Access the What Is Ethics?: Key Distinctions Lesson Plan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Impossibility of Informed Consent?
JME40: Good medical ethics J Med Ethics: first published as 10.1136/medethics-2014-102308 on 16 December 2014. Downloaded from PAPER The impossibility of informed consent? Kenneth Boyd Correspondence to ABSTRACT medical ethics’ over the 40 years of the Journal’s Professor Kenneth Boyd, The problematic nature of informed consent to medical publication. Biomedical Teaching Organisation, Edinburgh treatment and research, and its relation to autonomy, trust and clinical practice, has been addressed on many University, Edinburgh, Scotland Surveying the scene: the law and ethics of EH89AG, UK; occasions and from a variety of ethical perspectives in informed consent to treatment and research [email protected] the pages of the Journal of Medical Ethics. This paper Two early and wide-ranging contributions on medi- gives an account of how discussion of these issues has Received 1 September 2014 colegal and ethical aspects of informed consent developed and changed, by describing a number of Revised 26 September 2014 were made in papers by judge Kirby3 of Australia Accepted 23 October 2014 significant contributions to these debates which provide in 1983 and paediatrician Silverman4 of the USA in examples of ‘doing good medical ethics’ over the 1989. Both agreed that a paternalist or beneficence- 40 years of the Journal’s publication. based approach, in which the doctor recommends a course of treatment to which the patient either con- sents or refuses, had properly been superseded by THE IMPOSSIBILITY OF INFORMED CONSENT? an approach based on respect for the autonomy or Awareness that informed consent is problematic, in right to self-determination of the individual theory and in practice, was already evident in the patient. -

On the Mute, Deaf, and Blind’
Journal of Moral Theology, Vol. 6, Special Issue 2 (2017): 112-137 Seventeenth-Century Casuistry Regarding Persons with Disabilities: Antonino Diana’s Tract ‘On the Mute, Deaf, and Blind’ Julia A. Fleming N 1639, THE FAMOUS THEATINE casuist Antonino Diana published the fifth part of his Resolutiones morales, a volume that included a tract regarding the mute, deaf, and blind.1 Structured I as a series of cases (i.e., questions and answers), its form resembles tracts in Diana’s other volumes concerning members of particular groups, such as vowed religious, slaves, and executors of wills.2 While the arrangement of cases within the tract is not systematic, they tend to fall into two broad categories, the first regarding the status of persons with specified disabilities in the Church and the second in civil society. Diana draws the cases from a wide variety of sources, from Thomas Aquinas and Gratian to later experts in theology, pastoral practice, canon law, and civil law. The tract is thus a reference collection rather than a monograph, although Diana occasionally proposes a new question for his colleagues’ consideration. “On the Mute, Deaf, and Blind” addresses thirty-seven different cases, some focused upon persons with a single disability, and others, on persons with combination of these three disabilities. Specific cases hinge upon further distinctions. Is the individual in question completely or partially blind, totally deaf or hard of hearing, mute or beset with a speech impediment? Was the condition present from birth 1 Antonino Diana, Resolutionum moralium pars quinta (hereafter RM 5) (Lyon, France: Sumpt. -
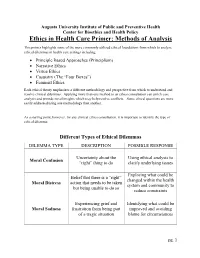
Ethics in Health Care Primer: Methods of Analysis
Augusta University Institute of Public and Preventive Health Center for Bioethics and Health Policy Ethics in Health Care Primer: Methods of Analysis This primer highlights some of the more commonly utilized ethical foundations from which to analyze ethical dilemmas in health care settings including: • Principle Based Approaches (Principlism) • Narrative Ethics • Virtue Ethics • Casuistry (The “Four Boxes”) • Feminist Ethics Each ethical theory emphasizes a different methodology and perspective from which to understand and resolve clinical dilemmas. Applying more than one method to an ethics consultation can enrich case analysis and provide novel insights which may help resolve conflicts. Some ethical questions are more easily addressed using one methodology than another. As a starting point, however, for any clinical ethics consultation, it is important to identify the type of ethical dilemma: Different Types of Ethical Dilemmas DILEMMA TYPE DESCRIPTION POSSIBLE RESPONSE Uncertainty about the Using ethical analysis to Moral Confusion “right” thing to do clarify underlying issues Exploring what could be Belief that there is a “right” changed within the health Moral Distress action that needs to be taken system and community to but being unable to do so reduce constraints Experiencing grief and Identifying what could be Moral Sadness frustration from being part improved and avoiding of a tragic situation blame for circumstances pg. 1 Principlism Principlism refers to a method of analysis utilizing widely accepted norms of moral agency (the ability of an individual to make judgments of right and wrong) to identify ethical concerns and determine acceptable resolutions for clinical dilemmas. In the context of bioethics, principlism describes a method of ethical analysis proposed by Beauchamp and Childress, who believe that there are four principles central in the ethical practice of health care1: 1. -

