**No Patient Handout Palmoplantar Keratoderma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Idiopathic Spiny Keratoderma: a Report of Two Cases and Literature Review
Idiopathic Spiny Keratoderma: A Report of Two Cases and Literature Review Jessica Schweitzer, DO,* Matthew Koehler, DO,** David Horowitz, DO*** *Intern, Largo Medical Center, Largo, FL **Dermatology Resident, Third Year, College Medical Center/Western University, Long Beach, CA ***Dermatology Residency Program Director, College Medical Center/Western University, Long Beach, CA Abstract Spiny keratoderma is a rare and likely underreported condition that presents with punctate hyperkeratotic growths localized to the palms and soles. We present two cases of clinically diagnosed spiny keratoderma. Although the lesions were asymptomatic, patients are at risk of an underlying internal malignancy with this condition, so diagnosis is crucial. Neither men were seeking treatment for the lesions when they were discovered, suggesting that this condition may be much more common than reported. Patients with histories of manual labor, increased UV exposure, and non-melanoma skin cancer (NMSC) may also be at higher risk for developing spiny keratoderma.1 The epidemiology, histopathologic features, differential diagnosis, and current treatments for spiny keratoderma are reviewed. Introduction Case 2 enthusiast for his entire life, spending significant Spiny keratoderma is a rare palmoplantar A 67-year-old Caucasian male presented with a time using his hands to maintain and fire his keratoderma that presents with keratotic, pinpoint one-year history of insidiously growing, pinpoint weapons and many hours outside without sun papules on the palms and soles. There are both hyperkeratotic papules projecting from his palms protection. The patient was referred back to his hereditary and acquired forms. When found, bilaterally (Figures 4-5). He presented to the clinic primary care physician for internal evaluation. -

Bilateral Lower Extremity Hyperkeratotic Plaques: a Case Report of Ichthyosis Vulgaris
Faculty & Staff Scholarship 2015 Bilateral lower extremity hyperkeratotic plaques: a case report of ichthyosis vulgaris Hayley Leight Zachary Zinn Omid Jalali Follow this and additional works at: https://researchrepository.wvu.edu/faculty_publications Clinical, Cosmetic and Investigational Dermatology Dovepress open access to scientific and medical research Open Access Full Text Article CASE REPORT Bilateral lower extremity hyperkeratotic plaques: a case report of ichthyosis vulgaris Hayley Leight Abstract: Here, we report a case of a middle-aged woman presenting with severe, long-standing, Zachary Zinn hyperkeratotic plaques of the lower extremities unrelieved by over-the-counter medications. Omid Jalali Initial history and clinical findings were suggestive of an inherited ichthyosis. Ichthyoses are genetic disorders characterized by dry scaly skin and altered skin-barrier function. A diagnosis Department of Dermatology, West Virginia University, of ichthyosis vulgaris was confirmed by histopathology. Etiology, prevalence, and treatment Morgantown, WV, USA options are discussed. Keywords: filaggrin gene, FLG, profilaggrin, keratohyalin granules, hyperkeratosis Introduction For personal use only. Inherited ichthyoses are a diverse group of genetic disorders characterized by dry, scaly skin; hyperkeratosis; and altered skin-barrier function. While these disorders of cutaneous keratinization are multifaceted and varying in etiology, disruption in the stratum corneum with generalized scaling is common to all.1–4 Although not entirely known -
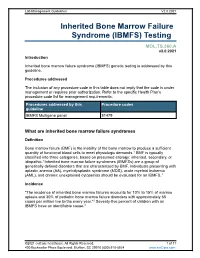
Inherited Bone Marrow Failure Syndrome (IBMFS) Testing
Lab Management Guidelines V2.0.2021 Inherited Bone Marrow Failure Syndrome (IBMFS) Testing MOL.TS.360.A v2.0.2021 Introduction Inherited bone marrow failure syndrome (IBMFS) genetic testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline IBMFS Multigene panel 81479 What are inherited bone marrow failure syndromes Definition Bone marrow failure (BMF) is the inability of the bone marrow to produce a sufficient quantity of functional blood cells to meet physiologic demands.1 BMF is typically classified into three categories, based on presumed etiology: inherited, secondary, or idiopathic.1 Inherited bone marrow failure syndromes (IBMFSs) are a group of genetically defined disorders that are characterized by BMF. Individuals presenting with aplastic anemia (AA), myelodysplastic syndrome (MDS), acute myeloid leukemia (AML), and chronic unexplained cytopenias should be evaluated for an IBMFS.1 Incidence "The incidence of inherited bone marrow failures accounts for 10% to 15% of marrow aplasia and 30% of pediatric bone marrow failure disorders with approximately 65 cases per million live births every year."2 Seventy-five percent of children with an IBMFS have an identifiable cause.2 ©2021 eviCore healthcare. All Rights Reserved. 1 of 17 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V2.0.2021 Symptoms While specific features may vary by each type of IBMFS, features that are present in most IBMFSs include bone marrow failure with single or multi-lineage cytopenia. -

