Download File
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Strategies to Increase ß-Cell Mass Expansion
This electronic thesis or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Strategies to increase -cell mass expansion Drynda, Robert Lech Awarding institution: King's College London The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. END USER LICENCE AGREEMENT Unless another licence is stated on the immediately following page this work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence. https://creativecommons.org/licenses/by-nc-nd/4.0/ You are free to copy, distribute and transmit the work Under the following conditions: Attribution: You must attribute the work in the manner specified by the author (but not in any way that suggests that they endorse you or your use of the work). Non Commercial: You may not use this work for commercial purposes. No Derivative Works - You may not alter, transform, or build upon this work. Any of these conditions can be waived if you receive permission from the author. Your fair dealings and other rights are in no way affected by the above. Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 02. Oct. 2021 Strategies to increase β-cell mass expansion A thesis submitted by Robert Drynda For the degree of Doctor of Philosophy from King’s College London Diabetes Research Group Division of Diabetes & Nutritional Sciences Faculty of Life Sciences & Medicine King’s College London 2017 Table of contents Table of contents ................................................................................................. -
The Evolutionary Origin of the Vasopressin/V2-Type Receptor/ Aquaporin Axis and the Urine-Concentrating Mechanism
Endocrine (2012) 42:63–68 DOI 10.1007/s12020-012-9634-y MINI REVIEW The evolutionary origin of the vasopressin/V2-type receptor/ aquaporin axis and the urine-concentrating mechanism Kristian Vinter Juul Received: 5 December 2011 / Accepted: 8 February 2012 / Published online: 29 February 2012 Ó Springer Science+Business Media, LLC 2012 Abstract In this mini-review, current evidence for how circadian regulation of urine volume and osmolality that the vasopressin/V2-type receptor/aquaporin axis developed may lead to enuresis and nocturia. co-evolutionary as a crucial part of the urine-concentrating mechanism will be presented. The present-day human Keywords Arginine vasopressin Á V2-R Á AQPs Á kidney, allowing the concentration of urine up to a maxi- Evolution mal osmolality around 1200 mosmol kg-1—or urine to plasma osmolality ratio around 4—with essentially no sodium secreted is the result of up to 3 billion years evo- Introduction lution. Moving from aquatic to terrestrial habitats required profound changes in kidney morphology, most notable the The evolutionary process that ultimately lead to the loops of Henle modifying the kidneys from basically a development of the urine-concentrating mechanism was water excretory system to a water conserving system. originally proposed by Homer Smith, the ‘Father of Renal Vasopressin-like molecules has during the evolution played Physiology’ [1], and is now generally accepted: First cru- a significant role in body fluid homeostasis, more specifi- cial step was salt water vertebrates’ simple nephron cally, the osmolality of body liquids by controlling the developing into nephrons with large glomerular capillaries elimination/reabsorption of fluid trough stimulating and proximal and distal tubules in fresh water vertebrates, V2-type receptors to mobilize aquaporin water channels in allowing the excretion of the vast amounts of excess water the renal collector tubules. -

Receptor-Arrestin Interactions: the GPCR Perspective
biomolecules Review Receptor-Arrestin Interactions: The GPCR Perspective Mohammad Seyedabadi 1,2 , Mehdi Gharghabi 3, Eugenia V. Gurevich 4 and Vsevolod V. Gurevich 4,* 1 Department of Toxicology & Pharmacology, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari 48471-93698, Iran; [email protected] 2 Pharmaceutical Sciences Research Center, Faculty of Pharmacy, Mazandaran University of Medical Sciences, Sari 48167-75952, Iran 3 Department of Cancer Biology and Genetics, The Ohio State University Wexner Medical Center, Columbus, OH 43210, USA; [email protected] 4 Department of Pharmacology, Vanderbilt University, Nashville, TN 37232, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-615-322-7070; Fax: +1-615-343-6532 Abstract: Arrestins are a small family of four proteins in most vertebrates that bind hundreds of different G protein-coupled receptors (GPCRs). Arrestin binding to a GPCR has at least three functions: precluding further receptor coupling to G proteins, facilitating receptor internalization, and initiating distinct arrestin-mediated signaling. The molecular mechanism of arrestin–GPCR interactions has been extensively studied and discussed from the “arrestin perspective”, focusing on the roles of arrestin elements in receptor binding. Here, we discuss this phenomenon from the “receptor perspective”, focusing on the receptor elements involved in arrestin binding and empha- sizing existing gaps in our knowledge that need to be filled. It is vitally important to understand the role of receptor elements in arrestin activation and how the interaction of each of these elements with arrestin contributes to the latter’s transition to the high-affinity binding state. A more precise knowledge of the molecular mechanisms of arrestin activation is needed to enable the construction of arrestin mutants with desired functional characteristics. -