Whose Life Is It Anyway? a Study in Respect for Autonomy
Journal ofmedical ethics 1995; 21: 179-183 J Med Ethics: first published as 10.1136/jme.21.3.179 on 1 June 1995. Downloaded from Medicine and literature Whose Life Is It Anyway? A study in respect for autonomy Margaret Norden Marymount University, Arlington, Virginia, USA Abstract Precis of the story Brian Clark's drama, Whose Life Is It Anyway? (1), Whose Life Is It Anyway? opens with the explores the difficulties ofapplying the principle of hospitalization of Ken Harrison who was critically respect for autonomy to real-life circumstances. In the injured in an automobile accident four months play a permanently disabled patient, who wishes to be earlier and permanently paralyzed from the neck allowed to die, raises moral questions about the down. Although Ken arrived in critical condition, he adequacy of the autonomous agent, respect for the has since been stabilized, informed by his doctors autonomy ofothers, the authority of the law, the that his paralysis is permanent, and advised that he allocation ofsociety's resources, and the intrinsic value will be transferred to a long-term care facility. Facing ofhuman life. After a brief review of the story and the prospect of such an existence, Ken chooses not definition of respect for autonomy, this paper cites to live. He realizes that he could not survive outside passages from the play that dramatize the tension of an institution, and therefore, requests a discharge. between respect for autonomy and these other moral Although a psychiatrist confirms Ken's mental copyright. concerns. There follows a review of relevant competence, the hospital doctors refuse to discharge commentary from the classicists Kant and Mill and the him. -

Early Medieval G
University of Richmond UR Scholarship Repository Religious Studies Faculty Publications Religious Studies 2001 History of Western Ethics: Early Medieval G. Scott aD vis University of Richmond, [email protected] Follow this and additional works at: http://scholarship.richmond.edu/religiousstudies-faculty- publications Part of the Ethics in Religion Commons, and the History of Christianity Commons Recommended Citation Davis, G. Scott. "History of Western Ethics: Early Medieval." In Encyclopedia of Ethics, edited by Lawrence Becker and Charlotte Becker, 709-15. 2nd ed. Vol. 2. New York: Routledge, 2001. This Article is brought to you for free and open access by the Religious Studies at UR Scholarship Repository. It has been accepted for inclusion in Religious Studies Faculty Publications by an authorized administrator of UR Scholarship Repository. For more information, please contact [email protected]. history of Western ethics: 5. Early Medieval Copyright 2001 from Encyclopedia of Ethics by Lawrence Becker and Charlotte Becker. Reproduced by permission of Taylor and Francis, LLC, a division of Informa plc. history of Western ethics: 5. Early Medieval ''Medieval" and its cognates arose as terms of op probrium, used by the Italian humanists to charac terize more a style than an age. Hence it is difficult at best to distinguish late antiquity from the early middle ages. It is equally difficult to determine the proper scope of "ethics," the philosophical schools of late antiquity having become purveyors of ways of life in the broadest sense, not clearly to be distin guished from the more intellectually oriented ver sions of their religious rivals. This article will begin with the emergence of philosophically informed re flection on the nature of life, its ends, and respon sibilities in the writings of the Latin Fathers and close with the twelfth century, prior to the systematic reintroduction and study of the Aristotelian corpus. -

