Timing of Induction of Labor: Myths, Facts, and Misunderstandings?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vincent Du Vigneaud
Vincent du Vigneaud May 18, 1901 — December 11, 1978 Vincent du Vigneaud was born in Chicago in 1901. He majored in chemistry at the University of Illinois at Urbana and received the Master of Science degree in 1924. H. B. Lewis and W. C. Rose introduced him to biochemistry, which became his major field of interest. At Urbana he supported himself by working as a waiter and teaching cavalry tactics and equitation as a reserve second lieutenant. He received his Ph.D. degree in 1927 from the University of Rochester for work on the chemistry of insulin. Insulin is a protein containing sulfur, an atom that became his life-long center of interest, as vividly told in his book A Trail of Research (Cornell University Press, 1952). For his postdoctoral work du Vigneaud moved to Baltimore with his wife, Zella, whom he had married in 1924, to work with J. J. Abel at Johns Hopkins. There, in the first steps following the sulfur trail, he worked on cystine, a constituent of insulin which Abel had crystallized in 1925. Du Vigneaud helped to establish that insulin is indeed a protein, an unpopular veiwpoint at the time. After another year of postdoctoral fellowship in Europe, du Vigneaud returned to Urbana as an assistant professor in physiological chemistry (1930-32). He continued his work on cystine and developed an important method for the reduction of the disulfide bond by metallic sodium in liquid ammonia. These reagents remained valuable tools in his hand for his later synthetic work. In 1932, at age 31, he was appointed chairman of biochemistry at George Washington University School of Medicine, where he remained for six years. -

Peptide Chemistry up to Its Present State
Appendix In this Appendix biographical sketches are compiled of many scientists who have made notable contributions to the development of peptide chemistry up to its present state. We have tried to consider names mainly connected with important events during the earlier periods of peptide history, but could not include all authors mentioned in the text of this book. This is particularly true for the more recent decades when the number of peptide chemists and biologists increased to such an extent that their enumeration would have gone beyond the scope of this Appendix. 250 Appendix Plate 8. Emil Abderhalden (1877-1950), Photo Plate 9. S. Akabori Leopoldina, Halle J Plate 10. Ernst Bayer Plate 11. Karel Blaha (1926-1988) Appendix 251 Plate 12. Max Brenner Plate 13. Hans Brockmann (1903-1988) Plate 14. Victor Bruckner (1900- 1980) Plate 15. Pehr V. Edman (1916- 1977) 252 Appendix Plate 16. Lyman C. Craig (1906-1974) Plate 17. Vittorio Erspamer Plate 18. Joseph S. Fruton, Biochemist and Historian Appendix 253 Plate 19. Rolf Geiger (1923-1988) Plate 20. Wolfgang Konig Plate 21. Dorothy Hodgkins Plate. 22. Franz Hofmeister (1850-1922), (Fischer, biograph. Lexikon) 254 Appendix Plate 23. The picture shows the late Professor 1.E. Jorpes (r.j and Professor V. Mutt during their favorite pastime in the archipelago on the Baltic near Stockholm Plate 24. Ephraim Katchalski (Katzir) Plate 25. Abraham Patchornik Appendix 255 Plate 26. P.G. Katsoyannis Plate 27. George W. Kenner (1922-1978) Plate 28. Edger Lederer (1908- 1988) Plate 29. Hennann Leuchs (1879-1945) 256 Appendix Plate 30. Choh Hao Li (1913-1987) Plate 31. -