Homogeneous Time-Resolved Fluorescence-Based Assay To
Homogeneous time-resolved fluorescence-based assay to monitor extracellular signal-regulated kinase signaling in a high-throughput format Mohammed Akli Ayoub, Julien Trebaux, Julie Vallaghe, Fabienne Charrier-Savournin, Khaled Al-Hosaini, Arturo Gonzalez Moya, Jean-Philippe Pin, Kevin D. Pfleger, Eric Trinquet To cite this version: Mohammed Akli Ayoub, Julien Trebaux, Julie Vallaghe, Fabienne Charrier-Savournin, Khaled Al- Hosaini, et al.. Homogeneous time-resolved fluorescence-based assay to monitor extracellular signal- regulated kinase signaling in a high-throughput format. Frontiers in Endocrinology, Frontiers, 2014, 5, pp.94. 10.3389/fendo.2014.00094. hal-01943335 HAL Id: hal-01943335 https://hal.archives-ouvertes.fr/hal-01943335 Submitted on 3 Dec 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. METHODS ARTICLE published: 23 June 2014 doi: 10.3389/fendo.2014.00094 Homogeneous time-resolved fluorescence-based assay to monitor extracellular signal-regulated kinase signaling in a high-throughput format Mohammed Akli Ayoub1*, JulienTrebaux 2, -

Download the Poster
Real-Time Kinetic Analysis of GPCR Signaling in Stable PathHunter® Cell Lines Paul Tewson (Montana Molecular), Sam Hoare (Pharmechanics), Thom Hughes (Montana Molecular), Anne Marie Quinn (Montana Molecular), Paul Shapiro (Eurofins DiscoverX), Nurulain T. Zaveri (Astraea Therapeutics) Overview Investigate GPCR biology with a simple protocol that Kinetic measurements make it possible to extract combines DiscoverX cells and Montana Molecular the initial rate parameter (kTau), which can be used • Eurofins DiscoverX stable cell lines are widely used biosensors to quantify agonist activity at GPCRs such as the tools in GPCR drug discovery, providing endpoint DAY 1 TRANSDUCE AND PLATE CELLS Nociceptin Opioid receptor (OPRL1) assays for G-protein signaling, GPCR internalization, STEP 1 The green cADDis Sensor 20 and β-arrestin recruitment. Prepare cells NOFQ 1. µM can be used in DiscoverX cells 10 nM expressing the Nociceptin 1.8 Opioid receptor to detect • Montana Molecular offers genetically-fluorescent 10 M 2+ + + Gi signaling. Dose response biosensors to detect cAMP, DAG, PIP2 , Ca , c GMP, STEP 2 BacMam Media HDAC 1.6 3.2 nM measurements to the agonist β-arrestin, and cell stress. Prepare viral transduction reaction Inhibitor Transduction Mix 1 nM nociceptin/orphanin FQ were 1.4 made, and the kinetic data was 0.2 nM used use determine the EC50 • The fluorescent sensors can be used effectively in both 0. nM by calculating the initial rate STEP 3 1.2 PathHunter® and cAMP Hunter® CHO-K1 cell lines to 0.032 M of activity (kTau) at each dose. Mix cells and transduction reaction + The initial rate of signaling 1.0 monitor signaling kinetics of G-protein and β-arrestin 0.01 nM (kTau) is a direct measure of pathways in live cells, in real time. -

