Thesis Biochemistry By
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Phase II Study of the Novel Proteasome Inhibitor Bortezomib In
Memorial Sloan-Kettering Cance r Center IRB Protocol IRB#: 05-103 A(14) A Phase II Study of the Novel Proteas ome Inhibitor Bortezomib in Combination with Rituximab, Cyclophosphamide and Prednisone in Patients with Relapsed/Refractory I Indolent B-cell Lymphoproliferative Disorders and Mantle Cell Lymphoma (MCL) MSKCC THERAPEUTIC/DIAGNOSTIC PROTOCOL Principal Investigator: John Gerecitano, M.D., Ph.D. Co-Principal Carol Portlock, M.D. Investigator(s): IFormerly: A Phase I/II Study of the Nove l Proteasome Inhibitor Bortezomib in Combinati on with Rituximab, Cyclophosphamide and Prednisone in Patients with Relapsed/Refractory Indolent B-cell Lymphoproliferative Disorders and Mantle Cell Lymphoma (MCL) Amended: 07/25/12 Memorial Sloan-Kettering Cance r Center IRB Protocol IRB#: 05-103 A(14) Investigator(s): Paul Hamlin, M.D. Commack, NY Steven B. Horwitz, M.D. Philip Schulman, M.D. Alison Moskowitz, M.D. Stuart Lichtman, M.D Craig H. Moskowitz, M.D. Stefan Berger, M.D. Ariela Noy, M.D. Julie Fasano, M.D. M. Lia Palomba, M.D., Ph.D. John Fiore, M.D. Jonathan Schatz, M.D. Steven Sugarman, M.D David Straus, M.D. Frank Y. Tsai, M.D. Andrew D. Zelenetz, M.D., Ph.D. Matthew Matasar, M.D Rockville Center, NY Mark L. Heaney, M.D., Ph.D. Pamela Drullinksy, M.D Nicole Lamanna, M.D. Arlyn Apollo, M.D. Zoe Goldberg, M.D. Radiology Kenneth Ng, M.D. Otilia Dumitrescu, M.D. Tiffany Troso-Sandoval, M.D. Andrei Holodny, M.D. Sleepy Hollow, NY Nuclear Medicine Philip Caron, M.D. Heiko Schoder, M.D. Michelle Boyar, M.D. -
Cardiac Events During Treatment with Proteasome Inhibitor Therapy for Multiple Myeloma John H
Chen et al. Cardio-Oncology (2017) 3:4 DOI 10.1186/s40959-017-0023-9 RESEARCH Open Access Cardiac events during treatment with proteasome inhibitor therapy for multiple myeloma John H. Chen1*, Daniel J. Lenihan2, Sharon E. Phillips3, Shelton L. Harrell1 and Robert F. Cornell1 Abstract Background: Proteasome inhibitors (PI) bortezomib and carfilzomib are cornerstone therapies for multiple myeloma. Higher incidence of cardiac adverse events (CAEs) has been reported in patients receiving carfilzomib. However, risk factors for cardiac toxicity remain unclear. Our objective was to evaluate the incidence of CAEs associated with PI and recognize risk factors for developing events. Methods: This was a descriptive analysis of 96 patients with multiple myeloma who received bortezomib (n = 44) or carfilzomib (n = 52). We compared the cumulative incidence of CAEs using a log rank test. Patient-related characteristics were assessed and multivariate analysis was used to identify risk factors for developing CAEs. Results: PI-related CAEs occurred in 21 (22%) patients. Bortezomib-associated CAEs occurred in 7 (16%) patients while carfilzomib-associated cardiac events occurred in 14 (27%) patients. The cumulative incidence of CAEs was not significantly different between agents. Events occurred after a median of 67.5 days on PI therapy. Heart failure was the most prevalent event type. More patients receiving carfilzomib were monitored by a cardiologist. By multivariate analysis, a history of prior cardiac events and longer duration of PI therapy were identified as independent risk factors for developing CAEs. Conclusions: AEs were common in patients receiving PIs. Choice of PI did not impact the cumulative incidence of CAEs. -
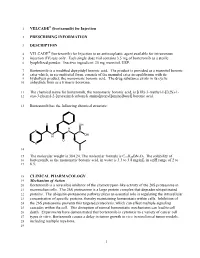
VELCADE® (Bortezomib) for Injection
1 VELCADE® (bortezomib) for Injection 2 PRESCRIBING INFORMATION 3 DESCRIPTION 4 VELCADE® (bortezomib) for Injection is an antineoplastic agent available for intravenous 5 injection (IV) use only. Each single dose vial contains 3.5 mg of bortezomib as a sterile 6 lyophilized powder. Inactive ingredient: 35 mg mannitol, USP. 7 Bortezomib is a modified dipeptidyl boronic acid. The product is provided as a mannitol boronic 8 ester which, in reconstituted form, consists of the mannitol ester in equilibrium with its 9 hydrolysis product, the monomeric boronic acid. The drug substance exists in its cyclic 10 anhydride form as a trimeric boroxine. 11 The chemical name for bortezomib, the monomeric boronic acid, is [(1R)-3-methyl-1-[[(2S)-1- 12 oxo-3-phenyl-2-[(pyrazinylcarbonyl) amino]propyl]amino]butyl] boronic acid. 13 Bortezomib has the following chemical structure: O OH H N N B N OH H O N 14 15 The molecular weight is 384.24. The molecular formula is C19H25BN4O4. The solubility of 16 bortezomib, as the monomeric boronic acid, in water is 3.3 to 3.8 mg/mL in a pH range of 2 to 17 6.5. 18 CLINICAL PHARMACOLOGY 19 Mechanism of Action 20 Bortezomib is a reversible inhibitor of the chymotrypsin-like activity of the 26S proteasome in 21 mammalian cells. The 26S proteasome is a large protein complex that degrades ubiquitinated 22 proteins. The ubiquitin-proteasome pathway plays an essential role in regulating the intracellular 23 concentration of specific proteins, thereby maintaining homeostasis within cells. Inhibition of 24 the 26S proteasome prevents this targeted proteolysis, which can affect multiple signaling 25 cascades within the cell. -

