Hypertensive Retinopathycourse # 40048
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Acute and Long-Term Ocular Effects of Accelerated Hypertension: a Clinical and Electrophysiological Study
THE ACUTE AND LONG-TERM OCULAR EFFECTS OF ACCELERATED HYPERTENSION: A CLINICAL AND ELECTROPHYSIOLOGICAL STUDY 1 2 2 3 3 L2 S. J. TALKS , , P. GOOD , C. G. CLOUGH , D. G. BEEVERS and P. M. DODSON Birmingham SUMMARY the invention of the ophthalmoscope in 1851 the Thirty-four patients with accelerated hypertension were causes of this disturbance could be described? clinically examined. The visual evoked potential (VEP) Leibreich,4 in 1859, was the first to describe and electroretinogram (ERG) were recorded: acutely 'albuminuric retinitis' in Bright's disease. However, in 12 patients, being repeated in 7 patients up to 6 it was not until 1914, after the invention of the Riva months later. In the remaining 22 patients these tests Rocci sphygmomanometer at the end of the nine were performed 2-4 years after presentation. Visual teenth century, that Volhard and Fahr6 related the acuity was 5.6/12 in 22 of 68 (32 %) eyes at presentation retinopathy to arterial hypertension. and 5.6/12 in 10 of 58 (19%) eyes at follow-up. The It was then realised that the fundal appearance cause of severest loss of vision appeared to be anterior was associated with the severity of the hypertension ischaemic optic neuropathy, found in 3 cases. During and with the prognosis of the patient. In 1939 Keith the acute stage 11 patients (92%) had abnormal VEPs et aC drew up a four-group grading system. Grade 3 and all had abnormal ERGs. The group mean PI00 (more recently called accelerated hypertensionS) latency, of the 7 patients (14 eyes) seen acutely and consisted of 'angiospastic retinitis', 'characterised followed up at 6 months, was 123.8 ms with significant especially by oedema, cotton wool patches, and recovery of latency (p<0.005) to 110.9 ms. -

MOC PORT/DOCK Practice Core Modules Content Outline
MOC PORT/DOCK Practice Core Modules Content Outline 1 Cataract and Anterior Segment (10%) 1.1 Basic Anatomical and Scientific Aspects 1.1.1 The Normal Lens 1.1.1.1 Anatomy 1.2 Assessment Techniques 1.2.1 History-Taking and Preoperative Examination of Ocular Structures 1.2.1.1 Take patient history 1.2.1.2 Examine ocular structures 1.2.1.3 Signs and symptoms 1.2.1.4 Indications for surgery 1.2.1.6 External examination 1.2.1.7 Slit-lamp examination 1.2.1.8 Fundus evaluation 1.2.1.9 Impact on visual functioning and quality of life 1.2.2 Measurement of Visual and Macular Function 1.2.2.1 Visual acuity testing 1.2.2.2 Test visual acuity 1.2.2.5 Visual field testing 1.2.2.6 Test visual field 1.2.2.7 Cataract's effect on visual acuity 1.2.2.8 Estimate cataract's effect on visual acuity 1.2.2.10 Measure visual (and macular) function 1.2.4.3 Evaluate glare disability: subjective and objective 1.3 Clinical Disease Conditions and Manifestations 1.3.1 Types of Cataract 1.3.1.1 Identify types of cataracts 1.3.2 Anterior Segment Disorders 1.3.2.1 Diagnose anterior segment disorders 1.3.2.2 Cataract associated with uveitis 1.3.2.3 Diabetes mellitus and cataract formation 1.3.2.4 Lens-induced glaucoma 1.3.2.4.1 Lens particle 1.3.2.4.2 Phacolytic 1.3.2.4.3 Phacomorphic Copyright and Use Policy for ABO Content Outlines © 2017 – American Board of Ophthalmology. -

