Informed Consent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Impossibility of Informed Consent?
JME40: Good medical ethics J Med Ethics: first published as 10.1136/medethics-2014-102308 on 16 December 2014. Downloaded from PAPER The impossibility of informed consent? Kenneth Boyd Correspondence to ABSTRACT medical ethics’ over the 40 years of the Journal’s Professor Kenneth Boyd, The problematic nature of informed consent to medical publication. Biomedical Teaching Organisation, Edinburgh treatment and research, and its relation to autonomy, trust and clinical practice, has been addressed on many University, Edinburgh, Scotland Surveying the scene: the law and ethics of EH89AG, UK; occasions and from a variety of ethical perspectives in informed consent to treatment and research [email protected] the pages of the Journal of Medical Ethics. This paper Two early and wide-ranging contributions on medi- gives an account of how discussion of these issues has Received 1 September 2014 colegal and ethical aspects of informed consent developed and changed, by describing a number of Revised 26 September 2014 were made in papers by judge Kirby3 of Australia Accepted 23 October 2014 significant contributions to these debates which provide in 1983 and paediatrician Silverman4 of the USA in examples of ‘doing good medical ethics’ over the 1989. Both agreed that a paternalist or beneficence- 40 years of the Journal’s publication. based approach, in which the doctor recommends a course of treatment to which the patient either con- sents or refuses, had properly been superseded by THE IMPOSSIBILITY OF INFORMED CONSENT? an approach based on respect for the autonomy or Awareness that informed consent is problematic, in right to self-determination of the individual theory and in practice, was already evident in the patient. -

Whose Life Is It Anyway? a Study in Respect for Autonomy
Journal ofmedical ethics 1995; 21: 179-183 J Med Ethics: first published as 10.1136/jme.21.3.179 on 1 June 1995. Downloaded from Medicine and literature Whose Life Is It Anyway? A study in respect for autonomy Margaret Norden Marymount University, Arlington, Virginia, USA Abstract Precis of the story Brian Clark's drama, Whose Life Is It Anyway? (1), Whose Life Is It Anyway? opens with the explores the difficulties ofapplying the principle of hospitalization of Ken Harrison who was critically respect for autonomy to real-life circumstances. In the injured in an automobile accident four months play a permanently disabled patient, who wishes to be earlier and permanently paralyzed from the neck allowed to die, raises moral questions about the down. Although Ken arrived in critical condition, he adequacy of the autonomous agent, respect for the has since been stabilized, informed by his doctors autonomy ofothers, the authority of the law, the that his paralysis is permanent, and advised that he allocation ofsociety's resources, and the intrinsic value will be transferred to a long-term care facility. Facing ofhuman life. After a brief review of the story and the prospect of such an existence, Ken chooses not definition of respect for autonomy, this paper cites to live. He realizes that he could not survive outside passages from the play that dramatize the tension of an institution, and therefore, requests a discharge. between respect for autonomy and these other moral Although a psychiatrist confirms Ken's mental copyright. concerns. There follows a review of relevant competence, the hospital doctors refuse to discharge commentary from the classicists Kant and Mill and the him. -

Human Challenge Trials for Vaccine Development: Regulatory Considerations
POST ECBS Version ENGLISH ONLY EXPERT COMMITTEE ON BIOLOGICAL STANDARDIZATION Geneva, 17 to 21 October 2016 Human Challenge Trials for Vaccine Development: regulatory considerations © World Health Organization 2016 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

Informed Consent and Refusal
CHAPTER 3 Informed Consent and Refusal Evolution of the doctrine of informed consent Elements of informed consent and refusal The nature of informed consent Exceptions to the consent requirement Mrs. Stack is a 67- year- old woman admitted with rectal bleeding, chronic renal in- sufficiency, diabetes, and blindness. On admission, she was alert and capacitated. Two weeks later, she suffered a cardiopulmonary arrest, was resuscitated and intu- bated, and was transferred to the medical intensive care unit (MICU) in an unrespon- sive and unstable state. Consent for emergency dialysis was obtained from her son, who is also her health care agent. Dialysis was repeated two days later. During the past several years, Mrs. Stack has consistently stated to her family and her primary care doctor that she would never want to be on chronic dialysis and she has refused it numerous times when it was recommended. The physician, who has known and treated Mrs. Stack for many years, also treated her daughter who had been on chronic dialysis for some time and had died after suffering a heart attack. According to the physician and the patient’s family, Mrs. Stack’s refusal of dialysis has been based on her conviction that her daughter died as a result of the dialysis treatments. Mrs. Stack’s mental status has cleared considerably and, despite the ventilator, she is able to communicate nonverbally. Although she appears to understand the benefits of dialysis and the consequences of refusing it, including deterioration and eventual death, she has consistently and vehemently refused further treatments. Her capacity to make this decision is not now in question. -

