Bilateral Lower Extremity Hyperkeratotic Plaques: a Case Report of Ichthyosis Vulgaris
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Skin Brief Articles
SKIN BRIEF ARTICLES Nab-paclitaxel/gemcitabine Induced Acquired Ichthyosis Adriana Lopez BAa, Joel Shugar MDb, and Mark Lebwohl MDc aColumbia University Vagelos College of Physicians and Surgeons, New York, NY bIcahn School of Medicine at Mount Sinai, Department of Otolaryngology, New York, NY cIcahn School of Medicine at Mount Sinai, Department of Dermatology, New York, NY ABSTRACT The ichthyoses are a diverse group of cutaneous disorders characterized by abnormalities in cornification. The majority of ichthyoses are inherited with childhood presentation and new onset ichthyosis in adulthood warrants further medical evaluation. Though most well recognized for its association with Hodgkin’s disease, acquired ichthyosis (AI) has been linked to a number of inflammatory, autoimmune, and endocrine processes. However, drug- induced AI is exceedingly rare and remains a poorly understood entity. Here we report a case of a male patient who developed AI while receiving nab-paclitaxel plus gemcitabine for treatment of pancreatic adenocarcinoma. months prior, the patient was first seen for INTRODUCTION recurrent, self-healing, pruritic erythematous Acquired ichythyosis (AI) is an uncommon papules. Punch biopsy was performed which non-inherited cutaneous disorder of showed an atypical cellular infiltrate of abnormal keratinization that is most scattered large CD30+ cells with clonal T-cell frequently associated with underlying receptor-β gene rearrangement. Though the malignancy. Drug induced AI is uncommon clinicopathologic diagnosis was most and has been rarely linked to consistent with lymphomatoid papulosis chemotherapeutic agents. Herein, we report (LyP), imaging was pursued to exclude the case of a man with pancreatic extracutaneous lymphoproliferative disease. adenocarcinoma who developed an CT scan incidentally detected a mass in the ichthyosiform eruption upon starting body of the pancreas and biopsy was chemotherapy with nab-paclitaxel plus concordant with pancreatic adenocarcinoma. -

Lymphatic Complaints in the Dermatology Clinic: an Osteopathic
Volume 35 JAOCDJournal Of The American Osteopathic College Of Dermatology Lymphatic Complaints in the Dermatology Clinic: An Osteopathic Approach to Management A five-minute treatment module makes lymphatic OMT a practical option in busy practices. Also in this issue: A Case of Acquired Port-Wine Stain (Fegeler Syndrome) Non-Pharmacologic Interventions in the Prevention of Pediatric Atopic Dermatitis: What the Evidence Says Inflammatory Linear Verrucous Epidermal Nevus Worsening in Pregnancy last modified on June 9, 2016 10:54 AM JOURNAL OF THE AMERICAN OSTEOPATHIC COLLEGE OF DERMATOLOGY Page 1 JOURNAL OF THE AMERICAN OSTEOPATHIC COLLEGE OF DERMATOLOGY 2015-2016 AOCD OFFICERS PRESIDENT Alpesh Desai, DO, FAOCD PRESIDENT-ELECT Karthik Krishnamurthy, DO, FAOCD FIRST VICE-PRESIDENT Daniel Ladd, DO, FAOCD SECOND VICE-PRESIDENT John P. Minni, DO, FAOCD Editor-in-Chief THIRD VICE-PRESIDENT Reagan Anderson, DO, FAOCD Karthik Krishnamurthy, DO SECRETARY-TREASURER Steven Grekin, DO, FAOCD Assistant Editor TRUSTEES Julia Layton, MFA Danica Alexander, DO, FAOCD (2015-2018) Michael Whitworth, DO, FAOCD (2013-2016) Tracy Favreau, DO, FAOCD (2013-2016) David Cleaver, DO, FAOCD (2014-2017) Amy Spizuoco, DO, FAOCD (2014-2017) Peter Saitta, DO, FAOCD (2015-2018) Immediate Past-President Rick Lin, DO, FAOCD EEC Representatives James Bernard, DO, FAOCD Michael Scott, DO, FAOCD Finance Committee Representative Donald Tillman, DO, FAOCD AOBD Representative Michael J. Scott, DO, FAOCD Executive Director Marsha A. Wise, BS AOCD • 2902 N. Baltimore St. • Kirksville, MO 63501 800-449-2623 • FAX: 660-627-2623 • www.aocd.org COPYRIGHT AND PERMISSION: Written permission must be obtained from the Journal of the American Osteopathic College of Dermatology for copying or reprinting text of more than half a page, tables or figures. -