The Early Years-Across the Bench from Bruce (1963-1966)
The Early Years—Across the Bench From Bruce (1963–1966) The Early Years—Across the Bench From Bruce (1963–1966) Garland R. Marshall1,2 1Department of Biochemistry and Molecular Biophysics, Center for Computational Biology, Washington University, St. Louis, MO 63110 2Department of Biomedical Engineering, Center for Computational Biology, Washington University, St. Louis, MO 63110 Received 14 July 2007; revised 20 September 2007; accepted 5 October 2007 Published online 16 October 2007 in Wiley InterScience (www.interscience.wiley.com). DOI 10.1002/bip.20870 a Nobel Laureate, Chairman of the Department of Biology at ABSTRACT: Caltech and a member of the National Academy of Science, and was still willing to recommend me for graduate studies This personal reflection on the author’s experience as at Rockefeller. Bruce Merrifield’s first graduate student has been I was convinced at the time that I was chosen to study adapted from a talk given at the Merrifield Memorial neurophysiology, having failed miserably to isolate the acetyl- Symposium at the Rockefeller University on November choline receptor from denervated rabbit muscle as an under- graduate at Caltech. The outstanding neurophysiologists at 13, 2006. # 2007 Wiley Periodicals, Inc. Biopolymers Rockefeller including H. Keffer Hartline, Nobel Laureate, (Pept Sci) 90: 190–199, 2008. were more interested, however, in the wiring diagrams of the Keywords: solid phase synthesis; Merrifield; DNA synthe- eye of the horseshoe crab2 than in how a small molecule sis; combinatorial chemistry could trigger the action potential. Thus, my first laboratory experience at Rockefeller was with Prof. Henry Kunkel, a This article was originally published online as an accepted prominent immunologist.3 Prof. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

THE PRACTICE of EPISIOTOMY: a QUALITATIVE DESCRIPTIVE STUDY on PERCEPTIONS of a GROUP of WOMEN Online Brazilian Journal of Nursing, Vol
Online Brazilian Journal of Nursing E-ISSN: 1676-4285 [email protected] Universidade Federal Fluminense Brasil Yi Wey, Chang; Rejane Salim, Natália; Pires de Oliveira Santos Junior, Hudson; Gualda, Dulce Maria Rosa THE PRACTICE OF EPISIOTOMY: A QUALITATIVE DESCRIPTIVE STUDY ON PERCEPTIONS OF A GROUP OF WOMEN Online Brazilian Journal of Nursing, vol. 10, núm. 2, abril-agosto, 2011, pp. 1-11 Universidade Federal Fluminense Rio de Janeiro, Brasil Available in: http://www.redalyc.org/articulo.oa?id=361441674008 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative THE PRACTICE OF EPISIOTOMY: A QUALITATIVE DESCRIPTIVE STUDY ON PERCEPTIONS OF A GROUP OF WOMEN Chang Yi Wey1, Natália Rejane Salim2, Hudson Pires de Oliveira Santos Junior3, Dulce Maria Rosa Gualda4 1. Hospital Universitário, Universidade de São Paulo 2,3,4. Escola de Enfermagem, Universidade de São Paulo ABSTRACT: This study set out to understand the experiences and perceptions of women from the practices of episiotomy during labor. This is a qualitative descriptive approach, performed in a school hospital in São Paulo, which data were collected through interviews with the participation of 35 women, who experienced and not episiotomy in labor. The thematic analysis shows these categories: Depends the size of the baby facilitates the childbirth; Depends each woman; The woman is not open; and Episiotomy is not necessary. The results allowed that there is lack of clarification and knowledge regarding this practice, which makes the role of decision ends up in the professionals’ hands. -