Combining Milatuzumab with Bortezomib, Doxorubicin, Or Dexamethasone Improves Responses in Multiple Myeloma Cell Lines Rhona Stein,1Mitchell R
CancerTherapy: Preclinical Combining Milatuzumab with Bortezomib, Doxorubicin, or Dexamethasone Improves Responses in Multiple Myeloma Cell Lines Rhona Stein,1Mitchell R. Smith,2 Susan Chen,1Maria Zalath,1and David M. Goldenberg1 Abstract Purpose: The humanized anti-CD74 monoclonal antibody, milatuzumab, is in clinical evaluation for the therapy of multiple myeloma (MM). The ability of milatuzumab to increase the efficacy of bortezomib, doxorubicin, and dexamethasone was examined in three human CD74+ MM cell lines, CAG, KMS11, KMS12-PE, and one CD74-MM cell line, OPM-2. Experimental Design: Activity of milatuzumab as a monotherapy and combined with the drugs was evaluated by studying in vitro cytotoxicity, signaling and apoptotic pathways, and in vivo therapeutic activity in severe combined immunodeficient (SCID) mouse models of MM. Results: Given as a monotherapy, cross-linked milatuzumab, but not milatuzumab alone, yielded sig- nificant antiproliferative effects in CD74+ cells.The combination of cross-linked milatuzumab with bortezomib, doxorubicin, or dexamethasone caused more growth inhibition than either cross-linked milatuzumab or drug alone, producing significant reductions in the IC50 of the drugs when combined. Efficacy of combined treatments was accompanied by increased levels of apoptosis measured by increases of activated caspase-3 and hypodiploid DNA. Both milatuzumab and bortezomib affect the nuclear factor-nB pathwayinCAGMMcells. In CAG-or KMS11-SCIDxenograftmodels ofdisseminated MM, milatuzumab more than doubled median survival time, compared withup to a 33% increase in median survival withbortezomib but no significant benefit with doxorubicin. Moreover, combining milatuzumabandbortezomibincreasedsurvivalsignificantlycomparedwitheither treatmentalone. Conclusions:The therapeutic efficacies of bortezomib, doxorubicin, and dexamethasone are en- hanced in MM cell lines when given in combination with milatuzumab, suggesting testing these combinations clinically. -

Enhances the Susceptibility to Viral Infection the Proteasome Inhibitor
The Proteasome Inhibitor Bortezomib Enhances the Susceptibility to Viral Infection Michael Basler, Christoph Lauer, Ulrike Beck and Marcus Groettrup This information is current as of September 27, 2021. J Immunol 2009; 183:6145-6150; Prepublished online 19 October 2009; doi: 10.4049/jimmunol.0901596 http://www.jimmunol.org/content/183/10/6145 Downloaded from References This article cites 50 articles, 23 of which you can access for free at: http://www.jimmunol.org/content/183/10/6145.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 27, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2009 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology The Proteasome Inhibitor Bortezomib Enhances the Susceptibility to Viral Infection1 Michael Basler,2*† Christoph Lauer,† Ulrike Beck,† and Marcus Groettrup*† The proteasome, a multicatalytic protease, is responsible for the generation of most MHC class I ligands. Bortezomib, a protea- some inhibitor, is clinically approved for treatment of multiple myeloma and mantle cell myeloma. -