Ichthyosis Hystrix
Case Report Ichthyosis hystrix Surajit Nayak, Basanti Acharjya, Prasenjit Mohanty Department of Skin ABSTRACT and VD, MKCG Medical College and Hospital, The present report describes the condition in a three day old male child with bilateral ,linear, hyperpigmented and Berhampur, Orissa, India hyperkeratotic verrucous plaques and patchy alopecia over scalpe without any nail and skeletal abnormalities. It was suggestive of ichthyosis hystrix type of epidermal nevus,and is being reported in view of the rarity of this condition. Key words: Icthyosis hystrix, epidermal nevus syndrome, etretinate INTRODUCTION most part of the face. Nails were normal. In the lower limbs, in addition to the nevus, there were Ichthyosis hystrix the nomenclature comes unilateral hyperpigmented [Figure 1] macular from the Greek word and condition was first patches encircling right upper thigh and complete described in England in early 18th century. left thigh, sparing a band-like zone. The term ichthyosis hystrix is used to describe several rare skin disorders in the ichthyosis On physical examination, we could not observe family of skin disorders characterized by massive any defects, especially in skeletal or central hyperkeratosis with an appearance like spiny nervous systems. Routine laboratory examination scales. The term has also been employed to including complete blood count, urine analysis, describe localized and linear warty epidermal nevi liver function test and chest X-ray were all within sometimes associated with mental retardation, normal limits. The parents did not permit a biopsy. seizures or skeletal anomalies. Alopecia and hair and nail abnormalities as well as inner ear Based on the above constellation of clinical deafness were also seen in these patients. -
Abstract Book
Abstract Book First World Conference on Ichthyosis August 31 – September 2, 2007 Münster, Germany Organized by Network for Ichthyoses and related keratinization disorders (NIRK) together with Selbsthilfe Ichthyose e.V. and EU-Coordination Action GENESKIN Contacts: H. Traupe, Münster, Email: [email protected] B. Willis, Münster, Email: [email protected] Barbara Kleinow, Email: [email protected] Geske Wehr, Email: [email protected] Location: Lecture Hall Location:Department of Dermatology University Hospital Von Esmarch-Str. 58 48149 Münster Germany Friday, August 31, 2007 page Workshop on clinical diversity and diagnostic standardization D. Metze, Münster Histopathology of ichthyoses: Clues for diagnostic standardization ..................................... 19 I. Hausser, Heidelberg Ultrastructural characterization of lamellar ichthyosis: A tool for diagnostic standardization 13 H. Verst, Münster The data base behind the NIRK register: a secure tool for genotype/phenotype analysis 34 V. Oji, Münster Classification of congenital ichthyosis ................................................................................... 20 M. Raghunath, Singapore Congenital Ichthyosis in South East Asia ............................................................................. 25 Keratinization disorders and keratins I. Hausser, Heidelberg Ultrastructure of keratin disorders: What do they have in common? ................................... 12 M. Arin, Köln Recent advances in keratin disorders ................................................................................. -

Cytoplasmic Plaque Formation in Hemidesmosome Development Is Dependent on Soxf Transcription Factor Function
Cytoplasmic Plaque Formation in Hemidesmosome Development Is Dependent on SoxF Transcription Factor Function Shelly Oommen1, Mathias Francois2, Maiko Kawasaki1, Melanie Murrell2, Katsushige Kawasaki1, Thantrira Porntaveetus1, Sarah Ghafoor1, Neville J. Young2, Yoshimasa Okamatsu3, John McGrath4, Peter Koopman2, Paul T. Sharpe1, Atsushi Ohazama1,3* 1 Craniofacial Development and Stem Cell Biology, and Biomedical Research Centre, Dental Institute, King’s College London, London, United Kingdom, 2 Institute for Molecular Bioscience, The University of Queensland, Brisbane, Australia, 3 Department of Periodontology, Showa University Dental School, Tokyo, Japan, 4 Genetic Skin Disease Group, St John’s Institute of Dermatology, Division of Skin Sciences, King’s College London, London, United Kingdom Abstract Hemidesmosomes are composed of intricate networks of proteins, that are an essential attachment apparatus for the integrity of epithelial tissue. Disruption leads to blistering diseases such as epidermolysis bullosa. Members of the Sox gene family show dynamic and diverse expression patterns during development and mutation analyses in humans and mice provide evidence that they play a remarkable variety of roles in development and human disease. Previous studies have established that the mouse mutant ragged-opossum (Raop) expresses a dominant-negative form of the SOX18 transcription factor that interferes with the function of wild type SOX18 and of the related SOXF-subgroup proteins SOX7 and 217. Here we show that skin and oral mucosa in homozygous Raop mice display extensive detachment of epithelium from the underlying mesenchymal tissue, caused by tearing of epithelial cells just above the plasma membrane due to hemidesmosome disruption. In addition, several hemidesmosome proteins expression were found to be dysregulated in the Raop mice. -

