E035930.Draft-Revisions.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplemental Data
Appendix: Omega 3 Fatty Acids (Fish Oils) and Aspirin in Vascular Access Outcomes in Renal Disease (FAVOURED) Study Collaborative Group The FAVOURED Study Collaborative Group comprises the Trial Steering Committee (Chen Au Peh [CNARTS, Royal Adelaide Hospital, Adelaide, Australia], Elaine Beller [Faculty of Health Services and Medicine, Bond University, Gold Coast, Australia], Alan Cass [School Menzies School of Health Research, Darwin, Australia], Sharan Dogra [Department of Renal Medicine, Sir Charles Gairdner Hospital, Perth, Australia], David Gracey [Department of Renal Medicine, Royal Prince Alfred Hospital, Sydney, Australia], Elvie Haluszkiewicz [Department of Vascular Surgery, Royal Perth Hospital, Perth, Australia], Carmel Hawley [Department of Nephrology, Princess Alexandra Hospital, Brisbane, Queensland, Australia], Lai-Seong Hooi [Hemodialysis Unit, Hospital Sultanah Aminah, Johor Bahru, Malaysia], Colin Hutchison [Renal Services, Hawkes Bay Hospital, Hawke’s Bay, New Zealand], Ashley Irish [Department of Nephrology Fiona Stanley Hospital, Perth, Western Australia, Australia], Peter Kerr [Department of Nephrology, Monash Medical Centre, Melbourne, Australia], Amanda Mather [Department of Renal Medicine, Royal North Shore Hospital, Sydney, Australia], Stephen McDonald [CNARTS, Royal Adelaide Hospital, Adelaide, Australia], Chris McIntyre [London Health Sciences Centre, Ontario, Canada], Trevor Mori [Medical School, RPH Unit, The University of Western Australia, Perth, Australia], Elaine Pascoe [Australasian Kidney Trials Network, -

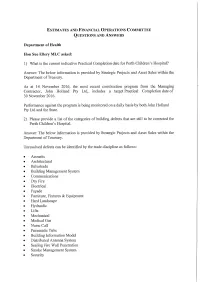
2019-20 Budget Statement Part 5 Health
Part 5 Health Introduction The Health portfolio delivers a safe, high quality and sustainable health system to help Western Australians live healthy lives. The portfolio has an increased emphasis on prevention and promotion in all areas of health and mental wellbeing. The portfolio is contributing to the achievement of the following Our Priorities and associated targets: • A Bright Future − improving the health and wellbeing of children in the early years; • A Safer Community − reducing illicit drug use; and • Sustainable Health Review. Summary of Recurrent and Asset Investment Expenditure 2018-19 2019-20 Estimated Budget Agency Actual Estimate $’000 $’000 WA Health − Total Cost of Services ........................................................................................... 8,994,191 9,134,503 − Asset Investment Program .................................................................................... 245,197 339,948 Mental Health Commission − Total Cost of Services ........................................................................................... 918,406 942,125 − Asset Investment Program .................................................................................... - 1,508 Health and Disability Services Complaints Office − Asset Investment Program .................................................................................... - 300 Animal Resources Authority − Asset Investment Program .................................................................................... 1,672 200 265 Ministerial Responsibilities -
Ef.Aar15.161118.Aon.001.Jd.Pdf
According to our patients, the best Hospital contacts: thing about their health journey was: Armadale Health Service PO Box 460, ARMADALE WA 6112 “Found staff in “Every midwife Telephone: (08) 9391 2000 admissions very that I encountered www.ahs.health.wa.gov.au You’ve told us…. helpful to make sure was fantastic, what was being said friendly, kind and Bentley Health Service was understood.” knowledgeable.” PO Box 158, BENTLEY WA 6982 we’re listening Telephone: (08) 9416 3666 “The doctor in the “From a bad www.bhs.health.wa.gov.au resuscitation ward situation, my hospital gave the clearest and experience was Fiona Stanley Hospital most understandable excellent to help me Locked Bag 100, PALMYRA DC 6961 explanation I’ve ever care for myself in the Telephone: (08) 6152 2222 had.” future.” www.fsh.health.wa.gov.au Fremantle Hospital and Health Service PO Box 480, FREMANTLE WA 6959 Telephone: (08) 9431 3333 Where to from here www.fh.health.wa.gov.au Rockingham General Hospital Our individual hospitals are listening to their patients. PO Box 2033, Rockingham WA 6967 Your feedback is guiding the various teams to Telephone: (08) 9599 4000 reassess how they can better keep their patients and www.rkpg.health.wa.gov.au families informed throughout their hospital and health service journey. Royal Perth Hospital GPO Box X2213, PERTH WA 6847 Through ongoing patient experience surveys over the Telephone: (08) 9224 2244 next two years, we will continue to make the necessary www.rph.health.wa.gov.au changes to meet our patients’ expectations and build on what we already do well. -