NARRATIVE, CASUISTRY, and the FUNCTION of CONSCIENCE in THOMAS AQUINAS – Stephen Chanderbhan –
Diametros 47 (2016): 1–18 doi: 10.13153/diam.47.2016.865 NARRATIVE, CASUISTRY, AND THE FUNCTION OF CONSCIENCE IN THOMAS AQUINAS – Stephen Chanderbhan – Abstract. Both the function of one’s conscience, as Thomas Aquinas understands it, and the work of casuistry in general involve deliberating about which universal moral principles are applicable in particular cases. Thus, understanding how conscience can function better also indicates how casuistry might be done better – both on Thomistic terms, at least. I claim that, given Aquinas’ de- scriptions of certain parts of prudence (synesis and gnome) and the role of moral virtue in practical knowledge, understanding particular cases more as narratives, or parts of narratives, likely will result, all else being equal, in more accurate moral judgments of particular cases. This is especially important in two kinds of cases: first, cases in which Aquinas recognizes universal moral principles do not specify the means by which they are to be followed; second, cases in which the type-identity of an action – and thus the norms applicable to it – can be mistaken Keywords: Thomas Aquinas, conscience, narrative, casuistry, prudence, virtue, moral judgment, moral development, moral knowledge. Introduction ‘Casuistry’ has a bad reputation in some circles. It tends to be associated wi- th formalized, but too legalistic, approaches to determining and enumerating mo- ral faults. In a more generic sense, though, casuistry just refers to deliberating about and discerning what universal moral principles apply in particular cases, based on relevant details of the case at issue. As Thomas Aquinas understands things, casuistry parallels the ordinary, everyday function of one’s conscience, which specifically regards particular cases in which one deliberates about one’s own morally relevant actions.1 Given this, we might be able to gain insight to how formalized casuistry can be done well by drawing an analogy from what it takes for conscience to function well. -

American Psychiatric Association the Principles of Medical Ethics
American Psychiatric Association The Principles of Medical Ethics With Annotations Especially Applicable to Psychiatry 2013 Edition Copyright © 2010 American Psychiatric Association ALL RIGHTS RESERVED Manufactured in the United States of America 08 07 06 3 2 1 The Principles of Medical Ethics 2013 Edition (Previous editions 1973, 1978, 1981, 1984, 1985, 1989, 1992, 1993, 1995, 1995 Revised, 1998, 2001, 2001 Revised, 2006, 2008, 2009. 2009 Revised, and 2010 American Psychiatric Association 1000 Wilson Boulevard #1825 Arlington, VA 22209 THE PRINCIPLES OF MEDICAL ETHICS With Annotations Especially Applicable to Psychiatry 2013 Edition In 1973, the American Psychiatric Association (APA) published the first edition of The Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry. Subsequently, revisions were published as the APA Board of Trustees and the APA Assembly approved additional annotations. In July of 1980, the American Medical Association (AMA) approved a new version of the Principles of Medical Ethics (the first revision since 1957), and the APA Ethics Committee1 incorporated many of its annotations into the new Principles, which resulted in the 1981 edition and subsequent revisions. This version includes changes to the Principles approved by the AMA in 2001. Foreword ALL PHYSICIANS should practice in accordance with the medical code of ethics set forth in the Principles of Medical Ethics of the American Medical Association. An up-to-date expression and elaboration of these statements is found in the Opinions and Reports of the Council on Ethical and Judicial Affairs of the American Medical Association.2 Psychiatrists are strongly advised to 3 be familiar with these documents. However, these general guidelines have sometimes been difficult to interpret for psychiatry, so further annotations to the basic principles are offered in this document. -