A Novel Proteasome Inhibitor NPI-0052 As an Anticancer Therapy
British Journal of Cancer (2006) 95, 961 – 965 & 2006 Cancer Research UK All rights reserved 0007 – 0920/06 $30.00 www.bjcancer.com Minireview A novel proteasome inhibitor NPI-0052 as an anticancer therapy 1 1 ,1 D Chauhan , T Hideshima and KC Anderson* 1Department of Medical Oncology, Harvard Medical School, Dana Farber Cancer Institute, The Jerome Lipper Multiple Myeloma Center, Boston, MA 02115, USA Proteasome inhibitor Bortezomib/Velcade has emerged as an effective anticancer therapy for the treatment of relapsed and/or refractory multiple myeloma (MM), but prolonged treatment can be associated with toxicity and development of drug resistance. In this review, we discuss the recent discovery of a novel proteasome inhibitor, NPI-0052, that is distinct from Bortezomib in its chemical structure, mechanisms of action, and effects on proteasomal activities; most importantly, it overcomes resistance to conventional and Bortezomib therapies. In vivo studies using human MM xenografts shows that NPI-0052 is well tolerated, prolongs survival, and reduces tumour recurrence. These preclinical studies provided the basis for Phase-I clinical trial of NPI-0052 in relapsed/ refractory MM patients. British Journal of Cancer (2006) 95, 961–965. doi:10.1038/sj.bjc.6603406 www.bjcancer.com & 2006 Cancer Research UK Keywords: protein degradation; proteasomes; multiple myeloma; novel therapy; apoptosis; drug resistance The systemic regulation of protein synthesis and protein degrada- inducible immunoproteasomes b-5i, b-1i, b-2i with different tion is essential -

The Combined Effects of Proteasome Inhibitor Bortezomib with Topoisomerase I and II Inhibitors on Topoisomerase Enzymes
Turkish Journal of Medical Sciences Turk J Med Sci (2016) 46: 1882-1888 http://journals.tubitak.gov.tr/medical/ © TÜBİTAK Research Article doi:10.3906/sag-1511-184 The combined effects of proteasome inhibitor bortezomib with topoisomerase I and II inhibitors on topoisomerase enzymes Emine ÖKSÜZOĞLU*, Çiydem TIRINOĞLU, Barış KERİMOĞLU Molecular Biology Division, Department of Biology, Faculty of Science and Letters, Aksaray University, Aksaray, Turkey Received: 29.11.2015 Accepted/Published Online: 17.02.2016 Final Version: 20.12.2016 Background/aim: DNA topoisomerases are ubiquitous enzymes that regulate conformational changes in DNA topology during essential cellular processes, and, for this reason, have been characterized as the cellular targets of a number of anticancer drugs. Bortezomib is a powerful proteasome inhibitor used in the treatment of hematological malignancies. In this study, we investigated the inhibitory effects of bortezomib on human topoisomerase I and II enzymes both alone and in combination modes with camptothecin and etoposide. Materials and methods: The interactions of these drugs with topoisomerase enzymes were evaluated by relaxation assay in cell-free systems. IC50 values of the drugs on topoisomerase enzymes were calculated using the S probit analysis program. Results: Bortezomib showed a very weak inhibition effect on topoisomerase I (IC50 = 87.11 mM). On the other hand, it had a strong inhibitory effect on topoisomerase II (IC50 = 1.41 mM). Our results indicated that bortezomib is effective not only on proteasome but also on topoisomerase II. In addition, bortezomib possesses an increased synergistic effect when used in combination with camptothecin and etoposide than when used alone. Conclusion: The results of this study point out that these data may build a framework for combination studies with bortezomib, camptothecin, and etoposide in the treatment of cancer. -