Vincent Du Vigneaud: Following the Sulfur Trail to the Discovery of the Hormones of the Posterior Pituitary Gland at Cornell Medical College
HISTORICAL VIGNETTE J Neurosurg 124:1538–1542, 2016 Vincent du Vigneaud: following the sulfur trail to the discovery of the hormones of the posterior pituitary gland at Cornell Medical College Malte Ottenhausen, MD,1 Imithri Bodhinayake, MD,1 Matei A. Banu, MD,1 Philip E. Stieg, PhD, MD,1 and Theodore H. Schwartz, MD1–3 1Department of Neurosurgery, Sackler Brain and Spine Center; 2Department of Otolaryngology; and 3Department of Neuroscience, Brain and Mind Institute, Weill Medical College of Cornell University, NewYork-Presbyterian Hospital, New York, New York In 1955, Vincent du Vigneaud (1901–1978), the chairman of the Department of Biochemistry at Cornell University Medical College, was awarded the Nobel Prize for Chemistry for his research on insulin and for the first synthesis of the posterior pituitary hormones—oxytocin and vasopressin. His tremendous contribution to organic chemistry, which began as an interest in sulfur-containing compounds, paved the way for a better understanding of the pituitary gland and for the development of diagnostic and therapeutic tools for diseases of the pituitary. His seminal research continues to impact neurologists, endocrinologists, and neurosurgeons, and enables them to treat patients who had no alternatives prior to du Vigneaud’s breakthroughs in peptide structure and synthesis. The ability of neurosurgeons to aggressively operate on parasellar pathology was directly impacted and related to the ability to replace these hormones after surgery. The authors review the life and career of Vincent du Vigneaud, his groundbreaking discoveries, and his legacy of the understanding and treatment of the pituitary gland in health and disease. http://thejns.org/doi/abs/10.3171/2015.5.JNS141952 KEY WORDS history; pituitary; Nobel Prize; Vincent du Vigneaud; chemistry; oxytocin; vasopressin ROUNDBREAKING scientific discoveries have paved tion in Illinois. -

Hospital Maternity Care Report Card, 2018
New Jersey Hospital Maternity Care Report Card, 2018 Revised on 06/16/2020 1 | P a g e HEALTHCARE QUALITY AND INFORMATICS Prepared by: Erin Mayo, DVM, MPH Genevieve Lalanne-Raymond, RN, MPH Mehnaz Mustafa, MPH, MSc Yannai Kranzler, PhD Technical Support Andreea A. Creanga, MD, PhD Debra Bingham, DrPH, RN, FAAN Jennifer Fearon, MPH Marcela Maziarz, MPA Hospital Partners Diana Contreras, MD-Atlantic Health System Lisa Gittens-Williams, MD Obstetrics & Gynecology– University Hospital Thomas Westover, MD, FACOG- Cooper University Health Care Perry L. Robin, MD, MSEd, FACOG- Cooper University Health Care Hewlett Guy, MD, FACOG- Cooper University Health Care Suzanne Spernal, DNP, APN-BC, RNC-OB, CBC- RWJBarnabas Health 2 | P a g e Table of Contents Statute ........................................................................................................................................................... 5 Summary of the Statute ............................................................................................................................. 5 Summary of Findings ................................................................................................................................ 6 Variation in Delivery Outcomes by Hospital .................................................................................... 6 Complication Rates by Race/Ethnicity: ............................................................................................ 6 General Observations ........................................................................................................................ -

