Venous Thrombosis: a Case and a Review Paul F.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Brain Abscess Review of 89 Cases Over a Period of 30 Years
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.36.5.757 on 1 October 1973. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry, 1973, 36, 757-768 Brain abscess Review of 89 cases over a period of 30 years A. J. BELLER, A. SAHAR, AND I. PRAISS From the Department ofNeurosurgery, Hadassah Hebrew University Hospital, Jerusalem, Israel SUMMARY Eighty-nine cases of brain abscess, diagnosed over a period of 30 years, are reviewed. The incidence of this disease did not decline throughout the period. Abscesses of ear and nose origin constituted the largest group (38%). Postoperative abscesses seem to have increased in inci- dence, presumably due to routine postoperative antibiotic treatment. Antibiotics were possibly responsible for the suppression of signs of infection in 4500 of the patients, who presented as suffering from a space-occupying lesion. The most accurate diagnostic tool was angiography, which localized the lesion in 9000 and suggested its nature in 61%. Brain scan may prove as satisfactory. Staphylococcus was cultured in about two-thirds of the cases. Mortality seemed to decrease con- comitantly with the advent of more potent antibiotics. The treatment of choice in terms of both Protected by copyright. mortality and morbidity seemed to be enucleation after previous sterilization. The hazards of radical surgery should be taken into consideration. The multiplicity of factors involved in the or subdural collections of pus were not included management of brain abscess complicates its in this study. evaluation. Surgical therapy in the pre-anti- biotic era carried a mortality of 61% (Webster FINDINGS AND COMMENTS and Gurdjian, 1950). -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

Infections in Deep Brain Stimulator Surgery
Open Access Original Article DOI: 10.7759/cureus.5440 Infections in Deep Brain Stimulator Surgery Jacob E. Bernstein 1 , Samir Kashyap 1 , Kevin Ray 1 , Ajay Ananda 2 1. Neurosurgery, Riverside University Health System Medical Center, Moreno Valley, USA 2. Neurosurgery, Kaiser Permanente, Los Angeles, USA Corresponding author: Jacob E. Bernstein, [email protected] Abstract Introduction: Deep brain stimulation has emerged as an effective treatment for movement disorders such as Parkinson’s disease, dystonia, and essential tremor with estimates of >100,000 deep brain stimulators (DBSs) implanted worldwide since 1980s. Infections rates vary widely in the literature with rates as high as 25%. Traditional management of infection after deep brain stimulation is systemic antibiotic therapy with wound incision and debridement (I&D) and removal of implanted DBS hardware. The aim of this study is to evaluate the infections occurring after DBS placement and implantable generator (IPG) placement in order to better prevent and manage these infections. Materials/Methods: We conducted a retrospective review of 203 patients who underwent implantation of a DBS at a single institution. For initial electrode placement, patients underwent either unilateral or bilateral electrode placement with implantation of the IPG at the same surgery and IPG replacements occurred as necessary. For patients with unilateral electrodes, repeat surgery for placement of contralateral electrode was performed when desired. Preoperative preparation with ethyl alcohol occurred in all patients while use of intra-operative vancomycin powder was surgeon dependent. All patients received 24 hours of postoperative antibiotics. Primary endpoint was surgical wound infection or brain abscess located near the surgically implanted DBS leads. -

Congenital Ocular Anomalies in Newborns: a Practical Atlas
www.jpnim.com Open Access eISSN: 2281-0692 Journal of Pediatric and Neonatal Individualized Medicine 2020;9(2):e090207 doi: 10.7363/090207 Received: 2019 Jul 19; revised: 2019 Jul 23; accepted: 2019 Jul 24; published online: 2020 Sept 04 Mini Atlas Congenital ocular anomalies in newborns: a practical atlas Federico Mecarini1, Vassilios Fanos1,2, Giangiorgio Crisponi1 1Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy 2Department of Surgery, University of Cagliari, Cagliari, Italy Abstract All newborns should be examined for ocular structural abnormalities, an essential part of the newborn assessment. Early detection of congenital ocular disorders is important to begin appropriate medical or surgical therapy and to prevent visual problems and blindness, which could deeply affect a child’s life. The present review aims to describe the main congenital ocular anomalies in newborns and provide images in order to help the physician in current clinical practice. Keywords Congenital ocular anomalies, newborn, anophthalmia, microphthalmia, aniridia, iris coloboma, glaucoma, blepharoptosis, epibulbar dermoids, eyelid haemangioma, hypertelorism, hypotelorism, ankyloblepharon filiforme adnatum, dacryocystitis, dacryostenosis, blepharophimosis, chemosis, blue sclera, corneal opacity. Corresponding author Federico Mecarini, MD, Neonatal Intensive Care Unit, Azienda Ospedaliero-Universitaria Cagliari, University of Cagliari, Cagliari, Italy; tel.: (+39) 3298343193; e-mail: [email protected]. -