The Implications of Religious Beliefs on Medical and Patient Care
University of Pennsylvania ScholarlyCommons Master of Science in Organizational Dynamics Theses Organizational Dynamics Programs 11-14-2011 The Implications of Religious Beliefs on Medical and Patient Care Dana I. Al Husseini University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/od_theses_msod Al Husseini, Dana I., "The Implications of Religious Beliefs on Medical and Patient Care" (2011). Master of Science in Organizational Dynamics Theses. 46. https://repository.upenn.edu/od_theses_msod/46 Submitted to the Program of Organizational Dynamics in the Graduate Division of the School of Arts and Sciences in Partial Fulfillment of the Requirements for the Degree of Master of Science in Organizational Dynamics at the University of Pennsylvania Advisor: Adrian Tschoegl This paper is posted at ScholarlyCommons. https://repository.upenn.edu/od_theses_msod/46 For more information, please contact [email protected]. The Implications of Religious Beliefs on Medical and Patient Care Abstract Throughout history and to this date in a continuously globalized world, monotheistic religions and medicine have caused numerous acrimonious debates especially in crucial moments of life and death. Medical and nursing staff working with patients from different religions in any country in the world must adhere to and respect those patients’ faiths and be aware of them to provide better patient care and in worst case scenarios, avoid litigation. Furthermore, this paper should not to be treated as an encyclopedic reference; it is merely a general overview into the three monotheistic faiths to alert professional healthcare staff of the possibility of a religious implication even if it contradicts their own concerns and points of views. -
Informed Consent
Christine Grady Department of Bioethics NIH Clinical Center The views expressed here are mine and do not necessarily represent those of the CC, NIH, or Department of Health and Human Services Informed consent is the bedrock principle on which most of modern research ethics rest…This was at the heart of the crucial ethical provision stated in the first words of the Nuremberg Code, and it remains equally compelling a half century later. Menikoff J, Camb Quarterly 2004 p 342 Authorization of an activity based on understanding what the activity entails. A legal, regulatory, and ethical requirement in health care and in most research with human subjects A process of reasoned decision making (not a form or an episode) One aspect of conducting ethical clinical research “Every human being of adult years and sound mind has a right to determine what will be done with his body… Justice Cardozo, 1914 Respect for autonomy or for an individual’s capacity and right to define own goals and make choices consistent with those goals. Well entrenched in American values, jurisprudence, medical practice, and clinical research. “Informed consent is rooted in the fundamental recognition…that adults are entitled to accept or reject health care interventions on the basis of their own personal values and in furtherance of their own personal goals” Presidents Commission for the study of ethical problems…1982 Informed consent in medical practice …informed consent in clinical practice is frequently inadequate… Physicians receive little training… Misunderstand requirements and legal standards… Time pressures and competing demands… Patient comprehension is often poor… Recent studies have demonstrated improvement in patient understanding of risks after communication interventions Schenker et al 2010; Matiasek et al. -

