class of agents used for this indication. Ketorolac has been associated with a relatively high incidence of gastrointestinal (GI) side effects, including severe cases of hemorrhage. Cost: There is no information available on the cost of parecoxib. Evidence: Parecoxib has been compared to ketorolac and morphine in clinical trials. Parecoxib at a dose of 20 and 40 mg/day IV, were compared to ketorolac, 30 mg/day IV and morphine, 4 mg/day or placebo in 202 women undergoing hysterectomy. Both doses of parecoxib were comparable to ketorolac for relieving postoperative pain. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Use of Aspirin and Nsaids to Prevent Colorectal Cancer
Evidence Synthesis Number 45 Use of Aspirin and NSAIDs to Prevent Colorectal Cancer Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-02-0021 Prepared by: University of Ottawa Evidence-based Practice Center at The University of Ottawa, Ottawa Canada David Moher, PhD Director Investigators Alaa Rostom, MD, MSc, FRCPC Catherine Dube, MD, MSc, FRCPC Gabriela Lewin, MD Alexander Tsertsvadze, MD Msc Nicholas Barrowman, PhD Catherine Code, MD, FRCPC Margaret Sampson, MILS David Moher, PhD AHRQ Publication No. 07-0596-EF-1 March 2007 This report is based on research conducted by the University of Ottawa Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-02-0021). Funding was provided by the Centers for Disease Control and Prevention. The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This document is in the public domain and may be used and reprinted without permission except those copyrighted materials noted for which further reproduction is prohibited without the specific permission of copyright holders. -
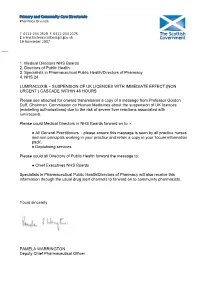
Lumiracoxib: Suspension of UK Licences with Immediate Effect (Non
Primary and Community Care Directorate Pharmacy Division T: 0131-244 2528 F: 0131-244 2375 E: [email protected] abcdefghijklmnopqrstu 19 November 2007 ___ 1. Medical Directors NHS Boards 2. Directors of Public Health 3. Specialists in Pharmaceutical Public Health/Directors of Pharmacy 4. NHS 24 LUMIRACOXIB – SUSPENSION OF UK LICENCES WITH IMMEDIATE EFFECT (NON URGENT ) CASCADE WITHIN 48 HOURS Please see attached for onward transmission a copy of a message from Professor Gordon Duff, Chairman, Commission on Human Medicines about the suspension of UK licences (marketing authorisations) due to the risk of severe liver reactions associated with lumiracoxib. Please could Medical Directors in NHS Boards forward on to :- ● All General Practitioners - please ensure this message is seen by all practice nurses and non principals working in your practice and retain a copy in your ‘locum information pack’. ● Deptutising services Please could all Directors of Public Health forward the message to: ● Chief Executives NHS Boards Specialists in Pharmaceutical Public Health/Directors of Pharmacy will also receive this information through the usual drug alert channels to forward on to community pharmacists. Yours sincerely PAMELA WARRINGTON Deputy Chief Pharmaceutical Officer St Andrew’s House, Regent Road, Edinburgh EH1 3DG www.scotland.gov.uk abcde abc a Ref: EL(07)A/21 LUMIRACOXIB - SUSPENSION OF UK LICENCES WITH IMMEDIATE EFFECT 19 November 2007 Dear Colleague, I am writing to inform you that the UK licences (marketing authorisations) for lumiracoxib have been suspended and stocks are being withdrawn from pharmacies, on the basis of advice from the Commission on Human Medicines (CHM). -

White Paper on Nimesulide Pharmacologic Category
White paper on Nimesulide Pharmacologic Category : Analgesic, Nonsteroidal Anti-inflammatory Drug; Nonsteroidal Anti-inflammatory Drug (NSAID) Indications: Fever, Pain & Inflammation Duration: Can be safely prescribed upto 15 days. Adults: Oral: 100 mg twice daily. Children below 12 years: Not to be used. Product Availability: Product available in various countries; not currently available in the U.S. Dosage Forms: Tablet: 100 mg 1. Nimesulide has preferential selectivity for COX-2 over COX-1 in vivo at full therapeutic doses and induces less gastrointestinal damage than that seen with naproxen in the short term. [ Uptodate: Gut. 2001;48(3):339.] 2. Atopy is a risk factor for non-steroidal anti-inflammatory drug sensitivity. The prevalence of atopy is increased in challenge-proven NSAID-intolerant patients. The atopic condition may represent an important risk factor for developing reactions to these drugs. Paracetamol and nimesulide are relatively safe alternative choices in those patients. [ Uptodate: Ann Allergy Asthma Immunol. 2000;84(1):101.] 3. Topical NSAIDs that are effective for chronic musculoskeletal pain in adults include diclofenac, ketoprofen (level 1 [likely reliable] evidence), ibuprofen, felbinac, and nimesulide (level 2 [mid-level] evidence) [DynaMed] 4. nimesulide may be associated with better efficacy than diclofenac for acute gout (level 2 [mid-level] evidence) [Ter Arkh 2007;79(5):35 ] 5. Nimesulide is safe in Crohn's disease [DynaMed: Clin Gastroenterol Hepatol 2006 Feb;4(2):196] 6. It is safe in ulcerative colitis { DynaMed Clin Gastroenterol Hepatol 2006 Feb;4(2):196, commentary can be found in Clin Gastroenterol Hepatol 2006 Feb;4(2):157] 7. Many PUBMED studies are available about its efficacy in primary dysmennhorea, acute dental pain, respiratory inflammatory conditions etc. -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

