A Twenty-Year Audit of Herpes Zoster in Asia-Pacific
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2021 – 22 Budget
2021 – 22 FISCAL YEAR BUDGET Operating Budget | Capital Improvement Program Strategic Digital Transformation Program Budget preparation team Finance team Brigid Drury, Senior Accountant Bridget Desmarais, Management Analyst Marcelo Penha, Senior Management Analyst Ryan Green, Finance Director Leadership team Scott Chadwick, City Manager Celia Brewer, City Attorney Geoff Patnoe, Assistant City Manager Gary Barberio, Deputy City Manager, Community Services Paz Gomez, Deputy City Manager, Public Works Laura Rocha, Deputy City Manager, Administrative Services Mike Calderwood, Chief, Fire Department Maria Callander, Director, Information Technology Sheila Cobian, Assistant to the City Manager, Office of the City Manager Tom Frank, Director, Public Works Transportation Morgen Fry, Executive Assistant, Office of the City Manager Neil Gallucci, Chief, Police Department David Graham, Chief Innovation Officer, Innovation & Economic Development Ryan Green, Director, Finance Jason Haber, Director, Intergovernmental Affairs, Office of the City Manager Kyle Lancaster, Director, Parks & Recreation John Maashoff, Manager, Public Works Facilities & Fleet Faviola Medina, City Clerk Services Manager, Office of the City Clerk Jeff Murphy, Director, Community Development Suzanne Smithson, Director, Library & Cultural Arts Vicki Quiram, Director, Public Works Utilities Kristina Ray, Director, Communication & Engagement Baq Taj, Engineering Manager, Public Works Construction Management & Inspections Judy Von Kalinowski, Director, Human Resources James Wood, -

Jaf Leaders Omured by Bomb in Shanghai
-5‘ - : ‘.v; V AVKRAOB DAJLT OIBOULATION for tlie Moatk of Maroh, IMS 5 r 5 3 0 liM iber of Audit Bnreaa of (Xrculotloo. (EIGHTEEN PAGES) (UlMilfled AdvertIMag oa Pag* I**) SOOTH MANCHE8TBB, CONN, FRIDAY, APRIL 2», 1932. VOL. U ., NO. 180. JURY DEADLOCKED When Inventors Are Left to Their Own Devices JAF LEADERS OMURED IN THE MASSIE CASE BY BOMB IN SHANGHAI Jnrors Oat Nearly 30 Hoars DR. DOLAN WINS Two Bay State Women Two Generals, As A M n i Withoat Reaching Deci LOCAL CAUCUS aid Two 1 ^ Raildig sion — Mrs. Forlescne Are Burned to Death Djpkmto Hvt Wide Ro* Seems To Be Cheerfnl. FOR ROOSEVELT Tiewigg MiGtanr Parade Mount Dora, Fla., April 29.— (A P )^ h en the fire started, but ran Into —Two felderly Massachusetts wo toe biiilding to save their personal Honolulu, April 29— (AP) — Ap Democrats Here Sapport men were fatally burned in a fire belongings. Trapped on the second In Honor of Japanese Em parently deadlocked the 12 men that destroyed two residences at floor. Miss Tillie Kelley stumbled striving for a verdict in the case of Tangerine, FIA, near here, yester and perished before aid could reach peror's BirAday—B ort four persons accused of the lynch Leader — Delegates Not day. her. ing of Joseph Kahahawal carried on Miss ’Tlllle Kelley, 70, of Otter The fire followed an explosion in today after having given watchers lostracted Bat All Are Fa River, Mass., was trapped In the an adjacent garage. Thrower, a Korean, Badly a few tantalizing glimpses of their flames and perished and her cousin. -

The Thai Popular Music Industry
THE THAI POPULAR MUSIC INDUSTRY: INDUSTRIAL FORM AND MUSICAL DESIGN NALIN WUTTIPONG, BFA, M Mus Thesis submitted to the University of Nottingham for the degree of Doctor of Philosophy SEPTEMBER 2011 o ABSTRACT Popular music, as it is generally defined in its commercial existence, originated in the West and has been widely discussed in Anglophone academia. One of the key means of approaching it is in terms of political economy, by viewing the culture industry essentially as a model of capitalism, with the purpose of maximizing profit [Bumett, 1996; Frith, Straw and Street, 2001]. The debates between political economists and other popular music scholars have predominantly taken as their subject Western popular music. Yet it is important to point out that whilst studies focused upon cultural industries outside of Western contexts have been few and far between, many have proved extremely fruitful and enlightening, exploring issues not considered in Western-centered accounts. This