AWARDS, HONORS, DISTINGUISHED LECTURESHIPS Prof. Dr. Dieter Seebach
AWARDS, HONORS, DISTINGUISHED LECTURESHIPS Prof. Dr. Dieter Seebach 1964 <> Wolf-Preis for the Ph.D. thesis, Universität Karlsruhe, Germany 1969 <> Dozentenpreis Fonds der Chemischen Industrie, Germany 1969/1970 – Visiting Professorship, University of Wisconsin, Madison, USA 1972 – "DuPont Travel Grantee", USA (lectures at 15 universities and companies) 1974 – Visiting Professorship, California Institute of Technology, Pasadena, USA 1977 – Visiting Professorship, Rand Afrikaans University, Johannesburg, South Africa – "Pacific Coast Lectureship“, USA/Canada (9 lectures at universities and companies along theUSA west coast) 1978 – Visiting Professorship, Polish Academy of Sciences (lectures in Warsaw and Lodz) 1980 – Visiting Professorship, Australian National University, Canberra, Australia – Visiting Professorship, Imperial College, London, U.K. 1981 – Visiting Professorship at the Weizmann Institute of Science, Rehovot, Israel –"Kolthoff Lectureship", University of Minnesota, Minneapolis, USA 1981 – „Carl Ziegler Visiting Professorship“, Max-Planck-Institut für Kohlenforschung, Mülheim a.d.Ruhr, Germany 1982 – "Vorhees Memorial Lectureship", University of Illinois, Urbana-Champaign, USA – "First Atlantic Coast Lectureship", (6 lectures at universities of the South-East of USA) – "Organic Syntheses Lectureship", Princeton University, Princeton, USA 1984 <> FRSC (Fellow of the Royal Society of Chemistry, U.K.) <> Elected member of the Deutsche Akademie der Naturforscher Leopoldina, D-Halle – "Greater Manchester Lectureship", University -
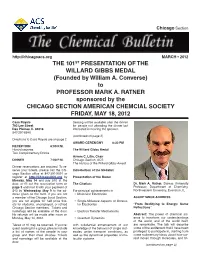
THE 101ST PRESENTATION of the WILLARD GIBBS MEDAL (Founded by William A
Chicago Section http://chicagoacs.org MARCH • 2012 THE 101ST PRESENTATION OF THE WILLARD GIBBS MEDAL (Founded by William A. Converse) to PROFESSOR MARK A. RATNER sponsored by the CHICAGO SECTION AMERICAN CHEMCIAL SOCIETY FRIDAY, MAY 18, 2012 Casa Royale Seating will be available after the dinner 783 Lee Street for people not attending the dinner but Des Plaines, IL 60016 interested in hearing the speaker. 847-297-6640 (continued on page 2) Directions to Casa Royale are on page 2. AWARD CEREMONY 8:30 PM RECEPTION 6:00 P.M. Hors-d’oeuvres The Willard Gibbs Medal Two Complimentary Drinks Avrom C. Litin, Chair DINNER 7:00 P.M. Chicago Section, ACS The History of the Willard Gibbs Award Dinner reservations are required. To re- serve your tickets, please call the Chi- Introduction of the Medalist cago Section office at 847-391-9091 or register at http://ChicagoACS.org by Presentation of the Medal Monday, May 14 and pay $40 at the door, or fill out the reservation form on The Citation: Dr. Mark A. Ratner, Dumas University page 5 and mail it with your payment of Professor, Department of Chemistry, $40 by Wednesday, May 9 to the ad- For principal achievements in Northwestern University, Evanston, IL dress given on the form. If you are not • Molecular Electronics a member of the Chicago Local Section, ACCEPTANCE ADDRESS you are not eligible for half price tick- • Single-Molecule Aspects of Molecu- ets for students, unemployed, or retired lar Electronics “From Rectifying to Energy: Some Chicago Section members. Tickets and Reflections” nametags will be available at the door. -

• Chapter 8 • Nursing Care of Women with Complications During Labor and Birth • Obstetric Procedures • Amnioinfusion –
• Chapter 8 • Nursing Care of Women with Complications During Labor and Birth • Obstetric Procedures • Amnioinfusion – Oligohydramnios – Umbilical cord compression – Reduction of recurrent variable decelerations – Dilution of meconium-stained amniotic fluid – Replaces the “cushion ” for the umbilical cord and relieves the variable decelerations • Obstetric Procedures (cont.) • Amniotomy – The artificial rupture of membranes – Done to stimulate or enhance contractions – Commits the woman to delivery – Stimulates prostaglandin secretion – Complications • Prolapse of the umbilical cord • Infection • Abruptio placentae • Obstetric Procedures (cont.) • Observe for complications post-amniotomy – Fetal heart rate outside normal range (110-160 beats/min) suggests umbilical cord prolapse – Observe color, odor, amount, and character of amniotic fluid – Woman ’s temperature 38 ° C (100.4 ° F) or higher is suggestive of infection – Green fluid may indicate that the fetus has passed a meconium stool • Nursing Tip • Observe for wet underpads and linens after the membranes rupture. Change them as often as needed to keep the woman relatively dry and to reduce the risk for infection or skin breakdown. • Induction or Augmentation of Labor • Induction is the initiation of labor before it begins naturally • Augmentation is the stimulation of contractions after they have begun naturally • Indications for Labor Induction • Gestational hypertension • Ruptured membranes without spontaneous onset of labor • Infection within the uterus • Medical problems in the -