Short Reports
Br Med J (Clin Res Ed): first published as 10.1136/bmj.287.6395.798 on 17 September 1983. Downloaded from 798 BRITISH MEDICAL JOURNAL VOLUME 287 17 SEPTEMBER 1983 SHORT REPORTS analgesic properties. The usual daily dosage is 400 mg. The amount Piroxicam poisoning of fentiazac absorbed after gastric lavage would probably be small and of little importance. Piroxicam is a potent non-steroidal anti-inflammatory drug. Ex- The main signs were altered consciousness and muscle twitchings. perience with overdosage is limited. We describe a patient who took The exact causes of these were unknown, but griseofulvin has been a large dose of piroxicam. associated with dizziness, mental confusion, irritability, and impaired coordination.2 Side effects of piroxicam have occasionally included headache and dizziness, although their incidences in double blind Case report comparative studies have been lower than those reported with indomethacin.3 Thus the drowsiness and muscle twitchings could not A 25 year old Chinese man weighing 46 kg was admitted to hospital be definitely attributed to piroxicam. about two hours after ingesting 56 capsules of 10 mg piroxicam, 97 tablets Gastrointestinal bleeding is usually the major side effect of most of 125 mg griseofulvin, and about 10 tablets of 100 mg fentiazac. He had been drugs. Piroxicam seemed to be well suffering from psoriatic arthropathy affecting both knee and ankle joints non-steroidal anti-inflammatory and had been taking piroxicam 30 mg daily for nine months. Other anal- tolerated since the patient did not complain of gastric discomfort or gesics, including aspirin, paracetamol, fentiazac, and indomethacin, had gastrointestinal bleeding despite a history of gastric erosions. -

The Effectiveness of Patches Containing Loxoprofen Sodium
22 Japanese Journal of Comprehensive Rehabilitation Science (2013) Original Article The effectiveness of patches containing Loxoprofen Sodium Hydrate (LX-P) in the conservative therapy of muscular back pain – Clinical results using the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) Toyoko Asami, MD, PhD,1 Naoya Yamanouchi, MD,1 Akihiko Asami, MD, PhD,2 Hisato Tanaka, MD,3 PhD, Norihiko Nogami, MD, PhD4 1Department of Rehabilitation Medicine, Saga University Hospital, Saga, Japan. 2Saga Social Insurance Hospital, Saga, Japan. 3Tanaka Hospital (Anju Medical Corporation), Saga, Japan. 4Wakakusu Ryoikuen, Tosu, Saga, Japan. ABSTRACT life disability. The rate of effectiveness of LX-P against Asami T, Yamanouchi N, Asami A, Tanaka H, Nogami pain-related disabilities in the fourth week was 62.2%. N. The effectiveness of patches containing Loxoprofen Conclusion: LX-P showed satisfactory analgesic Sodium Hydrate (LX-P) in the conservative therapy of effect and QOL improvement. We believe it is effective muscular back pain - Clinical results using the Japanese for clinical practice. Orthopaedic Association Back Pain Evaluation Keywords: loxoprofen sodium, JOABPEQ, VAS, Questionnaire (JOABPEQ). Jpn J Compr Rehabil Sci QOL, muscular back pain 2013; 4: 22-29. Objectives: We investigated the analgesic effect, Introduction degree of patient satisfaction, and QOL improvement provided by patches containing loxoprofen sodium According to the Ministry of Health, Labour and hydrate (LX-P) using a questionnaire based on the Welfare’s Comprehensive Survey of Living Conditions evaluation criteria of the Japanese Orthopaedic (several surveys conducted in fiscal 2004, 2007, 2010), Association Back Pain Evaluation Questionnaire pain in the locomotive organs, including “lower back (JOABPEQ). pain,” “stiff shoulders,” and “joint pain,” is one of the Methods: In this study of 53 patients (18 men, 35 most common subjective symptoms reported.