dissertation will attempt to examine and describe the causes and effects of corporate control over the major labels, which have been influential in the Thai popular music industry since 1982, when the first major label was established. Furthermore, this dissertation will argue that the popular music industry in Thailand presents something ofa variation on Adorno's theme of mass culture, replicating certain aspects of his description while also diverging in important ways. The study of the development of Thai popular music in this dissertation can be divided into five important periods: the Pre-pop Era (from the emergence of The Impossible to 1982) and the Pop Era (1982-1994), the Indie Phenomenon (1994-1997), the Major Retum (1997-2002) and the present day (2002 to today). -
An Overview of the Market for Alcoholic Beverages of Potentially Particular Appeal to Minors
An overview of the market for alcoholic beverages of potentially particular appeal to minors Specific Services No EAHC/2010/Health/14 Specific Contract No 2010 62 91 Edited by: Peter Anderson, Marc Suhrcke, and Chris Brookes This report was produced under the Health Programme (2008-2013) in the framework of a contract with the Executive Agency for Health and Consumers (EAHC) acting on behalf of the European Commission. The content of this report represents the views of National Heart Forum (HAPI Consortium) and is its sole responsibility; it can in no way be taken to reflect the views of the European Commission and/or the EAHC or any other body of the European Union. The European Commission and/or the EAHC do not guarantee the accuracy of the data included in this report, nor do they accept responsibility for any use made by third parties thereof. Keywords Alcohol; Minor; Market; Communications; ESPAD This report should be quoted as: Anderson P, Suhrcke M and Brookes C (2012) An overview of the market for alcohol beverages of potentially particular appeal to minors. London: HAPI. © EC/EAHC 2012 CONTENTS Acknowledgements i About the editors i Acronyms ii Chapter 1 Introduction 1 Chapter 2 Sales 6 Chapter 3 Drinking patterns and their drivers 16 Chapter 4 Country case studies 21 Chapter 5 Product case studies 35 Chapter 6 Conclusions 49 Annex A Supplement to Chapter 2 52 Annex B Supplement to Chapter 3 69 Annex C Supplement to Chapter 4 109 Annex D Supplement to Chapter 5 123 Annex E Data needs 131 Page i Acknowledgements The National Heart Forum (NHF) and the Health Action Partnership International (HAPI) are grateful to the European Commission for the financial support towards the production of this report. -

Muscle-Powered Soft Robotic Ventricular Assist Devices
Muscle-powered Soft Robotic Ventricular Assist Devices Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Engineering Jooli Han B.E., Biomedical Engineering, State University of New York M.S., Biomedical Engineering, State University of New York Carnegie Mellon University Pittsburgh, PA November 2020 © Jooli Han, 2020 All Rights Reserved Acknowledgements I am thankful for everyone that took parts in this meaningful journey towards a doctorate degree. I would like to thank my doctoral advisor, Professor Dennis R. Trumble, Ph.D., for his guidance in academics and in life throughout my time here at Carnegie Mellon University. He pushed me forward by living an example and sharing bits of life wisdom. It has been a privilege to have a caring, warm-hearted mentor who supervises his lab with great respect. Thanks to his unfailing patience and support, I was able to maintain a high standard of excellence and forge my own path independently. I would like to thank my thesis committee members for ensuring my research in the right direction. Professor Keith E. Cook, Ph.D. and Professor Conrad M. Zapanta, Ph.D. from Biomedical Engineering Department, Professor Carmel Majidi, Ph.D. from Mechanical Engineering Department, and Dr. Michael Scott Halbreiner, M.D. from Allegheny General Hospital generously shared their time and expertise. Without their critical questions and opinions, this thesis would not have been completed. I cannot express how lucky I am to have been a part of the Biomedical Engineering Department of Carnegie Mellon University. Thank you, faculty and staff, especially Maryia, Keri, Misti, and Kristin, for making the friendly and supportive environment to live in every day. -