Antitumor Effects of Bortezomib (PS-341) on Primary Effusion Lymphomas
Leukemia (2004) 18, 1699–1704 & 2004 Nature Publishing Group All rights reserved 0887-6924/04 $30.00 www.nature.com/leu Antitumor effects of bortezomib (PS-341) on primary effusion lymphomas JAn1, Y Sun1, M Fisher1 and MB Rettig1,2 1VA Greater Los Angeles Healthcare System, Los Angeles, CA 90073, USA; and 2Department of Medicine, David Geffen School of Medicine at UCLA, Los Angeles, CA 90095, USA Primary effusion lymphomas (PELs) are a rare type of non- treatment of refractory multiple myeloma, where it has an Hodgkin’s lymphoma that are resistant to cytotoxic chemother- acceptable toxicity profile.4–6 By inhibiting the proteasome, apy. PELs manifest constitutive activation of nuclear factor kappa B (NF-jB), and inhibition of NF-jB induces apoptosis of which degrades proteins that are marked by ubiquitination, PELs and sensitizes to tumor necrosis factor-related apoptosis- bortezomib modulates the cellular concentrations of hundreds inducing ligand (TRAIL)-induced death. Bortezomib (PS-341), a of proteins that are involved in a wide variety of functions, peptidyl boronic acid inhibitor of the proteasome, is a potent including cell cycle progression, signal transduction, and agent against a wide range of hematologic malignancies and apoptosis.7,8 For example, the proteasome regulates the activity has been shown to inhibit NF-jB. Thus, we examined the of the NF-kB pathway, in that the degradation of I kappa B (IkB), cytotoxic effects of bortezomib alone and in combination with the NF-kB inhibitory protein, is dependent upon the ubiquitin– various drugs. Bortezomib potently inhibited NF-jB in PEL cells 9 in a dose-dependent manner. -

Bortezomib Plus Docetaxel in Advanced Non-Small Cell Lung Cancer and Other Solid Tumors: a Phase I California Cancer Consortium Trial
CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector ORIGINAL ARTICLE Bortezomib Plus Docetaxel in Advanced Non-small Cell Lung Cancer and Other Solid Tumors: A Phase I California Cancer Consortium Trial Primo N. Lara, Jr., MD,*† Mariana Koczywas, MD,‡ David I. Quinn, MD, PhD,§ Heinz Josef Lenz, MD,§ Angela M. Davies, MD,* Derick H.M. Lau, MD, PhD,*† Paul H. Gumerlock, PhD,* Jeff Longmate, PhD,‡ James H. Doroshow, MD,‡ David Schenkein, MD,͉͉ Oscar Kashala, MD,͉͉ and David R. Gandara, MD*† n recent years, the inhibition of the 26S proteasome has Background: This phase I study was performed to determine the emerged as a rational anti-neoplastic strategy. The 26S dose-limiting toxicity and maximum tolerated dose (MTD) of do- I proteasome is a very large proteolytic complex involved in a cetaxel in combination with bortezomib in patients with advanced non-small cell lung cancer (NSCLC) or other solid tumors. significant catabolic pathway, the ubiquitin–proteasome path- way, for many intracellular regulatory proteins, including IB Methods: Patients were enrolled in cohorts of three over six dose levels. Each treatment cycle was 3 weeks long and consisted of one kinase/nuclear factor- B(I B/NF- B), p53, and the cyclin- docetaxel infusion (day 1) and four bortezomib injections (days 1, 4, dependent kinase inhibitors p21 and p27, which contribute to 8, and 11). Dose escalation and MTD determination were based on the regulation of the cell cycle, apoptosis, and angiogene- 1–3 the occurrence of dose-limiting toxicities in cycle 1 only. -

Proteasome Inhibitor-Adapted Myeloma Cells Are Largely
Leukemia (2016) 30, 2198–2207 OPEN © 2016 Macmillan Publishers Limited, part of Springer Nature. All rights reserved 0887-6924/16 www.nature.com/leu ORIGINAL ARTICLE Proteasome inhibitor-adapted myeloma cells are largely independent from proteasome activity and show complex proteomic changes, in particular in redox and energy metabolism GP Soriano1,4, L Besse2,4,NLi1, M Kraus2, A Besse2, N Meeuwenoord1, J Bader2, B Everts3, H den Dulk1, HS Overkleeft1, BI Florea1 and C Driessen2 Adaptive resistance of myeloma to proteasome inhibition represents a clinical challenge, whose biology is poorly understood. Proteasome mutations were implicated as underlying mechanism, while an alternative hypothesis based on low activation status of the unfolded protein response was recently suggested (IRE1/XBP1-low model). We generated bortezomib- and carfilzomib-adapted, highly resistant multiple myeloma cell clones (AMO-BTZ, AMO-CFZ), which we analyzed in a combined quantitative and functional proteomic approach. We demonstrate that proteasome inhibitor-adapted myeloma cells tolerate subtotal proteasome inhibition, irrespective of a proteasome mutation, and uniformly show an 'IRE1/XBP1-low' signature. Adaptation of myeloma cells to proteasome inhibitors involved quantitative changes in 4600 protein species with similar patterns in AMO-BTZ and AMO-CFZ cells: proteins involved in metabolic regulation, redox homeostasis, and protein folding and destruction were upregulated, while apoptosis and transcription/translation were downregulated. The quantitatively most upregulated protein in AMO-CFZ cells was the multidrug resistance protein (MDR1) protein ABCB1, and carfilzomib resistance could be overcome by MDR1 inhibition. We propose a model where proteasome inhibitor-adapted myeloma cells tolerate subtotal proteasome inhibition owing to metabolic adaptations that favor the generation of reducing equivalents, such as NADPH, which is supported by oxidative glycolysis. -