Ophthalmology July 10-11, 2018 Bangkok, Thailand
J Clin Exp Ophthalmol 2018, Volume 9 conferenceseries.com DOI: 10.4172/2155-9570-C4-088 3rd International Conference on Ophthalmology July 10-11, 2018 Bangkok, Thailand Stage of Hypertensive Retinopathy among Patients who undergone Cataract Surgery in Zamboanga City Medical Center Jerne Kaz Niels B. Paber Dr.evangelista st, sta. Catalina Background: Individuals who are not known hypertensive are noted to have blurring of vision as an initial presentation. Preventable co- morbidity such as hypertension is essential in saving sight in patients with cataract. Objective: To determine the prevalence of hypertension and stage of hypertensive retinopathy among individuals who undergone cataract surgery and to identify the association between the stage of hypertension and the risk factors for hypertension and the stage of hypertensive retinopathy. Methods: This prospective study included 203 individuals. All of the participants were noted to have mature cataract surgery done and was noted to have followed up at Tzu Chi Eye center from July 1 2017 to March 30, 2018. The nature, significance and procedure of the study were explained to every identified respondent. There was only one ophthalmologist who saw the participants who enrolled in the study. Once they understood the study, a written informed consent was taken. They were asked to answer questions provided by the researcher and their laboratory results were recorded. A follow up after 2 weeks was done in order to determine the stage of retinopathy of the patients. Demographic variables, hypertensive retinopathy, history of hypertension, medication usage, compliance, ECG changes, proteinuria, creatinine, and cardiomegaly on chest x-ray, radiographic identification of Atheromatous aorta and fundoscopic examination were analyzed. -

Ocular Co-Morbidity in Patients with Refractive Errors in Nigeria
N igerian Journal of Ophthalmology 2011; 19(1): 19-24 Ocular Co-morbidity in Patients with Refractive Errors in Nigeria BO Adegbehingbe FWA CS, O Adeoye FWA CS, BA Adewara M BBS Ophthalmology Unit, Faculty of Clinical Sciences, Obafemi Awolowo University, Ile-Ife 1-4 ABSTRACT a high proportion of patients attend ing ophthalm ic clinics. Refractive errors can be easily d iagnosed , m easured and Purpose: To d eterm ine the pattern and prevalence of other corrected w ith spectacles or other refractive corrections to ocular problem s seen in patients w ith refractive errors attain normal vision. H ow ever, non correction or inad equate in a N igerian teaching hospital. correction of refractive errors becom es a m ajor cause of low Methods: A retrospective hospital-based review of all vision and even blind ness. Globally, there are 8 m illion consecutive patients w ho presented w ith signs and people w ho are blind and 153 m illion w ith visual sym ptom s of refractive errors at the Obafem i Aw olow o im pairm ent (presenting visual acuity <6/ 18 in the better University Teaching H ospitals Com plex betw een 1st eye) d ue to uncorrected refractive errors; this exclud es January 2007 and 31st August 2007. Patients w ho had a presbyopia.5 Poor visual outcom e in patients w ith refractive d iagnosis of refractive error and su bsequently had errors could be in part d ue to other associated ocular d etailed eye exam ination w ere includ ed in this stud y. -

27 Cardiovascular Disorders
27 Cardiovascular Disorders ◆ Systemic Hypertension Effects of Systemic Hypertension on the Eye and Vision ◆ Hypertensive retinopathy ◆ Hypertensive choroidopathy ◆ Hypertensive optic neuropathy ◆ Central and branch retinal vein occlusion ◆ Retinal macroaneurysm ◆ Vitreous hemorrhage ◆ Subconjunctival hemorrhage ◆ Secondary effects ° Carotid disease—retinal arterial emboli ° Cerebrovascular accident—visual field loss ° Ischemic optic neuropathy ° Oculomotor cranial nerve palsies ° Cataract, glaucoma, age-related macular degeneration Hypertensive Retinopathy Hypertensive retinopathy is usually asymptomatic. In severe hypertension, how- ever, painless loss of vision may occur due to the development of vitreous or reti- nal hemorrhages, retinal edema, retinal vascular occlusion, serous retinal detach- ment, choroidal ischemia, or optic neuropathy. Fundus Features ◆ Focal or diffuse narrowing of retinal arterioles ◆ Increased vascular tortuosity ( Fig. 27.1 ) ◆ Arteriovenous nicking (nipping) ( Fig. 27.2 ) ◆ Retinal hemorrhages ( Fig. 27.3 ) ° Flame-shaped hemorrhage ° Dot and blot hemorrhage ° Preretinal hemorrhage ◆ Microaneurysms ◆ Hard exudates, macular star ◆ Cotton-wool spots (F igs. 27.4 and 27.5 ) ◆ Abnormality of vascular reflex ° Copper-wire reflex ( Fig. 27.6 ) ° Silver-wire reflex ( Fig. 27.7 ) ◆ Intraretinal microvascular abnormalities ◆ Retinal edema ( Fig. 27.8 ) ◆ Serous retinal detachment—occurs secondary to hypertensive choroidopathy in patients with very severe hypertension or eclampsia ( Fig. 27.9 ) ◆ Elschnig spots—small to medium-size hyper- and hypopigmented patches rep- resenting chorioretinal scarring due to prior choroidal infarction ( Figs. 27.10 and 27.11 ) 111 14585C27.indd 111 7/8/09 3:44:46 PM 112 III The Retina in Systemic Disease ◆ Siegrist streaks—linear configurations of hyperpigmentation that have a patho- genesis similar to that of Elschnig spots. ◆ Optic disc edema ( Fig. 27.12 ) ◆ Optic atrophy ◆ Vitreous hemorrhage Fig. -