Informed Consent for Participation in Personal Training
PRINCETON UNIVERSITY Personal Training INFORMED CONSENT FOR PARTICIPATION IN PERSONAL TRAINING Name: ________________________ 1. Purpose and Explanation of Procedure I desire to participate voluntarily in an acceptable plan of exercise conditioning. I also desire to be placed in program activities which are recommended to me for improvement of my general health and well-being in which I will be given exact instructions regarding the amount and kind of exercise I should do. Professionally trained personnel will provide leadership to direct my activities, monitor my performance and otherwise evaluate my effort. Depending upon my health status, I may or may not be required to have my heart rate evaluated during these sessions and/or regulate my exercise within desired limits. I understand that I am expected to follow staff instructions with regard to the proper performance of each exercise. I have been advised and understand it is recommended that I obtain a medical examination by a physician before I participate in this program. The medical examination is highly suggested in order to identify conditions which may preclude participation. If I am taking prescribed medications, I have already so informed the program staff and further agree to inform them promptly of any changes which my doctor or I may make with regard to such use. I have been informed that during my participation in exercise, I will be asked to complete the physical activities unless such symptoms as fatigue, shortness of breath, chest discomfort or similar occurrences appear. At that point, I have been advised it is my complete right and responsibility to decrease or stop exercising and that it is my obligation to inform the program personnel of my symptoms. -
TWU IRB Reference Sheet for Recruitment and Informed Consent
TWU IRB Reference Sheet for Recruitment and Informed Consent RECRUITMENT Recruitment Materials (flyers, email scripts, social media posts, etc.) • Items that are required: • State that research will be conducted • State that participation is voluntary • If the internet/email is used for participation, include the following statement: “There is a potential risk of loss of confidentiality in all email, downloading, electronic meetings, and internet transactions.” • Items that are NOT required, but recommended: • PI’s contact information (email is recommended over cell phone #, but both are okay) • Location/site of the study • Study title • Brief description of the study • If using a TWU logo, TWU marketing is asking that you use the new logo • Main eligibility requirements • Benefits for participation • Total time commitment • If your scripts will vary across different platforms (email script, social media post, phone script, etc.), make sure you attach all appropriate scripts. If you are using the same script across all platforms, state so. • Make sure the information you include is consistent with the information you provide in the application and consent form. • Remember, it is okay to leave out details that are subject to change (e.g., study or session dates, gift card vendors). It is very possible that your study will not start when you want it to. If you leave out actual dates, you will not need to submit a modification request to change it later. The same thing goes with gift cards. If your study is funded, you may work with ORSP to get gift cards. You may need 40 $5 gift cards, but they do not have 40 from the same vendor. -
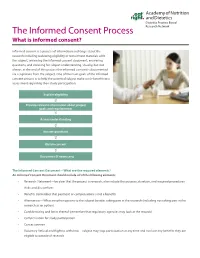
The Informed Consent Process Research Network What Is Informed Consent?
Dietetics Practice Based The Informed Consent Process Research Network What is informed consent? Informed consent is a process of information exchange about the research including reviewing eligibility or recruitment materials with the subject, reviewing the informed consent document, answering questions, and checking for subject understanding. Usually, but not always, at the end of this process the informed consent is documented via a signature from the subject. One of the main goals of the informed consent process is to help the potential subject make a risk-benefit ratio assessment regarding their study participation. Explain eligibility Provide relevant information about project goals and requirements Assess understanding Answer questions Obtain consent Document (if necessary) The Informed Consent Document—What are the required elements? An Informed Consent Document should include all of the following elements: • Research Statement—be clear that the project is research, also include the purpose, duration, and required procedures • Risks and discomforts • Benefits (remember that payment or compensation is not a benefit) • Alternatives—What are other options to the subject besides taking part in the research (including not taking part in the research as an option) • Confidentiality and limits thereof (remember that regulatory agencies may look at the records) • Compensation for study participation • Contact person • Voluntary Refusal and Right to withdraw—subject may stop participation at any time and not lose any benefits they are -

Bioethics and Informed Consent
Bioethics and Informed Consent Professor Lucy Allais Informed consent is a central notion in bioethics. The emphasis on informed consent in medical practice is relatively recent (20th century). Bioethics is a relatively young field, beginning, in the USA, in the 50s and 60s, maturing in the 80s and 90s. This is different to both medical ethics, and ethics generally. Medical ethics Reflections by doctors and societies on the ethics of medical practice is probably as old as doctoring (Hippocratic oath; the Code of Hammurabi, written in Babylon in 1750 BC). Traditionally focused on the doctor-patient relationship and the virtues possessed by the good doctor. (Kuhse and Singer A Companion to Bioethics 2001:4). Ethics in philosophy: Morality: how should we live? what is right? what is wrong? Ethics: the academic study of morality. Are there objective values? Are there truths about right and wrong? What makes actions wrong? How do we resolve moral disputes? What is the basis of human rights? When (if ever) is euthanasia permissible? Is it morally justifiable to incarcerate MDR TB patients? “in 1972, no American medical school thought medical ethics important enough to be taught to all future physicians.... A decade later, in 1984—after the advent of bioethics—84 percent of medical schools required students to take a course in medical ethics or bioethics during their first two years of instruction.” (Baker 2013) The four core values of autonomy, justice, beneficence and non-maleficence. Autonomy often dominates discussions of bioethics. 6 Informed consent is linked to autonomy. Autonomy means being self-governing. Autonomy is often thought to be at the basis of human rights: human rights protect the capacities of each individual to live their life for themself. -