Biased Signaling of G Protein Coupled Receptors (Gpcrs): Molecular Determinants of GPCR/Transducer Selectivity and Therapeutic Potential
Pharmacology & Therapeutics 200 (2019) 148–178 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Biased signaling of G protein coupled receptors (GPCRs): Molecular determinants of GPCR/transducer selectivity and therapeutic potential Mohammad Seyedabadi a,b, Mohammad Hossein Ghahremani c, Paul R. Albert d,⁎ a Department of Pharmacology, School of Medicine, Bushehr University of Medical Sciences, Iran b Education Development Center, Bushehr University of Medical Sciences, Iran c Department of Toxicology–Pharmacology, School of Pharmacy, Tehran University of Medical Sciences, Iran d Ottawa Hospital Research Institute, Neuroscience, University of Ottawa, Canada article info abstract Available online 8 May 2019 G protein coupled receptors (GPCRs) convey signals across membranes via interaction with G proteins. Origi- nally, an individual GPCR was thought to signal through one G protein family, comprising cognate G proteins Keywords: that mediate canonical receptor signaling. However, several deviations from canonical signaling pathways for GPCR GPCRs have been described. It is now clear that GPCRs can engage with multiple G proteins and the line between Gprotein cognate and non-cognate signaling is increasingly blurred. Furthermore, GPCRs couple to non-G protein trans- β-arrestin ducers, including β-arrestins or other scaffold proteins, to initiate additional signaling cascades. Selectivity Biased Signaling Receptor/transducer selectivity is dictated by agonist-induced receptor conformations as well as by collateral fac- Therapeutic Potential tors. In particular, ligands stabilize distinct receptor conformations to preferentially activate certain pathways, designated ‘biased signaling’. In this regard, receptor sequence alignment and mutagenesis have helped to iden- tify key receptor domains for receptor/transducer specificity. -

Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

1 Pharmacological Characterization of AZD5069, a Slowly Reversible CXCR2 Antagonist Table S1. Kinase Panel Screening Performe
Pharmacological Characterization of AZD5069, a Slowly Reversible CXCR2 Antagonist Nicholls DJ, Wiley K, Dainty I, MacIntosh F, Phillips C, Gaw A, Kärrman Mårdh C. JPET #221358 Pharmacological Characterization of AZD5069, a Slowly Reversible CXCR2 Antagonist David Nicholls, Katherine Wiley, Ian Dainty, Fraser MacIntosh, Caroline Phillips, Alasdair Gaw, Carina Kärrman Mårdh. The Journal of Pharmacology and Experimental Therapeutics Table S1. Kinase panel screening performed at Dundee University ATP Inhibition Target (μM) (%) AMP-activated Protein Kinase 50 19 Cyclin Dependent Kinase 2:Cyclin A 20 18 Checkpoint Kinase I 20 10 Casein Kinase 1 20 -6 Casein Kinase 2 5 4 Lymphocyte-Specific Protein Tyrosine Kinase 50 -5 Mitogen Activated Protein Kinase 1 50 13 MAPK Activated Protein Kinase-1a 50 -3 MAPK Activated Protein Kinase-2 20 13 Mitogen Activated Protein Kinase Kinase 1 5 21 Protein Kinase, cAMP-dependent, catalytic, alpha 5 -71 v-akt murine thymoma viral oncogene homolog 1 5 19 Protein Kinase C alpha 20 9 p38 Regulated Activated Kinase 20 7 Dual Specificity Tyrosine Phosphorylation Regulated Kinase 1A 50 15 Glycogen Synthase Kinase-3 beta 5 12 Mitogen Activated Protein Kinase 8 20 9 Mitogen and Stress Activated Protein Kinase 1 20 8 P70S6 Kinase 20 22 Phospho B Kinase 20 4 3-Phosphoinositide Dependent Protein Kinase-1 20 10 Rho Associated, Coiled Coil Containing Protein Kinase 2 20 2 Stress Activated Protein Kinase 2a 50 4 Stress Activated Protein Kinase 2b 20 17 Serum and Glucocorticoid Regulated Kinase? 20 11 1 Pharmacological Characterization of AZD5069, a Slowly Reversible CXCR2 Antagonist Nicholls DJ, Wiley K, Dainty I, MacIntosh F, Phillips C, Gaw A, Kärrman Mårdh C. -