Epidermolytic Hyperkeratosis with Ichthyosis Hystrix Geromanta Baleviciené, MD, Vilnius, Lithuania Robert A
pediatric dermatology Series Editor: Camila K. Janniger, MD, Newark, New Jersey Epidermolytic Hyperkeratosis With Ichthyosis Hystrix Geromanta Baleviciené, MD, Vilnius, Lithuania Robert A. Schwartz, MD, MPH, Newark, New Jersey Epidermolytic hyperkeratosis (EH) is a congenital, autosomal-dominant genodermatosis characterized by blisters.1,2 Shortly after birth, the infant’s skin becomes red and may show bullae. The erythema regresses, but brown verrucous hyperkeratosis persists, particularly accentuated in the flexures. This condition is also known as bullous ichthyosiform erythroderma. The disorder of keratinization has varied clinical manifestations in the extent of cutaneous involve- ment, palmar and plantar hyperkeratosis, and evi- dence of erythroderma. We describe 5 patients, 4 with EH (one of whom had it in localized form and one of whom had an unusual type of ichthyosis hystrix described by Curth and Macklin3-7). Case Reports FIGURE 1. Seven-year-old girl with EH, demonstrating Patient 1—A 7-year-old girl with a cutaneous erup- erythema and verrucous hyperkeratosis (Patient 1). tion since birth characterized by flaccid bullae vary- ing in size. The palms and soles had intense diffuse keratosis from 1 year of age. Her nails, hair, teeth, and mental state were normal. The patient’s mother (Pa- tient 2) had a similar disorder. Skin biopsy specimens showed the changes of EH, with pronounced cellular vacuolation of the middle and upper portions of the malpighian stratum and large, clear, irregular spaces. Cellular boundaries were indistinct. A thickened granular layer was evident with large, irregularly shaped keratohyalin granules. Ultrastructural study showed tonofilament clumping of the malpighian layer and cytolysis. -

Proceedings of the 16Th Annual Meeting of the Society for Pediatric Dermatoiogy
SPECIAL ARTICLE Pediatric Dermatology Vol. 9 No. 1 66-76 Proceedings of the 16th Annual Meeting of the Society for Pediatric Dermatoiogy WiUiamsburg, Virginia June 3a-July 3, 1991 Eleanor £. Sahn, M.D. Medical University of South Carolina Charleston, South Carolina A. Howiand Hartley, M.D. Children's Hospital National Medical Center Washington, D.C. Stephen Gellis, M.D. Children's Hospital Medical Center Boston, Massachusetts James E. Rasmussen, M.D. University of Michigan Medical Center Ann Arbor, Michigan Monday, July 1, 1991 ture by the newspaper account he received, dated December 17, 1799, telling of General George Dr. Alfred T. Lane (Stanford University) orga- Washington's death. We learn the story of General nized the sixteenth annual meeting of the Society Washington's rapid demise, probably from bacterial for Pediatric Dermatology, held in Wiliiamsburg, infection, hastened by the medical treatments of the Virgitiia. The seventh annual Sidney Hurwitz Lec- day, including frequent and copious blood letting. ture was delivered by Dr. Rona M. MacKie (Uni- There was a current saying, "more people died an- versity of Glasgow) on "Melanoma: Risk Factors in nually from lancets than from swords." Dysplastic Nevus Syndrome." President Anne Lucky (Cincinnati, Ohio) welcomed the society MELANOMA: RISK FACTORS AND members to Wiliiamsburg and introduced the first DYSPLASTIC NEVUS SYNDROME speaker. Dr. Rona MacKie first discussed risk factors in mel- anoma, citing several large case control studies car- COLONIAL MEDICINE ried out in western Canada, Scotland, Scandinavia, Dr. Tor A. Shwayder (Henry Ford Hospital) pre- and Germany. The frequency of melanoma has dou- sented a delightful and professional "Character In- bled each decade in Scandinavia, the United King- terpreter Portrayal of Iseiac Shwayder, Medical dom, and Germany. -

