Chronic Fatigue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dangerous Vaccines - All the Proof in the World
DANGEROUS VACCINES - ALL THE PROOF IN THE WORLD Chapters: 1. No. 1 Cause Of All Health Problems - Our Health Care System 2. A Pharmacist Questions Vaccines 3. The Myth of Polio & Smallpox Eradication 4. The Myth People Are Living Longer 5. AIDS Drugs Do More Harm Than Good 6. Babies Dying In Vaccine Trials 7. How the MMR and Measles Vaccines Endanger Your Child's Health 8. Doctor Calls Chicken Pox Vaccine Deaths "Reassuring" 9. Deaths & Adverse Reactions from Vaccines 10. Reports on Vaccine Dangers 11. Government Payouts to Vaccine Damaged Victims 12. Doctors Believe Their Technology Is Superior to Mother Nature's 13. The Tamiflu Scam / Dr. Mercola's Total Health Program 14. Scary Medicine: Exposing The Dark Side of Vaccines 15. Extensive Research on Vaccines Proves the Dangers 16. Biased Reporting: A Vaccination Case Study 17. Mercury Toxicity and Autism 18. Horrors of Vaccination Exposed and Illustrated 19. Quotes On Vaccines By Health Care Experts 20. Vaccination Statistics 21. What's Really In Vaccines? Proof of MSG, Formaldehyde, Aluminum and Mercury 22. Additional Vaccine Facts 23. The Flu - Facts Show Different Picture 24. Vaccine Blamed for the Worst Flu Season in Four Years 25. Why Vaccinations Harm Children: Health Experts Sound Off 26. The Flawed Theory Behind Vaccinations & Why MMR Jabs Are Dangerous 27. Waking Up To Vaccine Dangers 28. Pet Vaccine Myths Debunked 29. Questions To Ask Your Physician or Vaccine Advocate 30. Universal Immunization — Medical Miracle or Masterful Mirage 31. Physician’s Warranty of Vaccine Safety 32. The Death of Medicine: An Open Letter to Allopathic Physicians 33. -

DR. J. WESSON ASHFORD Research Advisory Committee on Gulf War
Research Advisory Committee on Gulf War Veterans’ Illnesses DR. J. WESSON ASHFORD War Related Illness and Injury Study Center (WRIISC) CA VA Palo Alto Health Care System Stanford University Health Outcomes Military Exposures (HOME) Gulf War Illnesses (GWI) Acetyl-cholinesterase inhibitor withdrawal hypothesis: Tardive Dysautonomia Research Advisory Committee on Gulf War August 4, 2021 J. Wesson Ashford, MD, PhD Director, WRIISC-CA VA Palo Alto Health Care System [email protected] www.warrelatedillness.va.gov What is Gulf War Illness (GWI)? • A condition that affects 30-40% of Veterans who were deployed to Operations Desert Shield/Storm/Sabre (ODS/S/S) • Collection of symptoms • Weak diagnostic criteria • No accepted pathophysiological explanation • Variety of unestablished biomarkers • No specific treatment Results of Iowa Study – 3,695 Veterans: Symptoms, % Prevalence Non-GW GW Veterans Veterans Fibromyalgia 19.2 9.6 Cognitive Dysfunction 18.7 7.6 Alcohol Abuse 17.4 12.6 Depression 17.0 10.9 Asthma 7.2 4.1 PTSD 1.9 0.8 Sexual Discomfort 1.5 1.1 Chronic fatigue 1.5 0.3 Iowa Persian Gulf Study Group, 1997 Most Frequent Symptoms, Affected Systems of Veterans from Gulf War 1 Frequency of Symptoms of 53,835 Participants in VA Registry (1992–1997) Symptoms Percentage – Fatigue 20.5 – Skin rash 18.4 – Headache 18.0 – Muscle and joint pain 16.8 – Loss of memory 14.0 – Shortness of breath 7.9 – Sleep disturbances 5.9 Systems – Musculoskeletal and connective tissue 25.4 – Mental disorders 14.7 – Respiratory system 14.0 – Skin and subcutaneous -
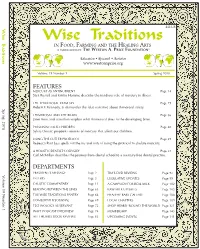
Wise Traditions for Wisetraditions Non Profit Org
® HE ESTON RICE OUNDatION T W A. P F $12 US Wise Traditions for WiseTraditions Non Profit Org. IN FOOD, FARMING AND THE HEALING ARTS U.S. Postage Education Research Activism PAID Wise Traditions PMB 106-380, 4200 WISCONSIN AVENUE, NW Suburban, MD WASHINGTON, DC 20016 Permit 4889 IN FOOD, FARMING AND THE HEALING ARTS A PUBLICatION OF THE WESTON A. PRICE FOUNDatION® Education Research Activism www.westonaprice.org Volume 19 Number 1 Spring 2018 FEATURES MERCURY AS ANTINUTRIENT Page 14 Sara Russell and Kristin Homme describe the insidious role of mercury in illness. THE THIMEROSAL TRAVESTY Page 29 Spring 2018 Robert F. Kennedy, Jr. dismantles the false narrative about thimerosal safety. THIMEROSAL AND THE BRAIN Page 36 Janet Kern and coauthors explain what thimerosal does to the developing brain. ® POISONING OUR CHILDREN Page 40 THE WESTON A. PRICE FOUNDatION Sylvia Onusic pinpoints sources of mercury that affect our children. USING THE CUTLER PROTOCOL Page 49 for WiseTraditions Rebecca Rust Less spells out the ins and outs of using the protocol to chelate mercury. IN FOOD, FARMING AND THE HEALING ARTS Education Research Activism A HOLISTIC DENTIST’S ODYSSEY Page 57 Carl McMillan describes the journey from dental school to a mercury-free dental practice. NUTRIENT DENSE FOODS TRADITIONAL FATS DEPARTMENTS LACTO-FERMENTATION PRESIDENT’S MESSAGE Page 2 TIM’S DVD REVIEWS Page 92 BROTH IS BEAUTIFUL A CAMPAIGN FOR REAL MILK 19 Number 1 Volume TRUTH IN LABELING PREPARED PARENTING SOY ALERT! LETTERS Page 3 LEGISLATIVE UPDATES Page 99 LIFE-GIVING -