Freedman Eyelid Abnormalities
1/16/2018 1 1/16/2018 Upper Lid Lower Lid Protractors Retractors: Levator m. 3rd nerve function Muller’s m. Cranial Nerve VII function Sympathetic Function Inferior Tarsal Muscle Things to Note Lid Apposition to Globe Position of Lid Margins MRD = 3‐5 mm Canthal Insertions Brow Positions 2 1/16/2018 Ptosis Usually age related levator dehiscence, but sometimes a sign of neurologic, mechanical orbital or inflammatory disease Blepharospasm Sign of External Irritation or Neurologic Disease 3 1/16/2018 First Consider Underlying Orbital Disease Orbital Cellulitis, Pseudotumor, Wegener’s Graves Ophthalmopathy, Orbital Varix Orbital Tumors that can mimic inflammatory process: Lacrimal Gland CA, Lymphoma, Lymphangioma, etc. Lacrimal Gland – Dacryoadenitis or tumor Sinus Mucocele Without Inflammatory Appearance, consider above but also… Allergic Eyelid Edema Hormonal Shifts Systemic Disorder – Cardiac, Renal, Hepatic, Thyroid with edema Cutaneous Lymphoma Graves Ophthalmopathy –can just have lid edema w/o inflammatory appearance Lymphedema after trauma, surgery to lids or orbit (e.g. lymphatics in lateral canthus) Traumatic Leak of CSF into upper eyelid (JAMA Oph 2014;312:1485) Blepharochalasis Not True Edema, but might mimic it: Dermatochalasis, Hidden Eyelid or Sub‐Conjunctival Mass, Prolapsed Orbital Fat When your concerned about: Orbital Cellulitis Orbital Pseudotumor Orbital Malignancy Vascular – e.g. CC fistula Proptosis Chemosis Poor Motility Poor Vision Pupil abnormality – e.g. RAPD Orbital Pseudotumor 4 1/16/2018 Good Vision Good Motility -

Carotid-Cavernous Sinus Fistulas and Venous Thrombosis
141 Carotid-Cavernous Sinus Fistulas and Venous Thrombosis Joachim F. Seeger1 Radiographic signs of cavernous sinus thrombosis were found in eight consecutive Trygve 0. Gabrielsen 1 patients with an angiographic diagnosis of carotid-cavernous sinus fistula; six were of 1 2 the dural type and the ninth case was of a shunt from a cerebral hemisphere vascular Steven L. Giannotta · Preston R. Lotz ,_ 3 malformation. Diagnostic features consisted of filling defects within the cavernous sinus and its tributaries, an abnormal shape of the cavernous sinus, an atypical pattern of venous drainage, and venous stasis. Progression of thrombosis was demonstrated in five patients who underwent follow-up angiography. Because of a high incidence of spontaneous resolution, patients with dural- cavernous sinus fistulas who show signs of venous thrombosis at angiography should be followed conservatively. Spontaneous closure of dural arteriovenous fistulas involving branches of the internal and/ or external carotid arteries and the cavernous sinus has been reported by several investigators (1-4). The cause of such closure has been speculative, although venous thrombosis recently has been suggested as a possible mechanism (3]. This report demonstrates the high incidence of progres sive thrombosis of the cavernous sinus associated with dural carotid- cavernous shunts, proposes a possible mechanism of the thrombosis, and emphasizes certain characteristic angiographic features which are clues to thrombosis in evolution, with an associated high incidence of spontaneous " cure. " Materials and Methods We reviewed the radiographic and medical records of eight consecutive patients studied at our hospital in 1977 who had an angiographic diagnosis of carotid- cavernous sinus Received September 24, 1979; accepted after fistula. -

CT Observations Pertinent to Septic Cavernous Sinus Thrombosis
755 CT Observations Pertinent to Septic Cavernous Sinus Thrombosis Jamshid Ahmadi1 The use of high-resolution computed tomography (CT) is described in four patients James R. Keane2 with septic cavernous sinus thrombosis, In all patients CT findings included multiple Hervey D. Segall1 irregular filling defects in the enhancing cavernous sinus. Unilateral or bilateral inflam Chi-Shing Zee 1 matory changes in the orbital soft tissues were also present. Enlargement of the superior ophthalmic vein due to extension of thrombophlebitis was noted in three patients. Since the introduction of antibiotics, septic cavernous sinus thrombosis (throm bophlebitis) has become a rare disease [1-4]. Despite considerable improvement in morbidity and mortality (previously almost universal), it remains a potentially lethal disease. The diagnosis of cavernous sinus thrombophlebitis requires a careful clinical evaluation supplemented with appropriate laboratory and radiographic studies. Current computed tomographic (CT) scanners (having higher spatial and contrast resolution) play an important role in the radiographic evaluation of the diverse pathologiC processes that involve the cavernous sinus [5-7]. The use of CT has been documented in several isolated cases [8-13], and small series [14] dealing with the diagnosis and management of cavernous sinus thrombophlebitis. CT scanning in these cases was reported to be normal in two instances [8 , 10]. In other cases so studied, CT showed abnormalities such as orbital changes [11 , 14], paranasal sinusitis [12], and associated manifestations of intracranial infection [9]; however, no mention was made in these cases of thrombosis within the cavernous sinus itself. Direct CT demonstration of thrombosis within the cavernous sinus has been rarely reported [13]. -