Open Full Page
CCR PEDIATRIC ONCOLOGY SERIES CCR Pediatric Oncology Series Recommendations for Childhood Cancer Screening and Surveillance in DNA Repair Disorders Michael F. Walsh1, Vivian Y. Chang2, Wendy K. Kohlmann3, Hamish S. Scott4, Christopher Cunniff5, Franck Bourdeaut6, Jan J. Molenaar7, Christopher C. Porter8, John T. Sandlund9, Sharon E. Plon10, Lisa L. Wang10, and Sharon A. Savage11 Abstract DNA repair syndromes are heterogeneous disorders caused by around the world to discuss and develop cancer surveillance pathogenic variants in genes encoding proteins key in DNA guidelines for children with cancer-prone disorders. Herein, replication and/or the cellular response to DNA damage. The we focus on the more common of the rare DNA repair dis- majority of these syndromes are inherited in an autosomal- orders: ataxia telangiectasia, Bloom syndrome, Fanconi ane- recessive manner, but autosomal-dominant and X-linked reces- mia, dyskeratosis congenita, Nijmegen breakage syndrome, sive disorders also exist. The clinical features of patients with DNA Rothmund–Thomson syndrome, and Xeroderma pigmento- repair syndromes are highly varied and dependent on the under- sum. Dedicated syndrome registries and a combination of lying genetic cause. Notably, all patients have elevated risks of basic science and clinical research have led to important in- syndrome-associated cancers, and many of these cancers present sights into the underlying biology of these disorders. Given the in childhood. Although it is clear that the risk of cancer is rarity of these disorders, it is recommended that centralized increased, there are limited data defining the true incidence of centers of excellence be involved directly or through consulta- cancer and almost no evidence-based approaches to cancer tion in caring for patients with heritable DNA repair syn- surveillance in patients with DNA repair disorders. -

Palmoplantar Keratoderma with Progressive Gingivitis and Recurrent Pyodermas
Palmoplantar Keratoderma With Progressive Gingivitis and Recurrent Pyodermas Tyler A. Moss, DO; Anne P. Spillane, MD; Sam F. Almquist, MD; Patrick E. McCleskey, MD; Oliver J. Wisco, DO Practice Points Papillon-Lefèvre syndrome (PLS) is an autosomal-recessive inherited transgredient palmoplantar kerato- derma (PPK) that is associated with gingivitis and recurrent pyodermas. The symptoms associated with PLS are thought to be due to cathepsin C gene, CTSC, mutations. CTSC is expressed in epithelial regions commonly affected by PLS and also plays a role in the activation of immune and inflammatory responses. Papillon-Lefèvre syndrome must be differentiated from other conditions causing PPK, such as Haim-Munk syndrome, Greither syndrome, mal de Meleda, Clouston syndrome, Vohwinkel syndrome, and Olmsted syndrome. Treatment of PLS includesCUTIS keratolytics such as urea and/or salicylic acid comb ined with oral retinoids. Active gingivitis may be treated with combined use of amoxicillin and metronidazole. Papillon-Lefèvre syndrome (PLS) is a rare inher- Case Report ited palmoplantar keratoderma (PPK) that is asso- A 30-year-old woman presented to the dermatology ciated with progressive gingivitis and recurrent clinic with erythematous hyperkeratotic plaques on pyodermas.Do We present a caseNot exhibiting classic the palmsCopy and soles. The plaques extended onto features of this autosomal-recessive condition the dorsal aspects of the fingers, toes, hands, and and review the current understanding of its patho- feet (Figures 1 and 2). The patient had psoriasiform physiology, diagnosis, and treatment. Addition- plaques on the extensor surfaces of the knees and ally, a review of pertinent transgredient PPKs is elbows (Figure 3) along with a history of slow- undertaken, with key and distinguishing features progressing gingivitis and periodontal disease that of each syndrome highlighted. -