2017 Authors Author Address Title Publication
2017 Authors Author Title Publication Abstract address [No authors listed] RE: "MULTI-SITE CLINICAL Am J Epidemiol. 2017 ASSESSMENT OF MYALGIC Jul 1;186(1) :129. ENCEPHALOMYELITIS/CHRONIC FATIGUE SYNDROME (MCAM) : DESIGN AND IMPLEMENTATION OF A PROSPECTIVE/RETROSPECTIVE ROLLING COHORT STUDY". [No authors listed] Correction for Naviaux et al., Proc Natl Acad Sci U Erratum for Proc Natl Acad Sci U S A. 2016 Sep 13;113(37) :E5472- Metabolic features of chronic S A. 2017 May 80. fatigue syndrome. 2;114(18) :E3749. ABDULLA J(15) , Torpy Research Chronic Fatigue Syndrome. In: De Groot LJ(1) , et Chronic fatigue syndrome (CFS) is a common, enigmatic medical BDJ(16) . Professor, Cell al. editors. Endotext condition comprising mental and physical fatigue, diagnosed after and Molecular [Internet]. South exclusion of possible medical causes. The prominence of post- Biology, Dartmouth (MA) : exertional exacerbation of fatigue is highlighted by the recently College of the MDText.com, Inc.; suggested re-naming as Syndrome of Exertional Intolerance Disease Environment 2000-. 2017 Apr 20. (SEID) . Diagnosis is syndromic. No clinical test can confirm the and Life presence of CFS. Treatment is supportive with no specific therapy Sciences, shown to be reproducibly effective. There are several categories of University of hypotheses regarding CFS aetiology including infections, immune, Rhode Island, mitochondrial, neurobehavioural or stress system (HPA axis and Kingston, RI sympathetic nervous system) disorders. Recently, fatigue disorders have been popularly referred to as “adrenal fatigue.― Although CFS and the syndromically related fibromyalgia have been shown to have lower HPA axis function especially reduced cortisol, when analysed compared to controls in aggregate, and in some cases excessive sympathetic nervous system usually sympathoneural system responses, these findings overlap with controls and such testing is not diagnostic. -