The Proteasome Metabolizes Peptide-Mediated Nonviral Gene Delivery Systems
Gene Therapy (2005) 12, 1581–1590 & 2005 Nature Publishing Group All rights reserved 0969-7128/05 $30.00 www.nature.com/gt RESEARCH ARTICLE The proteasome metabolizes peptide-mediated nonviral gene delivery systems J Kim, C-P Chen and KG Rice Division of Medicinal and Natural Product Chemistry, College of Pharmacy, University of Iowa, Iowa City, IA, USA The proteasome is a multisubunit cytosolic protein complex directly with proteasome inhibition, and was not the result of responsible for degrading cytosolic proteins. Several studies lysosomal enzyme inhibition. The enhanced transfection was have implicated its involvement in the processing of viral specific for peptide DNA condensates, whereas Lipofecta- particles used for gene delivery, thereby limiting the mine- and polyethylenimine-mediated gene transfer were efficiency of gene transfer. Peptide-based nonviral gene significantly blocked. A series of novel gene transfer peptides delivery systems are sufficiently similar to viral particles in containing intrinsic GA proteasome inhibitors (CWK18(GA)n, their size and surface properties and thereby could also be where n ¼ 4, 6, 8 and 10) were synthesized and found to recognized and metabolized by the proteasome. The present inhibit the proteasome. The gene transfer efficiency mediated study utilized proteasome inhibitors (MG 115 and MG 132) by these peptides in four different cell lines established that a to establish that peptide DNA condensates are metabolized GA repeat of four is sufficient to block the proteasome and by the proteasome, thereby limiting their gene transfer significantly enhance the gene transfer. Together, these efficiency. Transfection of HepG2 or cystic fibrosis/T1 (CF/T1) results implicate the proteasome as a previously undiscov- cells with CWK18 DNA condensates in the presence of ered route of metabolism of peptide-based nonviral gene MG 115 or MG 132 resulted in significantly enhanced gene delivery systems and provide a rationale for the use of expression. -

Velcade, INN-Bortezomib
SCIENTIFIC DISCUSSION This module reflects the initial scientific discussion for the approval of Velcade. This scientific discussion has been updated until 1 May 2004. For information on changes after this date please refer to module 8. 1. Introduction Multiple myeloma Multiple myeloma is a B-cell malignancy of the plasma cell and represents the second most common hematological malignancy, with non-Hodgkin’s lymphoma being the most common. The incidence and prevalence of multiple myeloma are similar in the US and Europe. In 2000, there were approximately 19,000 cases diagnosed in the European Economic Area (Globocan, 2000), with a 5- year prevalence of approximately 47,000 cases. The course of multiple myeloma is characterized by an asymptomatic or subclinical phase before diagnosis (possibly for several years), a chronic phase lasting several years, and an aggressive terminal phase. Multiple myeloma leads to progressive morbidity and eventual mortality by lowering resistance to infection and causing significant skeletal destruction (with bone pain, pathological fractures, and hypercalcemia), anemia, renal failure, and, less commonly, neurological complications and hyperviscosity. From the time of diagnosis, the survival without treatment is between 6 to 12 months and extends to 3 years with chemotherapy. Approximately 25% of patients survive 5 years or longer, with fewer than 5% surviving longer than 10 years. Approved anticancer agents for the treatment of myeloma in the US include melphalan (1992), carmustine (BCNU, 1977) and cyclophosphamide (1959) and in addition, in Europe, epirubicin is also approved for treatment of this disease. At the time of diagnosis, multiple myeloma is a heterogeneous disease, with a course that varies on the basis of both disease- and host-related factors (e.g., age, renal function, stage, alpha2- microglobulin, chromosomal abnormalities).