Hypertension and the Eye
rnib.org.uk/gp [email protected] Hypertension and the eye This factsheet was produced under a collaboration between the UK Vision Strategy, RNIB, and the Royal College of General Practitioners. Key learning points • Hypertensive retinopathy is a clinical diagnosis made when characteristic fundus findings are seen in a patient with or who has had systemic arterial hypertension. • Mild hypertensive retinal features are seen commonly and are of limited relevance, advanced changes represent important signs of accelerated hypertension. • The main complications from hypertension are retinal artery and retinal vein occlusions, and these cause considerable visual morbidity. • Treatment of hypertension may resolve ocular features, but does not improve established vision loss. • Other vascular risk factors eg hyperglycaemia, dyslipidaemia, smoking and abnormal circulation compound the risk and effect of hypertension in the eye. Evidence base: common eye diseases are commoner if the patient is hypertensive • Cataract: In a meta-analysis of 25 studies across the world, risk of cataract was found to be increased in populations with hypertension independent of glycaemic risk, obesity or lipids [1]. We don’t know how generalisable this finding is. • Glaucoma: Nocturnal hypotension is also found to be associated with progression of visual field defects in glaucoma. • Late stage AMD: Some population studies show increased incidence with high © 2016 RNIB Reg charity nos 226227, SC039316 rnib.org.uk/gp [email protected] systolic BP [2], others show incidence associated with the metabolic syndrome but not specifically with hypertension [3]. • Other: Incidental retinal detachment in non-myopic eyes has been found to be more common [4] but again we don’t know how generalisable this is. -
Diabetic Retinopathy by the Numbers a Guide to Following and Educating Patients LACRIMAL OCCLUSION ■ Who Face This Threatening Diagnosis, P
REVIEW OF OPTOMETRY Earn 2 CE Credits: Can You Identify These Vitreous Anomalies?, p. 94 ■ VOL. 153 NO. 6 June 15, 2016 www.reviewofoptometry.com ■ JUNE 15, 2016 ■ ANNUAL 7th Annual Retina Report RETINA REPORT Diabetic Retinopathy By the Numbers ■ A guide to following and educating patients LACRIMAL OCCLUSION who face this threatening diagnosis, p. 36 • Food for Thought: Diet, Genetics and AMD, p. 48 • The Dilation Dilemma p. 54 • Managing Patients with ■ VITREOUS ANOMALIES Hypertensive Crisis, p. 58 ■ VIRAL CONJUNCTIVITIS 125 YEARS Plug the Drain with Lacrimal Occlusion, p. 70 | Claim Victory Over Viral Conjunctivitis, p. 78 001_ro0616_fc.indd 1 6/9/16 9:57 AM We call it our fundamental business truth: 1 20/200 Your success is essential to Our success. When your practice grows and flourishes, so does ours. At Johnson & Johnson Vision Care, we have operated according to this simple, but profound, principle for over 30 years. And it is the inspiration and 2 20/100 energy behind every year of our 3 decades of Global leadership in the contact lens marketplace. But history tells only a small part of the story. It is what we will do together in partnership over 3 20/70 the next 3 decades that will truly change the very meaning of vision care. Our commitment to innovation is unwavering. 4 20/50 But at the center of all of the R & D eff orts—be they technological, educational, or commercial in nature— is our commitment to advancing the eye care profession. 5 20/40 We thank you for your partnership and look forward to the continued journey together. -
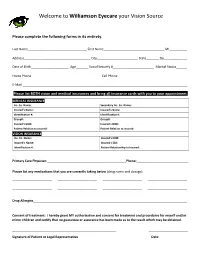
Welcome to Williamson Eyecare Your Vision Source
Welcome to Williamson Eyecare your Vision Source Please complete the following forms in its entirety. Last Name_________________________________ First Name__________________________________ MI__________ Address_____________________________________ City_______________________ State_______ Zip_____________ Date of Birth_____________________ Age_______ Social Security #_______________________ Marital Status______ Home Phone_______________________________________ Cell Phone_______________________________________ E-Mail ____________________________________________________________________________________________ Please list BOTH vision and medical insurances and bring all insurance cards with you to your appointment. MEDICAL INSURANCE Ins. Co. Name: Secondary Ins. Co. Name: Insured’s Name: Insured’s Name: Identification #: Identification #: Group#: Group#: Insured’s DOB: Insured’s DOB: Patient Relation to insured: Patient Relation to insured: VISION INSURANCE Ins. Co. Name: Insured’s DOB: Insured’s Name: Insured’s SS#: Identification #: Patient Relationship to Insured: Primary Care Physician ____________________________________________Phone:_____________________________ Please list any medications that you are currently taking below (drug name and dosage) ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ ______________________ Drug Allergies______________________________________________________________________________________ Consent -