Index of ME/CFS Published Research an A-Z Index of the Most Important Published Research
Index of ME/CFS Published Research An A-Z index of the most important published research 1st September 2021 The ME Association The ME Association Index of Published ME/CFS Research Foreword Welcome to the ME Association Index of Published ME/CFS Research. This is an A-Z index of the most important published research studies and selected key documents and articles, listed by subject matter, on myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS). It is correct to 1st August 2021. The Index is updated at the end of each month and we publish a weekly update of recent research publications that are also available on the MEA website and social media. The Index adopts the subject headings used in the MEA Clinical and Research Guide which provides a review of current clinical knowledge and research evidence and is updated annually. This authoritative and very popular book is written by Dr Charles Shepherd, Hon. Medical Adviser to the ME Association and Dr Abhijit Chaudhuri, consultant neurologist at Queen’s Hospital in Romford. The latest edition is available to order from the MEA website shop. We are pleased to be able to offer free hard copies to health professionals upon application and it is also available on Kindle. Please support our vital work If you would like to support our efforts and ensure we are able to inform, support, campaign, and invest in biomedical research, then please donate today. • Just click the image opposite for one-off donations or to establish a regular payment. • You can even establish your own fundraising event on JustGiving. -

Archana Chatterjee Editor Vaccinophobia and Vaccine Controversies of the 21St Century Vaccinophobia and Vaccine Controversies of the 21St Century
Archana Chatterjee Editor Vaccinophobia and Vaccine Controversies of the 21st Century Vaccinophobia and Vaccine Controversies of the 21st Century Archana Chatterjee Editor Vaccinophobia and Vaccine Controversies of the 21st Century Editor Archana Chatterjee, M.D., Ph.D. School of Medicine Creighton University Omaha , NE , USA ISBN 978-1-4614-7437-1 ISBN 978-1-4614-7438-8 (eBook) DOI 10.1007/978-1-4614-7438-8 Springer New York Heidelberg Dordrecht London Library of Congress Control Number: 2013940608 © Springer Science+Business Media New York 2013 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied specifi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. -

Vaccine Controversies: the Case for Freedom and Informed Consent Jane M
Guest Editorial Vaccine Controversies: the Case for Freedom and Informed Consent Jane M. Orient, M.D. The most controversial issue that AAPS has ever been formed Consent (https://physiciansforinformedconsent.org/), involved in is vaccine mandates. The controversy involves a stark medical organizations generally do not oppose mandates. confrontation between individual rights and public health, along Adult vaccines are likely to be more widely mandated soon, with many scientific questions. especially in view of outbreaks of measles, pertussis, and mumps AAPS policy is based on a resolution passed by the Assembly in fully vaccinated adults, whose vaccine-induced immunity at the 2000 annual meeting: apparently waned. AAPS members regularly complain to us WHEREAS: The statement of Patients’ Freedoms adopted about influenza vaccine requirements to work in hospitals or by the Assembly at the 47th annual meeting of AAPS other health facilities. One physician withdrew an application for in 1990 provides that “Patients have the freedom...to consulting privileges because of a demand to prove immunity or refuse medical treatment even if it is recommended recent vaccination against some 15 different diseases. by their physician and to be informed about their The dogma is that “vaccines are safe and effective,” and medical condition, the risks and benefits of treatment, it is our duty to protect the “herd,” especially vulnerable, and appropriate alternatives”; and immunosuppressed children, against vaccine-preventable WHEREAS: There are increasing numbers of mandatory diseases. Raising any question about this is almost certain to childhood vaccines, to which children are often trigger vitriolic accusations of being a danger to the community subjected without meaningful informed consent, as an “anti-science anti-vaxxer.” Nevertheless, serious questions including information about potential adverse side need to be explored with an open, critical mind. -