American Psychiatric Association the Principles of Medical Ethics
American Psychiatric Association The Principles of Medical Ethics With Annotations Especially Applicable to Psychiatry 2013 Edition Copyright © 2010 American Psychiatric Association ALL RIGHTS RESERVED Manufactured in the United States of America 08 07 06 3 2 1 The Principles of Medical Ethics 2013 Edition (Previous editions 1973, 1978, 1981, 1984, 1985, 1989, 1992, 1993, 1995, 1995 Revised, 1998, 2001, 2001 Revised, 2006, 2008, 2009. 2009 Revised, and 2010 American Psychiatric Association 1000 Wilson Boulevard #1825 Arlington, VA 22209 THE PRINCIPLES OF MEDICAL ETHICS With Annotations Especially Applicable to Psychiatry 2013 Edition In 1973, the American Psychiatric Association (APA) published the first edition of The Principles of Medical Ethics with Annotations Especially Applicable to Psychiatry. Subsequently, revisions were published as the APA Board of Trustees and the APA Assembly approved additional annotations. In July of 1980, the American Medical Association (AMA) approved a new version of the Principles of Medical Ethics (the first revision since 1957), and the APA Ethics Committee1 incorporated many of its annotations into the new Principles, which resulted in the 1981 edition and subsequent revisions. This version includes changes to the Principles approved by the AMA in 2001. Foreword ALL PHYSICIANS should practice in accordance with the medical code of ethics set forth in the Principles of Medical Ethics of the American Medical Association. An up-to-date expression and elaboration of these statements is found in the Opinions and Reports of the Council on Ethical and Judicial Affairs of the American Medical Association.2 Psychiatrists are strongly advised to 3 be familiar with these documents. However, these general guidelines have sometimes been difficult to interpret for psychiatry, so further annotations to the basic principles are offered in this document. -

Clinician Conscience Objection and Ethical Care of Patients
1 VERMONT MEDICAL SOCIETY RESOLUTION 2 3 Clinician Conscience Objection and Ethical Care of Patients 4 5 As adopted at the VMS Annual Meeting on November 2, 2019 6 7 RESOLVED, that the VMS Policy on Physician Conscience be amended to read: The 8 Vermont Medical Society recognizes that the provision of certain types of medical care 9 or treatment can come in conflict with members’ cultural values, ethics or religious 10 beliefs. The Vermont Medical Society commits to protecting its members’ (physicians, 11 physician assistants, medical students) freedom to follow their own conscience in 12 deciding whether to participate in providing care or treatment, consistent with the 13 ethical norms of their professions, stated for physicians in AMA Code of Ethics Section 14 1.1.7, found in its entirety below, including fidelity to patients, respect for patient self- 15 determination, non-discrimination and informing the patient about all relevant options 16 for treatment, including options to which the physician morally objects, and information 17 regarding how to access such services. 18 19 AMA Code of Medical Ethics Opinion 1.1.7 20 Physicians are expected to uphold the ethical norms of their profession, including fidelity 21 to patients and respect for patient self-determination. Yet physicians are not defined 22 solely by their profession. They are moral agents in their own right and, like their 23 patients, are informed by and committed to diverse cultural, religious, and philosophical 24 traditions and beliefs. For some physicians, their professional calling is imbued with their 25 foundational beliefs as persons, and at times the expectation that physicians will put 26 patients’ needs and preferences first may be in tension with the need to sustain moral 27 integrity and continuity across both personal and professional life.