What Is Hypertensive Retinopathy?
What is hypertensive retinopathy? Hypertension, or high blood pressure, can be a spontaneous (primary) condition, but is usually associated with kidney disease or hyperthyroidism. We always recommend a complete blood count (CBC), serum profile / panel, urinalysis and a thyroid (T4) level, if it has not already been recently performed. It is very common to diagnose hypertension only after changes in vision have occurred, because while this medical condition is serious, it is not painful and may not cause any other changes in the pet's behavior. Hypertensive retinopathy, which can include small to extensive areas of retinal detachments and hemorrhage, is often controllable with oral medications. However, systemic hypertension is rarely curable and lifelong treatment is necessary. Eyes with complete (total) retinal detachments, and especially those with significant hemorrhage, tend to be associated with a poorer visual prognosis. Any changes in vision may be permanent. It is important to control blood pressure as much as possible due to the damage that can be caused to the heart and kidneys, as well as the retinas. Regular monitoring of blood pressure and blood testing with your family veterinarian is crucial for optimal long-term management of this condition. An aged cat, blind, with a systemic hypertension and a secondary hypertensive retinopathy: note the complete dilation of the pupil (we can almost not see his yellow irises). Picture of the fundus (retina) of the same cat: note Picture of the fundus (retina) of the same cat after 10 the important hemorrhages. days of medical treatment for systemic hypertension: note that most of the hemorrhages have resolved. -

Non-Diabetic Retinal Vascular Disease”
“Non-Diabetic Retinal Vascular Disease” Brad Sutton, O.D., F.A.A.O. Clinical Professor IU School of Optometry Indianapolis Eye Care Center Retinal Vascular Disease No financial disclosures Hypoperfusion Syndrome Occurs when the eye lacks blood perfusion secondary to carotid artery blockage or ophthalmic artery blockage. Terminology debate: venous stasis retinopathy vs. hypoperfusion syndrome Why is venous stasis retinopathy a poor term for this condition? Hypoperfusion Syndrome Patient may complain of dull, chronic ache in the affected eye Photostress issues / dazzle TIA symptoms may or may not be present (amaurosis fugax) Possible bruit / decreased pulse strength in carotid Hypoperfusion Syndrome Bruit at 30-85% blockage; swishing sound Bell vs. diaphragm Definitive diagnosis requires carotid imaging Hypoperfusion Syndrome Peripheral dot / blot hemorrhages Dilated veins Relatively spares the posterior pole Ocular Ischemic Syndrome With ocular NVD / NVE / NVI ischemic Iritis syndrome same Sluggish pupil findings plus……….. Conjunctival congestion Corneal Edema 80% unilateral / 20% bilateral Ocular Ischemic Syndrome Rare! Only 10% of eyes with 70+% blocked carotids 60% CF or worse VA by one year: 82% if NVI is present Teichopsia: colored afterimages after viewing lights More likely in patients with increased homocysteine and CRP Ocular Ischemic Syndrome When presented with Question about TIA these ocular findings……. Check carotids Arrange for carotid testing (Doppler has limits) ESR C-reactive protein CBC Ocular Ischemic Syndrome Treatment: Systemic management (diet, drugs, surgery) PRP / cryotherapy? Avastin / Lucentis / Eyelea? Five year mortality rate of 40% Sickle Cell Retinopathy Hemoglobinopathy affecting mostly AA (8% in US carry trait, .15% have SS dis.) 60,000 in US: 250,000 born yearly w-wide Malaria and natural selection (sickle trait carriers and sickle cell patients are resistant to malaria) AC, SA, SS, Sthal, SC. -