CFS/ME Literature Review (Jan 2004 – Jun 2009)
CFS/ME Literature Review (Jan 2004 – Jun 2009) A literature review has been included to help inform the workshop participants of the current state of research in the field. A search on Scopus was run using the following search terms and limits: Limits Articles published or entered onto Scopus from 2004 – 2009. Search Terms A search was run using the following search terms: CFS/ME OR chronic fatigue syndrome OR myalgic encephalomyelitis OR myalgic encephalopathy. Autonomic dysfunction inc. cardiovascular abnormalities Van Houdenhove B., Eede F.V.D., Luyten P. Does hypothalamic-pituitary-adrenal axis hypofunction in chronic fatigue syndrome reflect a 'crash' in the stress system? 2009 Medical Hypotheses 72 (6); 701 - 705 http://www.scopus.com/inward/record.url?eid=2-s2.0-62949099218&partnerID=40 Department of Liaison Psychiatry, University Hospitals K.U. Leuven, Herestraat 49, B-3000 Leuven, Belgium; Collaborative Antwerp Psychiatric Research Institute, Department of Psychiatry, Antwerp University Hospital, Antwerp, Belgium; Department of Psychology, K.U. Leuven, Leuven, Belgium The etiopathogenesis of chronic fatigue syndrome (CFS) remains poorly understood. Although neuroendocrine disturbances - and hypothalamic-pituitary-adrenal (HPA) axis hypofunction in particular - have been found in a large proportion of CFS patients, it is not clear whether these disturbances are cause or consequence of the illness. After a review of the available evidence we hypothesize that that HPA axis hypofunction in CFS, conceptualized within a system-biological perspective, primarily reflects a fundamental and persistent dysregulation of the neurobiological stress system. As a result, a disturbed balance between glucocorticoid and inflammatory signaling pathways may give rise to a pathological cytokine-induced sickness response that may be the final common pathway underlying central CFS symptoms, i.e. -

ME/CFS Research Paper 2015-Today
www.millionsmissing.de ME/CFS Research 2015-2019 1/40 31st Oct 2019 Author Year Title Puplication PMID Link Topic Subtopic Murga I and 2019 From neurasthenia to post-exertion disease: Aten Primaria 31182238 https://www.ncbi. 01. Nomenclature Lafuente JV Evolution of the diagnostic criteria of chronic nlm.nih.gov/pub and definition fatigue syndrome/myalgic encephalomyelitis med/31182238 O’Leary D 2019 Ethical classification of ME/CFS in the United Bioethics 30734339 https://www.ncbi. 01. Nomenclature Kingdom nlm.nih.gov/pub and definition med/30734339 Scartozzi S et al. 2019 Myalgic encephalomyelitis and chronic fatigue Fatigue: https://www.tandf 01. Nomenclature syndrome case definitions: effects of requiring a Biomedicine, online.com/doi/a and definition substantial reduction in functioning Health & bs/10.1080/2164 Behavior 1846.2019.16008 Vol 7, 2019 - 25 Issue 2 Twisk FNM 2019 Myalgic Encephalomyelitis, Chronic Fatigue Curr Rheumatol 31073713 https://www.ncbi. 01. Nomenclature Syndrome, and Chronic Fatigue: Three Distinct Rep nlm.nih.gov/pub and definition Entities Requiring Complete Different Approaches med/31073713 Howard H 2018 Recent insights into 3 under recognized Canadian Family 29898928 https://www.ncbi. 01. Nomenclature conditions: Myalgic encephalomyelitis–chronic Physician 64 (6): nlm.nih.gov/pmc/ and definition fatigue syndrome, fibromyalgia, and 413-415 articles/PMC599 environmental sensitivities– multiple chemical 9262/ sensitivity Sharif K, et al 2018 On chronic fatigue syndrome and nosological Clinical 29417255 https://www.ncbi. 01. Nomenclature categories Rheumatology nlm.nih.gov/pub and definition med/29417255 Twisk F 2018 Dutch Health Council Advisory Report on Myalgic Diagnostics 8 (2) 29772739 https://www.ncbi. -

Written Public Comments Stephanie Dorr
Written Public Comments IACC Full Committee Meeting April 17, 2019 1 List of Written Public Comments Stephanie Dorr .............................................................................................................................................. 3 James Strack ................................................................................................................................................ 17 Whitney Ellenby .......................................................................................................................................... 18 Sally Pacholok ............................................................................................................................................. 19 Elissa Leonard ............................................................................................................................................. 20 PrabhakarGupta Garla ................................................................................................................................ 22 Suresh Kalkunte .......................................................................................................................................... 23 Pamela Vandegrift....................................................................................................................................... 24 Sandra McClennen, Ph.D. ........................................................................................................................... 25 Clarissa Kripke, M.D. .................................................................................................................................. -