Pediatric and Adolescent Dermatology
Pediatric and adolescent dermatology Management and referral guidelines ICD-10 guide • Acne: L70.0 acne vulgaris; L70.1 acne conglobata; • Molluscum contagiosum: B08.1 L70.4 infantile acne; L70.5 acne excoriae; L70.8 • Nevi (moles): Start with D22 and rest depends other acne; or L70.9 acne unspecified on site • Alopecia areata: L63 alopecia; L63.0 alopecia • Onychomycosis (nail fungus): B35.1 (capitis) totalis; L63.1 alopecia universalis; L63.8 other alopecia areata; or L63.9 alopecia areata • Psoriasis: L40.0 plaque; L40.1 generalized unspecified pustular psoriasis; L40.3 palmoplantar pustulosis; L40.4 guttate; L40.54 psoriatic juvenile • Atopic dermatitis (eczema): L20.82 flexural; arthropathy; L40.8 other psoriasis; or L40.9 L20.83 infantile; L20.89 other atopic dermatitis; or psoriasis unspecified L20.9 atopic dermatitis unspecified • Scabies: B86 • Hemangioma of infancy: D18 hemangioma and lymphangioma any site; D18.0 hemangioma; • Seborrheic dermatitis: L21.0 capitis; L21.1 infantile; D18.00 hemangioma unspecified site; D18.01 L21.8 other seborrheic dermatitis; or L21.9 hemangioma of skin and subcutaneous tissue; seborrheic dermatitis unspecified D18.02 hemangioma of intracranial structures; • Tinea capitis: B35.0 D18.03 hemangioma of intraabdominal structures; or D18.09 hemangioma of other sites • Tinea versicolor: B36.0 • Hyperhidrosis: R61 generalized hyperhidrosis; • Vitiligo: L80 L74.5 focal hyperhidrosis; L74.51 primary focal • Warts: B07.0 verruca plantaris; B07.8 verruca hyperhidrosis, rest depends on site; L74.52 vulgaris (common warts); B07.9 viral wart secondary focal hyperhidrosis unspecified; or A63.0 anogenital warts • Keratosis pilaris: L85.8 other specified epidermal thickening 1 Acne Treatment basics • Tretinoin 0.025% or 0.05% cream • Education: Medications often take weeks to work AND and the patient’s skin may get “worse” (dry and red) • Clindamycin-benzoyl peroxide 1%-5% gel in the before it gets better. -

Revertant Mosaicism in a Human Skin Fragility Disorder Results from Slipped Mispairing and Mitotic Recombination
Revertant mosaicism in a human skin fragility disorder results from slipped mispairing and mitotic recombination Dimitra Kiritsi, … , Leena Bruckner-Tuderman, Cristina Has J Clin Invest. 2012;122(5):1742-1746. https://doi.org/10.1172/JCI61976. Brief Report Dermatology Spontaneous gene repair, also called revertant mosaicism, has been documented in several genetic disorders involving organs that undergo self-regeneration, including the skin. Genetic reversion may occur through different mechanisms, and in a single individual, the mutation can be repaired in various ways. Here we describe a disseminated pattern of revertant mosaicism observed in 6 patients with Kindler syndrome (KS), a genodermatosis caused by loss of kindlin-1 (encoded by FERMT1) and clinically characterized by patchy skin pigmentation and atrophy. All patients presented duplication mutations (c.456dupA and c.676dupC) in FERMT1, and slipped mispairing in direct nucleotide repeats was identified as the reversion mechanism in all investigated revertant skin spots. The sequence around the mutations demonstrated high propensity to mutations, favoring both microinsertions and microdeletions. Additionally, in some revertant patches, mitotic recombination generated areas with homozygous normal keratinocytes. Restoration of kindlin-1 expression led to clinically and structurally normal skin. Since loss of kindlin-1 severely impairs keratinocyte proliferation, we predict that revertant cells have a selective advantage that allows their clonal expansion and, consequently, the improvement of the skin condition. Find the latest version: https://jci.me/61976/pdf Brief report Revertant mosaicism in a human skin fragility disorder results from slipped mispairing and mitotic recombination Dimitra Kiritsi,1 Yinghong He,1 Anna M.G. Pasmooij,2 Meltem Onder,3 Rudolf Happle,1 Marcel F. -