Clinician Conscience Objection and Ethical Care of Patients
1 VERMONT MEDICAL SOCIETY RESOLUTION 2 3 Clinician Conscience Objection and Ethical Care of Patients 4 5 As adopted at the VMS Annual Meeting on November 2, 2019 6 7 RESOLVED, that the VMS Policy on Physician Conscience be amended to read: The 8 Vermont Medical Society recognizes that the provision of certain types of medical care 9 or treatment can come in conflict with members’ cultural values, ethics or religious 10 beliefs. The Vermont Medical Society commits to protecting its members’ (physicians, 11 physician assistants, medical students) freedom to follow their own conscience in 12 deciding whether to participate in providing care or treatment, consistent with the 13 ethical norms of their professions, stated for physicians in AMA Code of Ethics Section 14 1.1.7, found in its entirety below, including fidelity to patients, respect for patient self- 15 determination, non-discrimination and informing the patient about all relevant options 16 for treatment, including options to which the physician morally objects, and information 17 regarding how to access such services. 18 19 AMA Code of Medical Ethics Opinion 1.1.7 20 Physicians are expected to uphold the ethical norms of their profession, including fidelity 21 to patients and respect for patient self-determination. Yet physicians are not defined 22 solely by their profession. They are moral agents in their own right and, like their 23 patients, are informed by and committed to diverse cultural, religious, and philosophical 24 traditions and beliefs. For some physicians, their professional calling is imbued with their 25 foundational beliefs as persons, and at times the expectation that physicians will put 26 patients’ needs and preferences first may be in tension with the need to sustain moral 27 integrity and continuity across both personal and professional life. -

The Hippocratic Oath and Principles of Medical Ethics
MEDICINE AND PUBLIC POLICY The Hippocratic Oath and Principles of Medical Ethics Gilbert Berdine MD The Hippocratic Oath is associated with the morally right. This tradition remains in the modern practice of medicine, but over time fewer medical era. “As God is my witness I hereby pledge to …” can graduates have taken any form of the Hippocratic be found in modern rituals to stress the seriousness Oath. As of 2006, the State University of New York of purpose. Courts in the U.S. require prospective Upstate Medical School in Syracuse was the only witnesses to pledge their truthfulness: “Do you sol- U.S. medical school that administered the classic emnly swear or affirm that you will tell the truth, the version of the Hippocratic Oath to its graduates. The whole truth, and nothing but the truth, so help you Hippocratic Oath has been revised to make it more God?” This pledge becomes a source of contention in acceptable to modern schools, but the medical pro- a multi-cultural society as some members believe in fession no longer has a common set of promises that other deities. guide it. This article will look at the classic version of the Hippocratic Oath to see why it has been aban- Anyone who takes his or her religion seriously doned. Modern medical students wish to graduate would not pledge to a pagan god as this would be a into an ancient order of physicians, so they long for form of idolatry. This pledge is probably the main rea- a solemn ceremony, but it is difficult to craft a solemn son that the Oath has been abandoned in the modern ceremony that remains agreeable to a diverse group era, but what can take its place as a symbol of seri- of students. -