Pflugers Final
CORE Metadata, citation and similar papers at core.ac.uk Provided by Serveur académique lausannois A comprehensive analysis of gene expression profiles in distal parts of the mouse renal tubule. Sylvain Pradervand2, Annie Mercier Zuber1, Gabriel Centeno1, Olivier Bonny1,3,4 and Dmitri Firsov1,4 1 - Department of Pharmacology and Toxicology, University of Lausanne, 1005 Lausanne, Switzerland 2 - DNA Array Facility, University of Lausanne, 1015 Lausanne, Switzerland 3 - Service of Nephrology, Lausanne University Hospital, 1005 Lausanne, Switzerland 4 – these two authors have equally contributed to the study to whom correspondence should be addressed: Dmitri FIRSOV Department of Pharmacology and Toxicology, University of Lausanne, 27 rue du Bugnon, 1005 Lausanne, Switzerland Phone: ++ 41-216925406 Fax: ++ 41-216925355 e-mail: [email protected] and Olivier BONNY Department of Pharmacology and Toxicology, University of Lausanne, 27 rue du Bugnon, 1005 Lausanne, Switzerland Phone: ++ 41-216925417 Fax: ++ 41-216925355 e-mail: [email protected] 1 Abstract The distal parts of the renal tubule play a critical role in maintaining homeostasis of extracellular fluids. In this review, we present an in-depth analysis of microarray-based gene expression profiles available for microdissected mouse distal nephron segments, i.e., the distal convoluted tubule (DCT) and the connecting tubule (CNT), and for the cortical portion of the collecting duct (CCD) (Zuber et al., 2009). Classification of expressed transcripts in 14 major functional gene categories demonstrated that all principal proteins involved in maintaining of salt and water balance are represented by highly abundant transcripts. However, a significant number of transcripts belonging, for instance, to categories of G protein-coupled receptors (GPCR) or serine-threonine kinases exhibit high expression levels but remain unassigned to a specific renal function. -

A Novel Mutation in the Avpr2gene Causing Congenital Nephrogenic
ORI GI NAL AR TIC LE DO I: 10.4274/jcrpe.0097 J Clin Res Pediatr Endocrinol 2018;10(4):350-356 A Novel Mutation in the AVPR2 Gene Causing Congenital Nephrogenic Diabetes Insipidus Aslı Çelebi Tayfur1*, Tuğçe Karaduman2*, Merve Özcan Türkmen2, Dilara Şahin2, Aysun Çaltık Yılmaz1, Bahar Büyükkaragöz1, Ayşe Derya Buluş3, Hatice Mergen2 1Keçiören Training and Research Hospital, Clinic of Pediatric Nephrology, Ankara, Turkey 2Hacettepe University Faculty of Science, Department of Biology, Ankara, Turkey 3Keçiören Training and Research Hospital, Clinic of Pediatric Endocrinology, Ankara, Turkey *These authors contributed equally to this work. What is already known on this topic? About 90 percent of all cases of hereditary nephrogenic diabetes insipidus result from mutations in the AVPR2 gene. To date, more than 250 mutations have been identified comprising missense, nonsense, small insertions and deletions, large deletions and complex rearrangements in AVPR2 gene. What this study adds? In this study, we found a novel hemizygous missense mutation in the AVPR2 gene at the position 80th in exon 2 causing congenital nephrogenic diabetes insipidus in a 6-year-old boy presenting with growth failure and dull normal cognitive functions. Abstract Objective: Congenital nephrogenic diabetes insipidus (CNDI) is a rare inherited disorder characterized by a renal insensitivity to arginine vasopressin (AVP). In the majority of the cases, CNDI is caused by mutations in the arginine vasopressin receptor 2 (AVPR2) gene. Our objective is to report a novel mutation in the AVPR2 gene causing CNDI in a 6-year-old boy, presenting with growth failure and dull normal cognitive functions. Methods: The proband was the third off-spring of non-consanguineous parents and had polyuria (4.3 L/day), polydipsia (5 L/day). -

Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 12-2013 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Medical Cell Biology Commons, and the Medical Molecular Biology Commons Recommended Citation Bogard, Amy Sue , "Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells" (2013). Theses and Dissertations (ETD). Paper 330. http://dx.doi.org/10.21007/etd.cghs.2013.0029. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Document Type Dissertation Degree Name Doctor of Philosophy (PhD) Program Biomedical Sciences Track Molecular Therapeutics and Cell Signaling Research Advisor Rennolds Ostrom, Ph.D. Committee Elizabeth Fitzpatrick, Ph.D. Edwards Park, Ph.D. Steven Tavalin, Ph.D. Christopher Waters, Ph.D. DOI 10.21007/etd.cghs.2013.0029 Comments Six month embargo expired June 2014 This dissertation is available at UTHSC Digital Commons: https://dc.uthsc.edu/dissertations/330 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells A Dissertation Presented for The Graduate Studies Council The University of Tennessee Health Science Center In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy From The University of Tennessee By Amy Sue Bogard December 2013 Copyright © 2013 by Amy Sue Bogard. -
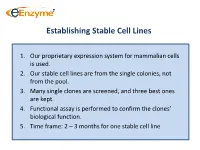
Establishing Stable Cell Lines
Establishing Stable Cell Lines 1. Our proprietary expression system for mammalian cells is used. 2. Our stable cell lines are from the single colonies, not from the pool. 3. Many single clones are screened, and three best ones are kept. 4. Functional assay is performed to confirm the clones’ biological function. 5. Time frame: 2 – 3 months for one stable cell line List of In-Stock ACTOne GPCR Stable Clones Transduced Gi-coupled receptors (22) Transduced Gs coupled receptors (34) Cannabinoid receptor 1 (CB1) Vasoactive Intestinal Peptide Receptor 2 (VIPR2) Dopamine Receptor 2 (DRD2) Melanocortin 4 Receptor (MC4R) Melanocortin 5 Receptor (MC5R) Somatostatin Receptor 5 (SSTR5) Parathyroid Hormone Receptor 1 (PTHR1) Adenosine A1 Receptor (ADORA1) Glucagon Receptor (GCGR) Chemokine (C-C motif) receptor 5 (CCR5) Dopamine Receptor 1 (DRD1) Melanin-concentrating Hormone Receptor 1 (MCHR1) Prostaglandin E Receptor 4 (EP4) Vasoactive Intestinal Peptide Receptor 1 (VIPR1) Cannabinoid receptor 2 (CB2) Gastric Inhibitor Peptide Receptor (GIPR) Glutamate receptor, metabotropic 8 (GRM8) Dopamine Receptor 5 (DRD5) Opioid receptor, kappa 1 (OPRK1) Parathyroid Hormone Receptor 2 (PTHR2) Adenosine A3 receptor (ADORA3) 5-hydroxytryptamine (serotonin) receptor 6 (HTR4) Corticotropin Releasing Hormone Receptor 2 (CRHR2) Glutamate receptor, metabotropic 8 (GRM8) Adenylate Cyclase Activating Polypeptide 1 Receptor type I (ADCYAP1R1) Neuropeptide Y Receptor Y1 (NPY1R) Secretin Receptor (SCTR) Neuropeptide Y Receptor Y2 (NPY2R) Follicle