Universiv International
INFORMATION TO USERS This reproduction was made from a copy o f a document sent to us for microfilming. While the most advanced technology has been used to photograph and reproduce tliis document, the quality o f the reproduction is heavily dependent upon the quality of the material submitted. The following explanation of techniques is provided to help clarify markings or notations which may appear on this reproduction. 1.The sign or “target” for pages apparently lacking from the document photographed is “Missing Page(s)” . I f it was possible to obtain the missing page(s) or section, they are spliced into the film along with adjacent pages. This may have necessitated cutting through an image and duplicating adjacent pages to assure complete continuity. 2. When an image on the film is obliterated with a round black mark, it is an indication o f either blurred copy because of movement during exposure, duplicate copy, or copyrighted materials that should not have been filmed. For blurred pages, a good image of the page can be found in the adjacent frame. If copyrighted materials were deleted, a target note will appear listing the pages in the adjacent frame. 3. When a map, drawing or chart, etc., is part o f the material being photographed, a definite method of “sectioning” the material has been followed. It is customary to begin filming at the upper left hand comer o f a large sheet and to continue from left to right in equal sections with small overlaps. I f necessary, sectioning is continued again—beginning below the first row and continuing on until complete. -
Student Scores Not As Good As They Can
Vol.16, No. 40 Friday, October 5, 2001 50 cents f Student scores •aaaaaaaaaaut-^^" -, //' ^aK^V M5M' - '^laaaaaaaaaaaaaaaaV^..aB - te fafe:.. •..• , not as good as l^^gRlralaa^BBBBBBES^BBB they can be? By THOMAS SCOTT writing. We would have liked to TllEUKf'OUD-l'KKSS see more breakdown by the state * mUl Assistant Superintendent of fj WESTFIELD - Nearly nil dis- Human Resources, Dr, Margaret trict fourth-graders scored above Dolun, "Wi> would have liked a stato standards on the scoring on vocabulary, literal and Elementary School Proficiency inferred moaning, and more of a Westfield's Danielle Coleman fin- Assessment (ESPA) tests admin- focus on mechanics." ished third at second singles in / ^jstohk ^aaat.c': ••; istered last May, school officials District educators want to raise die Union County Tournament :-:',^sVleaaBulaaal said lust week, but administra- tho bar for kids who test profi- Tuesday. Westfleld won the team tors arc still looking to got- a han- cient, but not- advanced proficient, title by beating Summit by a point, dle on ways to improve scon's. (in the tests. 6847. See story on Page C-1. BB^BBBBBBwRl^aHF -. • • • - /n M Scores for Language Arts, In tho area of Language Arta, Mathematics and Science we 99 for instance, (i9.2 percent of dis- percent, 94.4 percent, and 99.5 trict students scored proficient m percent respectively. while 2\).S percent scored ; ; .:•' •••'.;" •»-,. "v.--"- •'...;•'"_ '.'.!-.'••• ; • — ' .;- ;;- Despite the strong scores, advanced proficient. District Briefs t school administrators said the ndminintrutors want to improve - :' -• '• :' .••;• \'-:.'-'" .=.'"•'•'-•'• •*.'.- ; '•"!""••'.••' •'•'.•-•:.•• type of data provided by the stale the numbers by addressing GEORGE PACCIELLO/STAFF F3H0TOQRAPHER was limited and handicapped .strengths and/or weaknesses in Free bowling party their efforts to analyze the results llie curriculum. -

Resource / 6.81 MB