Arsenicosis Presenting with Cutaneous Squamous Cell Carcinoma: a Case Report
CASE REPORT Arsenicosis Presenting with Cutaneous Squamous Cell Carcinoma: A Case Report Marie Len A. Camaclang,1 Eileen Liesl A. Cubillan2 and Claudine Yap-Silva2 1Section of Dermatology, Department of Medicine, Philippine General Hospital, University of the Philippines Manila 2Section of Dermatology, Department of Medicine, College of Medicine and Philippine General Hospital, University of the Philippines Manila ABSTRACT A 29-year-old male with eleven-year history of hyperkeratotic papules and speckled pigmentation developed cutaneous squamous cell carcinoma. Arsenicosis was confirmed by elevated hair arsenic level, and histopathologic findings of arsenical keratosis and one lesion showing carcinoma-in-situ. Chronic arsenic exposure has been found to activate inflammatory and carcinogenic pathways leading to development of pre-malignant and malignant lesions. A multi-disciplinary approach involving healthcare specialists and environmentalists is crucial in source control and management of long-term complications. Key Words: arsenic, arsenic poisoning, arsenicosis, skin cancer, squamous cell carcinoma INTRODUCTION Arsenic is a potential human carcinogen of public health concern. Exposure may be via inhalation of arsenic dusts, direct contact with arsenites, or ingestion of contaminated water, the latter being the most common route.1 Chemical contamination of groundwater may come from natural sources such as geochemical processes (e.g. volcanic activities), as well as the result of human activities including mining wastes, landfills, -

EXTENDED CARRIER SCREENING Peace of Mind for Planned Pregnancies
Focusing on Personalised Medicine EXTENDED CARRIER SCREENING Peace of Mind for Planned Pregnancies Extended carrier screening is an important tool for prospective parents to help them determine their risk of having a child affected with a heritable disease. In many cases, parents aren’t aware they are carriers and have no family history due to the rarity of some diseases in the general population. What is covered by the screening? Genomics For Life offers a comprehensive Extended Carrier Screening test, providing prospective parents with the information they require when planning their pregnancy. Extended Carrier Screening has been shown to detect carriers who would not have been considered candidates for traditional risk- based screening. With a simple mouth swab collection, we are able to test for over 419 genes associated with inherited diseases, including Fragile X Syndrome, Cystic Fibrosis and Spinal Muscular Atrophy. The assay has been developed in conjunction with clinical molecular geneticists, and includes genes listed in the NIH Genetic Test Registry. For a list of genes and disorders covered, please see the reverse of this brochure. If your gene of interest is not covered on our Extended Carrier Screening panel, please contact our friendly team to assist you in finding a gene test panel that suits your needs. Why have Extended Carrier Screening? Extended Carrier Screening prior to pregnancy enables couples to learn about their reproductive risk and consider a complete range of reproductive options, including whether or not to become pregnant, whether to use advanced reproductive technologies, such as preimplantation genetic diagnosis, or to use donor gametes. -

Download PDF (Inglês)
Revista6Vol89ingles_Layout 1 10/10/14 11:08 AM Página 1003 WHAT IS YOUR DIAGNOSIS? 1003 s Case for diagnosis* João Roberto Antonio1 Larissa Cannizza Pacheco de Lucca1 Mariana Perez Borim1 Natália Cristina Pires Rossi1 Guilherme Bueno de Oliveira1 DOI: http://dx.doi.org/10.1590/abd1806-4841.20143156 CASE REPORT A 60-year-old woman reports a 5-year history of violaceous and intensely pruritic lesions on the dorsum and scalp, associated with a 2-year history of hair loss. She also reports decreased hair growth in the axillary and inguinal regions in the same period. Dermatological examination shows small, scaly, erythematous-violaceous, flat papules on the dorsal region; multifocal scarring alopecia areas, with smooth, bright and atrophic surface; discrete hair rarefaction in the axillary and inguinal regions; presence of longitu- FIGURE 2: dinal grooves and some depressions on the surface of Perifollicular the nail plate; no oral lesions (Figures 1 and 2). The erythema with desquamation at histopathology of the dorsal lesion is shown in figure the vertex of the 3A and that of the scalp is shown in figure 3B. scalp; cicatricial The treatment was performed using high- alopecia and potency corticoids and resulted, after three months, in smooth, bright and atrophic surface an improvement of pruritus and a slight lightening of the lesions. A FIGURE 1: B Cutaneous, erythematous- FIGURE 3: A. HE 200x. Interface dermatitis with lichenoid pattern purpuric lesions associated with dermo-epidermic detachment and lymphocytic on the infiltrate in band-like pattern in the upper dermis. B. HE 200x. dorsal region Detail of partially destroyed follicle, with perifollicular fibrosis and perivascular lymphocytic infiltrate Received on 19.09.2013. -