Bain Birthing Center Statistics
THE BAIN BIRTHING CENTER Our 2019 Statistics We are pleased to make available to you the following information about Mount Auburn Hospital's obstetrics program. We hope you will find this fact sheet interesting and informative, and we strongly encourage you to discuss any questions you might have with your health care provider or childbirth educator. MOUNT AUBURN HOSPITAL Mount Auburn Hospital is a Harvard Medical School community teaching hospital. Our goal is to provide personal, individualized care in a setting of clinical excellence. There are 22 obstetricians and 26 midwives on the staff. Last year, midwives attended 39% of the births at Mount Auburn Hospital. Labor/Delivery/Recovery Rooms (LDR's) The Bain Birthing Center at Mount Auburn Hospital welcomed 2481 birth parents and 2513 babies in 2019 (32 sets of twins!). All labor rooms are private Labor/Delivery/Recovery rooms (LDRs) with their own bathrooms and showers. Two of the rooms also have Jacuzzis. The Bain Birthing Center has expanded to include eight LDR rooms (one with a free standing birthing tub), a dedicated triage and evaluation area, and a four bed antepartum observation unit. Following the birth, families are transferred to a room in the maternity suite for their postpartum stay. Most parents and babies room-in together. There is a Level IIa Nursery for those babies who need special care. CESAREAN BIRTHS Although there are some babies who must be delivered by cesarean birth, we are strongly committed to keeping our rates as low as safely possible. The most common reasons for cesarean sections include fetal intolerance of labor (when the baby is dangerously stressed by uterine contractions), cephalopelvic disproportion or CPD (when the baby's head is larger than the mother's pelvis) and breech presentation (when the baby's buttocks are coming first instead of the head). -

517052* Phone: 612-273-2223 Fax: 612-273-2224 � Maternal-Fetal Medicine Center, Burnsville Patient Name: ______Ridgeview Medical Building, 303 E
M HEALTH MATERNAL-FETAL MEDICINE CENTERS MFM Provider Service Request OUTpatient Maternal-Fetal Medicine Center, Minneapolis University of Minnesota Medical Center, Riverside Professional Building 606 24th Ave. S., Suite 400, Minneapolis, MN 55454 *517052* Phone: 612-273-2223 Fax: 612-273-2224 Maternal-Fetal Medicine Center, Burnsville Patient Name: _______________________________________________ Ridgeview Medical Building, 303 E. Nicollet Blvd., Patient Address: _____________________________________________ Suite 363 Burnsville, MN 55337 Phone: 952-892-2270 Fax: 952-892-2275 DOB: ______/________/_________(mm/dd/yyyy) Maternal-Fetal Medicine Center, Edina Home Phone #: ( ) – Southdale Medical Building, 6545 France Ave., Work Phone #: ( ) – Suite 250 Edina, MN 55435 Cell Phone #: ( ) – Phone: 952-924-5250 Fax: 952-924-5251 Interpreter: Y / N Language: ___________________________________ Priority: High (will be scheduled within 72 hrs) First Available/Patient Convenience (If priority not selected will assume first available) Date: Prenatal Provider Name: Clinic Contact Person: Referring Clinic/Site: Clinic Phone #: ( ) – Clinic Fax #: ( ) – EDD:_____________ LMP:______________ Please Circle: SINGLE TWIN TRIPLET QUAD MORE _________ ULTRASOUND (US) - Reason for Ultrasound (Indication/Diagnosis): _______________________________________ *Patients will receive ultrasound interpretation only by the Maternal Fetal Medicine Specialist. First Trimester Ultrasound (less than 14 weeks gestation) First Trimester Screening (11to13weeks6daysgestation)*Patient