JANUARYJ f877. BY MRs. BooTH. t'L' "And herein do I exercise myself, to have always a conscience void of offence .. toward God and toward men."- .A.c:rs xxiv. lG . 0 ~-- "iwjERHAPS there is no complaint more frequently on the lips ·r·) of those who mourn over leanness of soul than this : "1\fy "' .:J:; fnith is so weak: I want more faith"; nncl doubtless a weak ~:~ iitith is the Rccrct of a great deal of the barrenness and misery t-'* of IIIIUIY Christians; but it never seems to occur to them to 1\Rk Wl;Y lhl'ir faith is weak? WIIY the\' find themselves JlOWI'rl cRs to npp1·oprinto the promises of God? "Yes,'' said a dying lm<'kH iid ('l' to IL uum of God who was trying to comfort him by quoting the promises ; "yes, I believe they are true, but somehow they won't stick ! " The fault was in the state of his own heart. 1Ie could not appropriate the promises, because he knew that he wns not the character to whom they were made. Now it seems to me that a great deal of failure in faith is simply the result of a defiled conscience, and if those who find themselves weak nud sickly in spiritual life would turn their attention to the condition of their .:onsciences they would soon discover the reason for all their fnilure. The fact is, we have a great deal of so·called Christianity in these days which dispenses with conscience altogether. \Ve sometimes meet with persons who tell us that they are not under the law, but unde1· grace,· and therefore they are not condemned, do what they will. -

White House Staff
I WHITE HOUSE Staff Book 1953-61 _ ___________N ~ 16~ __J I 1600 PENNSYLVANIA AVENUE, WASHJNGTON, D. C. NOT£ 1'0 READER: In the section devoted to bioi;ir aphietJ, you ma.y regret the omi:uion or ccrt:tin awards, cit.itlon&, decorations, honorary dcgrcc11 .tnd ach,icvcmcnts of one. 1;on or another, including dirccton\tcs, writings, speeches, special mluior1.&, confer ences, golf scorcil, £ish c~1,1g ht, an.d other pdde(ul thlngs. The6e are not inadve rLO::nces. The cditou d~cided to keep all 6tafi bio14: raplt1t~8 to a bare m ini..tnum; t r ying 11:iroply to de1;cribe the background and qua.Ji£ic;1Uion3 o f those wbo served the President or the United State& of Arnedca. Moreover, o(fcn$e WM deliberately risked by not usmg glamour-t)'l)C phot.Qgr.;i.ph• supplied in some inatan(:.Cf, favoring itt&tead - - again for the sake ofuniformity- lht- plain passport 11-bou from tbe of.flclal Wb..ite House paases. Dissatisfied !tub- 1J(:.riberi; may appl y for a refund b>• wr-iting The Editor s at the above addrc11-, any time aJter Janua ry 20, 1961. Dwight 0. £benhowcT DUTY • HONOR • COUNTRY ,c,<iW(IO¾. A Staff has no ex.istenct! independent of the person "stilled. " Whatever authority. • <\,,'l, wl:i..itevcr lnfiucnec, whatever eifective,ness, i :I a 51..l-Ci mil)' have ls purel>• derivative, In a<:.knowlcdgiog thls, the Ed.Hora have i n • t i c;.h,1dcd one biography - - ln fronl of the others -- that obvlou,ly do<:s not beloog in ..(ltot,14 a White Hou,c "St.lfl Book" but wilhout whom there would be no bc;,ok jn t b.c Ciut place, I.I t hh were the luo.ct of volu.tne tha t c ould, without presumption. -
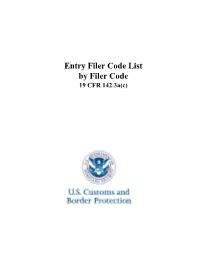
Filer Code List Sorted by Filer Code
Entry Filer Code List by Filer Code 19 CFR 142.3a(c) U.S. Customs and Border Protection FILER-CODE FILER-NAME 002 JF MORAN CO INC 003 PORTER INTERNATIONAL INC. 004 CEVA INTERNATIONAL, INC. 006 PACIFIC CUSTOMS HOUSE BROKERS 007 MARVIN H PARKER INC 008 PORT BROKERS INC 009 QUAST & CO 010 REEDY FORWARDING CO 011 ROYAL FREIGHT BROKERS 012 SHANNON BROKERAGE CO. 014 WILMINGTON SHIPPING COMPANY 015 WM STONE & CO 016 TRANS OVERSEAS 017 UNIVERSAL TRANSCONTINENTAL CORP 018 E.C. MCAFEE 019 SEAIR EXPRESS OF SAN FRANCISCO 020 JAGRO CUSTOMS BROKERS & INTL. F.F., 022 GOFF & PAGE CO 024 EXPORT-IMPORT SERVICES, INC. 026 T D DOWNING CO 028 KEYNOTE CARGO CLEARANCE 029 CARL & STARTARE 031 B & D CUSTOMHOUSE BROKERS, INC. 032 AJ ARANGO 034 AIRSPED INC 035 AERO SPACE CARGO INC 036 E SIDNEY STOCKWELL CO INC 037 W. F. WHELAN COMPANY 038 A & A, LTD. 040 MKC CUSTOMS BROKERS INTL INC 041 DIVISION M INC 042 ALL SERVICE IMPORT CO INC 043 THOMAS A BURCET CB 044 WAYNE M WITHROW & CO 045 SCHMIDT PRITCHARD & CO INC 046 JAGRO AIR SERVICES 048 FEDEX CUSTOMS BROKERAGE CORP 051 INTERNATIONAL SPECIALISTS, INC. 056 LESCHACO, INC. 059 JOSEPH G MAZZARISE CB INC 062 TOTAL LOGISTICS RESOURCE INC 063 C & R CUSTOMS BROKERS INC 064 KEVIN M DIRAN 065 OCEANLAND SERVICE INC 066 D HAUSER, INC. 068 DAVID L QUIGLEY 069 SIMMONS BROKERAGE SERVICE 070 ELCO SHIPPING CORP FILER-CODE FILER-NAME 071 WILLIAM B SKINNER, INC. 073 AMANA EXPRESS INTERNATIONAL INC. 074 NATHAN WEIN 075 TRANSMARINE SYSTEMS INC 077 TRANSWORLD SHIPPING CORP 081 VIMAR 082 WILLIAMS CLARKE CO., INC. -

Are Heavy Metal Music Bands/Musicians Managers of Their Own Music Business?