Comparative Study of Cataract in Hypertensive Patients and Non-Hypertensive Patients
Original Research Article Comparative study of cataract in hypertensive patients and non-hypertensive patients Reshma Mehta1,*, Manjunath Patil2, Shubashree Page3 1,2Assistant Professor, 3JR, Dept. of Ophthalmology, Ashwini Rural Medical College, Solapur, Maharashtra *Corresponding Author: Email: [email protected] Abstract Introduction: The purpose behind conducting this study was to determine if hypertension increases the risk of cataract, to find out common morphological types of cataract in hypertensive patients, to determine relation between grade of hypertension and grade of nuclear sclerosis and to compare prevalence rates of cataract in hypertensive patients on anti-hypertensive drugs and those not on anti-hypertensive drugs. Materials & Methods: Comparative study of cataract in hypertensive patients and non- hypertensive patients was crriedout in in Department of ophthalmology at Ashwini Rural Medical College, Kumbhari, Solapur with 300 eligible participants. Results: This was a comparative study with 156 hypertensive and 144 non-hypertensive patients. Prevalence of cataract was found to be 79.53%. Prevalence of cataract was significantly higher in eyes of hypertensive patients as compared to eyes of non- hypertensive patients; (87.83% and 70.8% respectively, with p-value<0.0001). Significant association was found between high systolic BP and cataract. (χ2=23.82, df= 1, p<0.0001). Nuclear cataract was the most common morphological type in eyes of hypertensive patients (50.4%). However, posterior sub capsular cataract was more common in eyes of hypertensive patients as in eyes of non-hypertensive patients (28.6% and 23.3%). No significant relation was found between grade of hypertension and grade of nuclear sclerosis (χ2 = 4.33, df= 3, p=0.23). -

Public Health and the Eye
SURVEY OF OPHTHALMOLOGY VOLUME 46 • NUMBER 1 • JULY–AUGUST 2001 PUBLIC HEALTH AND THE EYE DONALD FONG AND JOHANNA SEDDON, EDITORS Retinal Microvascular Abnormalities and their Relationship with Hypertension, Cardiovascular Disease, and Mortality Tien Yin Wong, FRCS, MPH,1,2,3 Ronald Klein, MD, MPH,1 Barbara E. K. Klein, MD, MPH,1 James M. Tielsch, PhD,3,4 Larry Hubbard, MAT,1 and F. Javier Nieto, MD, PhD3 1Department of Ophthalmology and Visual Sciences, University of Wisconsin, Madison, Wisconsin, USA, 2Singapore National Eye Center and Department of Ophthalmology, National University of Singapore, Singapore, 3Department of Epidemiology and 4Department of International Health, Johns Hopkins University School of Public Health, Baltimore, Maryland, USA Abstract. Retinal microvascular abnormalities, such as generalized and focal arteriolar narrowing, arte- riovenous nicking and retinopathy, reflect cumulative vascular damage from hypertension, aging, and other processes. Epidemiological studies indicate that these abnormalities can be observed in 2–15% of the nondiabetic general population and are strongly and consistently associated with elevated blood pressure. Generalized arteriolar narrowing and arteriovenous nicking also appear to be irreversible long-term markers of hypertension, related not only to current but past blood pressure levels as well. There are data supporting an association between retinal microvascular abnormalities and stroke, but there is no convincing evidence of an independent or direct association with atherosclerosis, ischemic heart disease, or cardiovascular mortality. New computer-related imaging methods are currently being developed to detect the presence and severity of retinal arteriolar narrowing and other microvascular characteristics. When reliably quantified, retinal microvascular abnormalities may be useful as risk indi- cators for cerebrovascular diseases.