Mutation and Expression of Abca12in Keratosis Pilaris and Nevus
MOLECULAR MEDICINE REPORTS 18: 3153-3158, 2018 Mutation and expression of ABCA12 in keratosis pilaris and nevus comedonicus FEN LIU1,2*, YAO YANG1,3*, YAN ZHENG1,3, YAN-HUA LIANG1,3 and KANG ZENG1 1Department of Dermatology, Nanfang Hospital, Southern Medical University, Guangzhou, Guangdong 510515; 2Department of Histology and Embryology, Institute of Neuroscience, School of Basic Medical Sciences, Wenzhou Medical University, Wenzhou, Zhejiang 325035; 3Department of Dermatology, Shenzhen Hospital, Southern Medical University, Shenzhen, Guangdong 518100, P.R. China Received June 22, 2017; Accepted April 17, 2018 DOI: 10.3892/mmr.2018.9342 Abstract. Keratosis pilaris (KP) and nevus comedonicus Introduction (NC) are congenital keratinized dermatoses; however, the exact etiology of these two diseases is unclear. The objective Keratosis pilaris (KP; OMIM #604093), also known as of the present study was to identify the disease-causing genes lichen pilaris, is a benign genodermatosis that is estimated and their association with functional alterations in the devel- to effect ~40% of the population (1). KP is characterized by opment of KP and NC. Peripheral blood samples of one KP the presence of symmetric, asymptomatic and grouped kera- family, two NC families and 100 unrelated healthy controls totic follicular papules with varying degrees of perifollicular were collected. The genomic sequences of 147 genes associ- erythema. KP lesions often involve the proximal and extended ated with 143 genetic skin diseases were initially analyzed parts of extremities, the cheeks and the buttocks (2). Cases from the KP proband using a custom-designed GeneChip. A may be generalized or unilateral (2). Most patients develop KP novel heterozygous missense mutation in the ATP-binding in their childhood, with a peak in incidence during adoles- cassette sub-family A member 12 (ABCA12) gene, designated cence (3). -

April 2011 Preventiongenetics Newsletter
News from PreventionGenetics IN THIS ISSUE Volume 3, Number 1 New Tests Welcome to the April 2011 PreventionGenetics Newsletter. In New Hires this issue, we present new DNA sequencing tests for 40 President's Corner disorders. In addition, we introduce two new geneticists to our staff. In the President's Corner, Dr. Jim Weber discusses recent progress at PreventionGenetics. QUICK LINKS Our Website Requisition Form New Tests at PreventionGenetics Please follow the gene links for the corresponding test description. · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · · Achondrogenesis (SLC26A2) Achondrogenesis Type II-Hypochondrogenesis (COL2A1) Amyotrophic Lateral Sclerosis and Primary Open-Angle Glaucoma (OPTN) Atelosteogenesis (SLC26A2) Camurati-Engelmann Disease (TGFB1) Cartilage-hair Hypoplasia and Related Disorders (RMRP) Chediak-Higashi Syndrome (LYST) Chondrodysplasia Punctata, X-Linked Dominant (EBP) Cleidocranial Dysplasia (RUNX2) Cranioectodermal Dysplasia 1 (IFT122) Diastrophic Dysplasia (SLC26A2) Dilated Cardiomyopathy and Limb-Girdle Muscular Dystrophy Type 2F (SGCD) Dentinogenesis Imperfecta (DSPP) Ellis-van Creveld Syndrome (EVC, EVC2) Emery-Dreifuss Muscular Dystrophy-1 (EMD) Fanconi Anemia (FANCL) Hennekam Lymphangiectasia-Lymphedema (CCBE1) Hereditary Breast Cancer (CHEK2) Hermansky Pudlak Syndrome (HPS1, HPS2/AP3B1, HPS3, HPS4, HPS5, HPS6, HPS7/DTNBP1, HPS8/BLOC1S3) Hirschsprung Disease (RET) Holt-Oram Syndrome (TBX5) Kneist Dysplasia (COL2A1) Lynch Syndrome (PMS2) Menkes Disease and X-Hereditary -