Glossary of Medical Ethics and Hospice Care
Center for Bioethics and Health Policy Glossary of Medical Ethics and Hospice Care Before defining the terms commonly used in medical ethics and hospice care, it might be reasonable to ask: What is medical ethics and how does ethics differ from morals? Morals relates to the principles of right and wrong behavior, i.e., a specific act is right or it is wrong, end of question: to murder is wrong. Ethics, on the other hand, is a system of moral principles that apply values and judgments to accepted professional standards of conduct. Medical ethics evolve/devolve, i.e., what may have been considered ethical behavior in the 19th century may not be considered ethical in the 21st century and vice versa, e.g., eugenics was accepted as ethical behavior in the early 20th century. The Tuskegee study was accepted from its inception in the mid 1930s until it was abruptly discontinued in 1972. Advanced Health Care Directive (Living Will) - a document in which a person gives advanced directions about medical care, or designates who should make medical decisions for the person if they should lose their decision making capacity, or both. There are two types: treatment directive (Living Will), and proxy/surrogate directives (Healthcare Power of Attorney). Allow Natural Death (Allow to Die) – involves the withholding or withdrawing of life- sustaining treatment that is judged by the patient or proxy to be excessively burdensome and/or of little or no benefit. It involves a decision to no longer prevent the underlying disease process or pathology to run its course. Assent – a concept that applies to minors and refers to their right to have their own perspective represented in all decision making about their health care. -

Downloadable%20File/New Published Maps and Institutional Affiliations
Swazo et al. Philosophy, Ethics, and Humanities in Medicine (2020) 15:7 https://doi.org/10.1186/s13010-020-00091-6 RESEARCH Open Access A Duty to treat? A Right to refrain? Bangladeshi physicians in moral dilemma during COVID-19 Norman K. Swazo1*, Md. Munir Hossain Talukder2 and Mohammad Kamrul Ahsan2 Abstract Background: Normally, physicians understand they have a duty to treat patients, and they perform accordingly consistent with codes of medical practice, standards of care, and inner moral motivation. In the case of COVID-19 pandemic in a developing country such as Bangladesh, however, the fact is that some physicians decline either to report for duty or to treat patients presenting with COVID-19 symptoms. At issue ethically is whether such medical practitioners are to be automatically disciplined for dereliction of duty and gross negligence; or, on the contrary, such physicians may legitimately claim a professional right of autonomous judgment, on the basis of which professional right they may justifiably decline to treat patients. Methods: This ethical issue is examined with a view to providing some guidance and recommendations, insofar as the conditions of medical practice in an under-resourced country such as Bangladesh are vastly different from medical practice in an industrialized nation such as the USA. The concept of moral dilemma as discussed by philosopher Michael Shaw Perry and philosopher Immanuel Kant’s views on moral appeal to “emergency” are considered pertinent to sorting through the moral conundrum of medical care during pandemic. Results: Our analysis allows for conditional physician discretion in the decision to treat COVID-19 patients, i.e., in the absence of personal protective equipment (PPE) combined with claim of duty to family. -

Health Care Ethics and Casuistry
Jrournal ofmedical ethics, 1992, 18, 61-62, 66 J Med Ethics: first published as 10.1136/jme.18.2.61 on 1 June 1992. Downloaded from Guest editorial: A personal view Health care ethics and casuistry Robin Downie University ofGlasgow In an editorial (1) Dr Gillon looks at some recent method of teaching and discussing medical ethics. The difficulties which have been raised about philosophy answer to Smith here is to point out that what is taking and the teaching ofhealth care ethics. This matter is of place in such discussions is a form of what he calls sufficient importance to the readers of this journal that 'natural jurisprudence'. It is an attempt to translate it is worth looking at it again, this time in an historical into case law, to give concrete application to, the ideals perspective. contained in codes. If natural jurisprudence is a One claim which is often made by those advocating legitimate activity, so too is this. the study of health care ethics is that such a study will Smith's second group ofarguments against casuistry assist in the solving of what have come to be called are to the effect that it does not 'animate us to what is 'ethical dilemmas'. Since health care ethics is so widely generous and noble' but rather teaches us 'to chicane taught for this reason the claim is worth examining. Is with our consciences' (4). Smith is certainly correct in health care ethics in this sense possible? Is it desirable? claiming that casuistry is concerned mainly with whatcopyright. Is it philosophy? In other words, can a case be made out is required or forbidden, that is, with rules, rather than for what earlier centuries called 'casuistry, or the with questions of motivation.