Earn NCMIC Premium Discounts Full-Time D.C.S Can Attend an 8
9/6/2019 Earn NCMIC Premium Discounts Full-time D.C.s can attend an 8-hour qualifying seminar and receive a 5% discount for 3 consecutive James Demetrious, DC, FACO years on the renewal of their malpractice insurance Fellow, Academy of Chiropractic Orthopedists premium (2.5% discount for part-time D.C.s). Offered by the University of Bridgeport College of Chiropractic and the Connecticut Chiropractic Association Sponsored by National Chiropractic Mutual Insurance Company 2 1 2 Doctorate, New York Chiropractic College Diplomate, American Board of Chiropractic Orthopedists Nationally Distinguished Fellow of the Academy of Chiropractic Orthopedists and American College of Chiropractic Orthopedists NCMIC Speakers’ Bureau Faculty Author - Peer-Reviewed Articles in C&O, JMPT, JNMS, JACA, JACO Editorial Peer Review – Spine, Annals of Internal Medicine, Clinical Anatomy, ACC-RCC Editorial Reviewer Post-graduate Faculty – University Bridgeport – NMSM/Orthopedic Diplomate Program Clinical Practice – >33 years, currently in Wilmington, NC Former Board Member Lower Cape Fear Hospice Past President / Founding Member – Wilmington Regional Autism Parental Support Group 3 4 3 4 Introduction – What is DDX? Trauma/injury/Dose Response? Biologic concepts of connective tissue Connective tissue matrices Myositis/myopathies Tendinitis/tendinopathy/enthesopathies Capsulitis Discogenic issues/discitis Radiculitis/neuritis/myelitis Spine/trunk Upper extremities Lower extremities Conclusion 5 6 5 6 1 9/6/2019 Using Diffusion Imaging, this study revealed that Autism subjects had a decrease of short-range structural “Successful health care hinges upon a connectivity in 13 tracts within the brain associated thorough history and carefully with social cognitive performed examination. deficits. These findings might suggest new targets There are no shortcuts.” for treatment. -

Society of General Internal Medicine
Society of General Internal Medicine 26th Annual Meeting Vancouver, British Columbia April 30±May 3, 2003 ABSTRACTS AN UNUSUAL CASE OF HEART FAILURE. J. Miller1, S. Agrama1, J. Wald1; 1Temple CLINICAL VIGNETTES University, Philadelphia, PA (Tracking ID #76825) LEARNING OBJECTIVES: Recognize that the presenting features of amyloidosis are protean and depend on the organ systems involved. Recognize that cardiac involvement is common in primary amyloidosis and that symptomatic heart involvement carries a poor prognosis. CASE INFORMATION: 66 year old man without PMH presented 8 months of progressive THE INFILTRATING EOSINOPHIL: A CASE OF CHURG STRAUSS SYNDROME. exertional dyspnea and fatigue. Evaluation revealed volume overload with anasarca and signs of G. Agarwal1, R. Granieri1; 1University of Pittsburgh, Pittsburgh, PA (Tracking ID #73667) biventricular heart failure. LEARNING OBJECTIVES: 1) Recognize the presentation of Churg Strauss Syndrome Laboratory studies revealed renal insufficiency with a creatinine of 1.8 and 2+ proteinuria. (CSS). 2) Diagnose CSS using clinical, laboratory, and histologic parameters. 3) Recognize the serum protein electrophoresis with immunofixation showed a monoclonal IgA kappa treatment of CSS. paraprotein; urine protein electrophoresis was unremarkable. Echocardiogram revealed an CASE INFORMATION: F.T. is a 55-year-old male with adult onset asthma who initially ejection fraction of 20%. Right ventricular function was moderately reduced and right and left presented with progressive asthma exacerbations. A leukotriene inhibitor was added to his ventricular hypertrophy was noted. ECG showed atrial fibrillation with a ventricular response regimen of inhaled beta agonists, and his asthma worsened. He subsequently developed low- of 105 BPM and low voltage. grade fevers, anorexia and a twenty pound weight loss over two months.