UNIVERSIDADE DA BEIRA INTERIOR Ciências Sociais e Humanas Are Heavy Metal Music Bands/Musicians Managers of their own Music Business? A Multiple Case Study: Portuguese vs. Finnish bands Lídia Baltazar Dissertação para obtenção do grau de mestre em Gestão (2º ciclo de estudos) Orientadora: Prof. Doutora Anabela Dinis Covilhã, Outubro 2013 Are Heavy Metal Music Bands/Musicians Managers of their own Music Business? ii Are Heavy Metal Music Bands/Musicians Managers of their own Music Business? Dedication To all the “start-up” bands and/or musicians out there, especially underground/unsigned Heavy Metal bands, who face many challenges in making their music heard: Do not give up! There are many ways to win in the Music Industry and it all starts with You! Stay loyal to your dreams, your music and Rock On! iii Are Heavy Metal Music Bands/Musicians Managers of their own Music Business? iv Are Heavy Metal Music Bands/Musicians Managers of their own Music Business? Acknowledgments Cordially, I would like to thank Professor Anabela Dinis for accepting my research proposal, providing me with the opportunity to learn and grow, both academically and personally. It was an enduring and time-consuming process but it was worth it! I am especially grateful to all the people I had the pleasure to meet throughout my research and data collection, in particular, to Toni-Matti Karjalainen for his availability, friendly reception, enthusiasm, support and valuable help in getting the right contacts. Thank you very much! Without your help this would be a lot harder to accomplish! I would also like to express my sincere gratitude to the guys that accepted making part of this study with their bands and spared some of their precious time to meet and talk with me. -

MINAT TERHADAP MUSIK KOREA DI KALANGAN REMAJA DI YOGYAKARTA (Studi Pada Penggemar K-Pop Di Daerah Sleman)
MINAT TERHADAP MUSIK KOREA DI KALANGAN REMAJA DI YOGYAKARTA (Studi pada Penggemar K-Pop di Daerah Sleman) SKRIPSI Diajukan Kepada Fakultas Ekonomi Universitas Negeri Yogyakarta untuk memenuhi Sebagian Persyaratan Guna Memperoleh Gelar Sarjana Ekonomi Disusun Oleh: ANISA NUR ANDINA 08408144033 PROGRAM STUDI MANAJEMEN - JURUSAN MANAJEMEN FAKULTAS EKONOMI UNIVERSITAS NEGERI YOGYAKARTA 2013 LEMBAR PERSETUJUAN SKRIPSI MINAT TERHADAP MUSIK KOREA DI KALANGAN REMAJA DI YOGYAKARTA (Studi pada Penggemar K-Pop di Daerah Sleman) Disusun Oleh : Anisa Nur Andina NIM. 08408144033 Telah disetujui oleh Dosen Pembimbing untuk diajukan dan dipertahankan di depan Tim Penguji Tugas Akhir Skripsi Jurusan Manajemen, Fakultas Ekonomi, Universitas Negeri Yogyakarta. Yogyakarta, 28 Mei 2013 Menyetujui, Pembimbing Dyna Herlina Suwarto, M.Sc NIP. 19810421 200501 2 001 ii lit PERI\IYATAAN Nama Anisa Nur Andina NIM 08408144033 Prodi/Jurusan Manajernen Fakultas Falarltas Ekonomi Judul Penelitian :Minat Terhadap Musik Korea di Kalangan Remaja di Yogyakarta (Studi pada Penggemar K-Pop di Daerah Sleman). rrya saya sendiri dan sepanjang pengetahuan saya, tidak berisi materi yang dipublikasikan atau ditulis oleh orang lain \ atau telah digunakan sebagai persymatan penyelesaian studi di perguruan tinggi lain, . kecuali pada bagian tertentu yang saya ambil sebagai acuan atau kutipan dengan I mengikuti tata penulisan karya ilmiatr yang telah lazim. i Yogyakarta, 28 Mei 2013 Yang menyatakan, AnisaW Nur Andina NrM.08408144033 IV MOTTO “Kemarin hanya akan menjadi kenangan untuk hari ini dan esok adalah impian untuk hari ini, mari lakukan yang terbaik” (Penulis) “Patience is bitter, but it’s fruit is sweet” (Jang Dongwoo - Infinite) “Hai orang-orang beriman, jadikan sabar dan shalatmu sebagai penolongmu, sesungguhnya Allah beserta orang-orang yang sabar” (Al Baqarah: 153) “Pendidikan adalah mempelajari apa yang bahkan kau tak tahu dari apa yang tak kau ketahui” ( Daniel J.