Genodermatoses
GENODERMATOSES Genodermatoses What’s new? Nigel P Burrows C Filaggrin mutations underlie ichthyosis vulgaris and are a risk factor for atopy including eczema, allergic sensitization, asthma, allergic rhinitis and peanut allergy Abstract C A new classification and nomenclature for ichthyoses was Genetic skin diseases encompass a spectrum from the common to the published in 2009, peeling skin syndromes which may be rare. It is important for the clinician to be alert to the possibility that confused for the milder subtypes of epidermolysis bullosa are the patient may be presenting for the first time with one or more features distinct genetic entities of a genetic disease so that appropriate investigation and counselling can C Emerging evidence that pseudoxanthoma elasticum is a meta- take place. Recent discoveries have helped the understanding of many of bolic disorder resulting in calcification of elastic fibres these disorders. A few common and important genodermatoses are high- C Mammalian target of rapamycin (mTOR) inhibitor therapies are lighted in this article. showing promise in tuberous sclerosis complex C Vascular anomalies on the skin may be the presenting feature of Keywords cancer syndromes; collagen; epidermolysis bullosa; filaggrin; inherited syndromes genodermatoses; ichthyosis; keratinization; pseudoxanthoma elasticum; vascular anomalies X-linked recessive ichthyosis In 75% of cases of X-linked recessive ichthyosis (XLRI) (Figure 1), scaling is present in the first week of life and tends to progress into adolescence. In contrast to IV, the flexures may be Genetic skin diseases encompass a spectrum from the common involved. A third of cases are associated with a prolonged labour. (e.g. atopic eczema) to the rare (e.g. -

Ichthyosis Vulgaris a Case Report and Review of Literature Sarah E
CASE REPORT Ichthyosis Vulgaris A Case Report and Review of Literature Sarah E. Mertz, Thea D. Nguyen, Lori A. Spies chthyosis vulgaris (IV) is a hereditary skin condi- removal surgery. By patient report, the lesions had been tion characterized by an accumulation of cells in present since childhood but progressively worsened over the horny layer that manifests as xerotic, plate- the past few years because of a lack of skin care routine. As like scales. It is most prominent on the extensor is typical in IV, there was a history of improvement of surfaces of the extremities, back, abdomen, and symptoms in warmer months of the summer. Comorbidities legs and exhibits palmar hyperlinearity (Takeichi & to the long-standing IV and cognitive disability include IAkiyama, 2016). If not properly treated, this build up hypertension and obesity. There was no personal history of can cause difficulty in patient care and a decrease in the skin cancer, and the patient was not able to provide details of quality of life of those afflicted with this condition. his family history. On physical examination, significant and There are more than 20 types of ichthyosis to include pertinent findings include diffuse symmetric, thick, hyper- epidermolytic ichthyosis, congential reticular ichthyosiform keratotic, light-gray, fish-scaled plaques with fissures prom- erythroderma, and lamellar ichthyosis, with IV being the inent on the dorsal and ventral surfaces of the bilateral upper most common type of hereditary nonsyndromic ichthyosis extremities including arms, forearms, dorsal hands, and and characterized as a reduction of keratohyalin granules posterior neck and fine, scaly, erythematous areas of or a granular layer absence (Takeichi & Akiyama, 2016). -
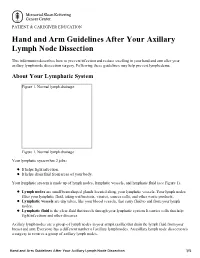
Hand and Arm Guidelines After Your Axillary Lymph Node Dissection
PATIENT & CAREGIVER EDUCATION Hand and Arm Guidelines After Your Axillary Lymph Node Dissection This information describes how to prevent infection and reduce swelling in your hand and arm after your axillary lymph node dissection surgery. Following these guidelines may help prevent lymphedema. About Your Lymphatic System Figure 1. Normal lymph drainage Figure 1. Normal lymph drainage Your lymphatic system has 2 jobs: It helps fight infection. It helps drain fluid from areas of your body. Your lymphatic system is made up of lymph nodes, lymphatic vessels, and lymphatic fluid (see Figure 1). Lymph nodes are small bean-shaped glands located along your lymphatic vessels. Your lymph nodes filter your lymphatic fluid, taking out bacteria, viruses, cancer cells, and other waste products. Lymphatic vessels are tiny tubes, like your blood vessels, that carry fluid to and from your lymph nodes. Lymphatic fluid is the clear fluid that travels through your lymphatic system. It carries cells that help fight infections and other diseases. Axillary lymph nodes are a group of lymph nodes in your armpit (axilla) that drain the lymph fluid from your breast and arm. Everyone has a different number of axillary lymph nodes. An axillary lymph node dissection is a surgery to remove a group of axillary lymph nodes. Hand and Arm Guidelines After Your Axillary Lymph Node Dissection 1/5 About Lymphedema Sometimes, removing lymph nodes can make it hard for your lymphatic system to drain properly. If this happens, lymphatic fluid can build up in the area where the lymph nodes were removed. This extra fluid causes swelling called lymphedema.