Health Department of Western Australia Healtha DISCUSSION PAPER
health2020A DISCUSSION PAPER THE METROPOLITAN HEALTH STRATEGIC PLANNING SERIES Health Department of Western Australia A CKNOWLEDGEMENT The many people and organisations who participated in the development of this discussion paper are acknowledged, particularly the Metropolitan Health Strategic Planning Committee who included: Dr Dianne McCavanagh Chairperson Representative, Health Department of Western Australia General Manager, Strategic Planning and Evaluation Dr Neale Fong Representative, Health Department of Western Australia Chief General Manager, Operations Dr Gareth Goodier Representative, Metropolitan Health Service Board Chief Executive Officer, PMH/KEMH Professor Louis Landau Representative, Metropolitan Health Service Board Executive Dean, Faculty of Medicine and Dentistry, University of Western Australia Ms Helen Lynes Community Member Mrs Helen Morton Representative, Metropolitan Health Service Board General Manager, Armadale Health Service Dr Bryant Stokes Representative, Health Department of Western Australia Chief Medical Officer Particular thanks should go to those individuals who provided background papers on specific issues including Dr Bill Beresford, Mr Don Black, Dr Scott Blackwell, Mr Alan Buckley, Dr Penny Burns, Mr David Cronin, Mr Eric Dillon, Ms Judith Finn, Professor David Fletcher, Dr Peter Goldswain, Dr Gareth Goodier, Mr Ian Haupt, Professor Michael Hobbs, Professor D’Arcy Holman, Mr David Inglis, Mr David Jacobs, Ms Stephanie Kirkham, Mr Alex Kirkwood, Professor Louis Landau, Professor George Lipton, Ms -

Cancer Care Closer to Home May 2016
Cancer care closer to home May 2016 WA Health has strongly invested in cancer care to support the 11,700 Western Australians diagnosed with cancer every year. The recent opening of Fiona Stanley Hospital and St John of God Midland Public Hospital ensure patients have access to excellent cancer care no matter where they live in the metropolitan area. These services are complemented by existing services at the Comprehensive Cancer Centre at Sir Charles Gairdner Hospital, Royal Perth Hospital, Rockingham General Hospital and Joondalup Health Campus with specialist cancer care at Princess Margaret Hospital and King Edward Memorial Hospital. Fiona Stanley Hospital (FSH) also houses a Comprehensive Cancer Centre which includes 22 consulting/interview rooms for cancer outpatients, a chemotherapy unit, a day therapy unit, a radiation oncology suite, radiation therapy planning and a breast assessment centre. The Cancer Centre has been developed around a private courtyard and features a separate entrance and drop-off area to improve privacy and access for patients and their visitors. What treatment can patients expect? With 80 per cent of FSH's cancer patients treated as outpatients, the cancer service has taken a multidisciplinary approach to treatment. This means several specialties work together, including physicians, radiology, pathology, radiation, medical oncology, nursing, counselling, family support services, and allied health. Patients also have access to services such as physiotherapy, clinical psychology, occupational therapy, social work, pharmacy, dietetics and speech pathology, all in one location. 1 Patients receiving targeted radiation therapies benefit from greatly reduced waiting times and faster treatment with state- of-the- art equipment such as the latest in linear accelerator (linac) technology. -

Patient Information Booklet
Fiona Stanley Fremantle Hospitals Group Patient information Fiona Stanley Hospital Contents Welcome to Fiona Stanley Hospital 2 Vending machines 6 Before you arrive – what to bring 3 Phones 6 Returning home 3 Mobile devices 6 The right care in the right place 3 Photography and recording 6 Smoking 6 My healthcare rights 4 Alcohol and drugs 6 Transport and parking 4 Pastoral Care Service 6 Public transport 4 Aboriginal Health Liaison Service 7 Taxi ranks 4 Interpreting services 7 Patient set down 4 Assistive devices 7 Paid parking 4 Preventing infections 7 Parking rates 4 Your identification 7 On arrival 5 Pressure injuries (bed sores) 7 Where do I need to go? 5 Medications 7 Private patients 5 Teaching 7 Admission 5 Involving your General Practitioner 7 Disability access 5 Feedback, compliments and complaints 8 On the ward 5 Patient and Family Liaison Service 8 Finding your way 5 Care Opinion 8 During your stay 5 Surveys 8 Health record 5 Donations 8 Patient enquiries 5 Carers WA 9 Visiting times 6 Map 10 Facilities 6 Patient entertainment 6 Meal times 6 Welcome to Fiona Stanley Hospital We would like you to be as comfortable as possible during your stay. This booklet is designed to provide you with information about what to expect during your hospital stay and what services and amenities are available for you and your visitors. Fiona Stanley Hospital (FSH) is the major tertiary hospital in the south metropolitan area, commissioned to meet the growing needs of communities south of Perth and across the State. We are committed to providing the very best patient care and provide high-quality health services including a full range of acute medical and surgical services, maternity, paediatric and neonate units, a State Rehabilitation Service, purpose-built mental health unit and the State burns service. -