Harlequin Ichthyosis
orphananesthesia Anaesthesia recommendations for patients suffering from Harlequin ichthyosis Disease name: Harlequin ichthyosis ICD 10: Q80.4 Synonyms: Harlequin baby, ichthyosis congenita, Ichthyosis fetalis, keratosis diffusa fetalis, Harlequin fetus, Ichthyosis congenita gravior Disease summary: Harlequin ichthyosis (HI) is an autosomal recessive congenital ichthyosis. HI is an extremely rare and most severe form of ichthyosis. The condition is caused by mutation of the ABCA12 gene resulting in impaired lipid transport in the outermost layer of the skin, the epidermis. During the neontatal period, harlequin ichthyosis manifests phenotypically as dramatic large polygonal plate-like scaling of the skin that cracks and can slough, revealing the underlying diffusely bright red skin. These thick skin plates can pull and distort facial features. The tightness of the skin can also pull on the eyes and mouth resulting in difficulties with closing these structures. The tightness also causes the eyes and the mouth to turn inside out resulting in ectropion and eclabium. Other features include hypoplasia of the fingers, malformation of the ears and nose, and alopecia. Affected neonates often do not survive and mortality is commonly attributed to respiratory failure and/or sepsis. Clinical data obtained from 45 HI patients revealed 25 survivors and 20 deaths with an overall survival rate of only 56%. The ages of survivors ranged from 10 months to 25 years and death usually occurred in the first 3 months. HI infants need to be cared for in a neonatal intensive care unit immediately after birth. Several harlequin neonates have survived. They tend to have severe erythroderma and fine scaling, even with optimal management. -

Erythrokeratodermia Variabilis Et Progressiva Allelic to Oculo-Dento
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector COMMENTARY See related article on pg 1540 translocated into the plasma membrane. Once expressed on the cell surface, the hemichannel docks with a connexon of an adjacent cell to form a channel that Erythrokeratodermia Variabilis et is termed gap junction. Connexons can form either homotypic (docking of two Progressiva Allelic to Oculo-Dento- identical connexons), heterotypic (docking of two dissimilar homomeric Digital Dysplasia connexons), or heteromeric (docking of two heteromeric connexons) channels Sabine Duchatelet1,2 and Alain Hovnanian1,2,3 (Mese et al., 2007). These diverse Erythrokeratodermia variabilis et progressiva (EKVP) is a genodermatosis with combinations of connexins create clinical and genetic heterogeneity, most often transmitted in an autosomal different types of channels, each having dominant manner, caused by mutations in GJB3 and GJB4 genes encoding unique properties (ionic conductance, connexins (Cx)31 and 30.3, respectively. In this issue, Boyden et al. (2015) report permeability, sensitivity to voltage, or for the first time de novo dominant mutations in GJA1 encoding the ubiquitous pH). Of note, several connexins may also Cx43 in patients with EKVP. These results expand the genetic heterogeneity of form functional nonjunctional hemi- EKVP and the human disease phenotypes associated with GJA1 mutations. They channels, although their physiological disclose that EKVP is allelic to oculo-dento-digital dysplasia, a rare syndrome relevance remains uncertain (Pfenniger previously known to be caused by dominant GJA1 mutations. et al., 2010). Mutations in 11 connexin genes cause a variety of genetic dis- Journal of Investigative Dermatology (2015) 135, 1475–1478.