Who Can Make a Complaint Or Provide Feedback?
How to make a complaint in the WA Health System Carly Parry- Advocacy Manager In the WA Health System, anyone can make a complaint or provide feedback, including…….. • Consumers • Families • Carers • Visitors Making a complaint, which option is right for you? Direct to The Health Service If you wish to comment on, compliment or complain about, any service received in a hospital or health service, you might want to first raise your concerns with the attending staff, either verbally or in writing. If you want the service to provide you with a response, you can request this. You can ask the service to provide their response to you verbally and/or in writing. When providing feedback or making a complaint, let the service know if you are seeking a specific resolution/outcome. Resolution for you might be…. • An apology • A change to a service’s processes • A reimbursement or refund • A second medical opinion WA Hospitals and Public Health Services….. Each WA Public Health Service & Hospital has an internal department that manages complaints and feedback. These departments are often referred to as a Family, Patient or Consumer Liaison/ Experience Service. You can contact a hospital’s main switchboard and ask to be transferred to the Patient Liaison Office. You can make a complaint over the phone or in writing. WA Health (Public) Services, must follow the “Complaints Management Policy.” Under this policy, a health service should; • Aim to provide a response to you within 30 working days. If they need more time, they should let you know at 15 day intervals. -
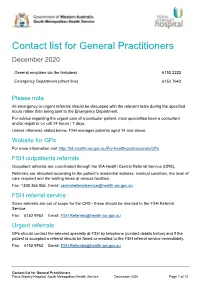
FSH Contact List For
Contact list for General Practitioners December 2020 General enquiries via the Helpdesk 6152 2222 Emergency Department (direct line) 6152 7642 Please note All emergency or urgent referrals should be discussed with the relevant team during the specified hours rather than being sent to the Emergency Department. For advice regarding the urgent care of a particular patient, most specialties have a consultant and/or registrar on call 24 hours / 7 days. Unless otherwise stated below, FSH manages patients aged 14 and above. Website for GPs For more information visit http://fsh.health.wa.gov.au/For-health-professionals/GPs FSH outpatients referrals Outpatient referrals are coordinated through the WA Health Central Referral Service (CRS). Referrals are allocated according to the patient’s residential address, medical condition, the level of care required and the waiting times at various facilities. Fax: 1300 365 056 Email: [email protected] FSH referral service Some referrals are out of scope for the CRS - these should be directed to the FSH Referral Service. Fax: 6152 9762 Email: [email protected] Urgent referrals GPs should contact the relevant specialty at FSH by telephone (contact details below) and if the patient is accepted a referral should be faxed or emailed to the FSH referral service immediately. Fax: 6152 9762 Email: [email protected] Contact list for General Practitioners Fiona Stanley Hospital, South Metropolitan Health Service December 2020 Page 1 of 12 Specialty Routine enquiries -

Royal Perth Hospital Emeritus Consultant Biographies
Royal Perth Hospital Emeritus Consultant biographies Volume three Contents Thomas Ahern ............................................................................................................................. 3 Nicholas Anastas ......................................................................................................................... 4 Trevor ApSimon ........................................................................................................................... 5 Peter Barnes ................................................................................................................................ 6 Nicholas Batalin ........................................................................................................................... 7 Colin Bayliss ................................................................................................................................ 8 Peter G. Beahan .......................................................................................................................... 9 David Booth ............................................................................................................................... 10 Richard Bruce ............................................................................................................................ 11 Frederick Clark ........................................................................................................................... 12 Geoffrey Clarke ......................................................................................................................... -

City of Nedlands Heritage List Comprises of the Places Listed Below
+HULWDJH/LVW nedlands.wa.gov.au Under the Planning and Development (Local Planning Schemes) Regulations 2015 – Schedule 2 Deemed Provisions, a local government must establish and maintain a Heritage List to identify places within the Scheme area that are of cultural heritage significance and worthy of built heritage conservation. The City of Nedlands Heritage List comprises of the places listed below. Name of Place Address Suburb Date of Inclusion Gallop House 22 Birdwood Pde DALKEITH 18-Dec-17 Sunset Hospital Birdwood Pde DALKEITH 18-Dec-17 War Memorial Birdwood Pde / Waratah Ave DALKEITH 18-Dec-17 Chisolm House 32 Genesta Cres DALKEITH 18-Dec-17 St Lawrence's Church 56 Viking Rd DALKEITH 18-Dec-17 Irwin Barracks Magazine Stubbs Tce KARRAKATTA 18-Dec-17 Graylands Hospital 1 Brockway Rd MT CLAREMONT 18-Dec-17 Director's House 1 Grainger Dr MT CLAREMONT 18-Dec-17 Director's Gardens Grainger Dr MT CLAREMONT 18-Dec-17 Swanbourne Hospital 1 Heritage La MT CLAREMONT 18-Dec-17 David Foulkes-Taylor Showroom 33 Broadway NEDLANDS 18-Dec-17 Nedlands Tennis Club 121 Bruce St NEDLANDS 18-Dec-17 Old Post Office 35 Stirling Hwy NEDLANDS 18-Dec-17 The Maisonettes 67 Stirling Hwy NEDLANDS 18-Dec-17 Captain Stirling Hotel 80 Stirling Hwy NEDLANDS 18-Dec-17 3HDFH0HPRULDORose Gardens Stirling Hwy NEDLANDS 18-Dec-17 St Margaret's Church 52 Tyrell St NEDLANDS 18-Dec-17 Shenton Park Rehabilitation Hospital 6 Selby St SHENTON PARK 18-Dec-17 Lemnos Hospital Stubbs Tce SHENTON PARK 18-Dec-17 Tom Collins House Kirkwood Rd SWANBOURNE 18-Dec-17 Mattie Furphy House Kirkwood Rd SWANBOURNE 18-Dec-17 Gallop House, Dalkeith PLACE NAME Gallop House OTHER NAMES - PIN No. -
Trauma System and Services
Trauma system and services Report of the Trauma Working Group Dr Simon Towler (Chair) Executive Director Health Policy and Clinical Reform Department of Health WA July 2007 Report of the Trauma Working Group Contents Executive summary 2 The Trauma System 3 Role delineation and hospital designation 3 The WA State Trauma Service 3 Special services in trauma care 5 Pre-hospital triage 6 Establishing a medical retrieval system 6 Trauma registries 7 Western Australian Trauma Services Advisory Group (WATSAG) 7 Education and training 8 Workforce 8 1. Trauma system and services report 9 1.1 Introduction 9 1.2 Health Reform Committee 9 1.3 Trauma Working Group 9 1.4 Injury and Trauma Health Network 10 1.5 The burden of injury on WA hospitals 11 1.6 Trauma data and trends 12 2. Trauma system and services 17 2.1 Towards a systematised approach 17 2.2 Trauma system 17 2.3 Role delineation and hospital designation 18 2.4. The WA State Trauma System 20 2.5. Special services in trauma care 28 3. Pre-hospital services and patient transport 32 3.1 Pre-hospital triage 32 3.2. Triage destination 33 3.3 Retrieval and transfer 34 4. Trauma system support and development 41 4.1 Trauma Registries 41 4.2 Western Australian Trauma Services Advisory Group (WATSAG) 46 4.3 Education and training 47 4.4 Workforce 49 Appendix 1 51 Terms of reference: Trauma Working Group 51 References 53 1 Trauma system and services Report of the Trauma Working Group Executive summary This group, working together with the Injury and Trauma Health Network, will provide the leadership for phasing in the different elements that will constitute the WA Trauma System. -

Fiona Stanley Hospital Junior Doctor Frequently Asked Questions
Fiona Stanley Hospital Junior Doctor Frequently Asked Questions Contents: 1. Overview of Fiona Stanley Hospital (FSH) 2. Opening schedule 3. Site tours and virtual tours 4. Working at FSH during phased opening 5. Applying for junior doctor positions (2015) 6. Available junior doctor placements 7. Accreditation of junior doctor positions 8. Junior doctor terms and rosters 9. Starting work at FSH 10. Junior doctor benefits 11. Medical education 12. Medical staff common room 13. Junior medical officer society 14. Facilities at FSH 15. Information Communication Technology (ICT) 16. Acronyms Fiona Stanley Hospital Page 1 of 10 Junior doctor frequently asked questions 1. Overview of Fiona Stanley Hospital (FSH) When it opens in October 2014, Fiona Stanley Hospital (FSH) will be Western Australia’s new flagship tertiary hospital. Services will transition from other South Metropolitan Health Service (SMHS) sites as part of an area-wide reconfiguration of services. Located about 20 minutes drive from Perth CBD, the hospital is conveniently situated along the Kwinana Freeway and southern railway line some 12km inland from Fremantle. The 783-bed hospital includes all major tertiary specialties and will provide a broad range of clinical experience and teaching for junior medical staff in a new, highly innovative hospital with a vision for rapidly becoming a leader in medical education and training. Some interesting facts about FSH: 783 beds, including the State rehabilitation service 16 wards (averaging 24 beds each) 83% single patient rooms. 15 theatres and 29 imaging rooms Anticipating up to 100,000 emergency presentations in its first year of operation. 135,000m2 gross area (excluding car parks) 2.