Bacterial Brain Abscess in a Patient with Granulomatous Amebic Encephalitis
SVOA Neurology ISSN: 2753-9180 Case Report Bacterial Brain Abscess in a Patient with Granulomatous Amebic Encephalitis. A Misdiagnosis or Free-Living Amoeba Acting as Trojan Horse? Rolando Lovaton1* and Wesley Alaba1 1 Hospital Nacional Cayetano Heredia (Lima-Peru) *Corresponding Author: Dr. Rolando Lovaton, Neurosurgery Service-Hospital Nacional Cayetano Heredia, Avenida Honorio Delgado 262 San Martin de Porres, Lima-Peru Received: July 13, 2021 Published: July 24, 2021 Abstract Amebic encephalitis is a rare and devastating disease. Mortality rate is almost 90% of cases. Here is described a very rare case of bacterial brain abscess in a patient with recent diagnosis of granulomatous amebic encephalitis. Case De- scription: A 29-year-old woman presented with headache, right hemiparesis and tonic-clonic seizure. Patient was diag- nosed with granulomatous amebic encephalitis due to Acanthamoeba spp.; although, there was no improvement of symptoms in spite of stablished treatment. Three months after initial diagnosis, a brain MRI showed a ring-enhancing lesion in the left frontal lobe compatible with brain abscess. Patient was scheduled for surgical evacuation and brain abscess was confirmed intraoperatively. However, Gram staining of the purulent content showed gram-positive cocci. Patient improved headache and focal deficit after surgery. Conclusion: It is the first reported case of a patient with cen- tral nervous system infection secondary to Acanthamoeba spp. who presented a bacterial brain abscess in a short time. Keywords: amebic encephalitis; Acanthamoeba spp; bacterial brain abscess Introduction Free–living amoebae cause potentially fatal infection of central nervous system. Two clinical entities have been de- scribed for amebic encephalitis: primary amebic meningoencephalitis (PAM), and granulomatous amebic encephalitis (GAE). -

Lower Eyelid Blepharoplasty 23 Roger L
Lower Eyelid Blepharoplasty 23 Roger L. Crumley, Behrooz A. Torkian, and Amir M. Karam Anatomical Considerations the orbicularis oculi muscle and (2) an inner lamella, which includes tarsus and conjunctiva. The skin of the lower 2 In no other area of facial aesthetic surgery is such a fragile eyelid, which measures less than 1 mm in thickness, balance struck between form and function as that in eye- retains a smooth delicate texture until it extends beyond lid modification. Owing to the delicate nature of eyelid the lateral orbital rim, where it gradually becomes thicker structural composition and the vital role the eyelids serve and coarser. The eyelid skin, which is essentially devoid of in protecting the visual system, iatrogenic alterations in a subcutaneous fat layer, is interconnected to the under- eyelid anatomy must be made with care, precision, and lying musculus orbicularis oculi by fine connective tissue thoughtful consideration of existing soft tissue structures. attachments in the skin’s pretarsal and preseptal zones. A brief anatomical review is necessary to highlight some of these salient points. With the eyes in primary position, the lower lid should Musculature be well apposed to the globe, with its lid margin roughly The orbicularis oculi muscle can be divided into a darker tangent to the inferior limbus and the orientation of its re- and thicker orbital portion (voluntary) and a thinner and spective palpebral fissure slanted slightly obliquely upward lighter palpebral portion (voluntary and involuntary). The from medial to lateral (occidental norm). An inferior palpe- palpebral portion can be further subdivided into preseptal bral sulcus (lower eyelid crease) is usually identified ϳ5 to and pretarsal components (Fig. -
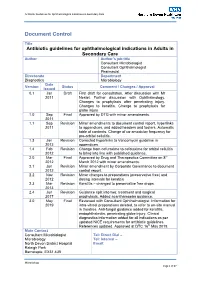
Antibiotic Guidelines for Ophthalmology V1.8 290413 Issue Date Review Date Review Cycle May 2019 May 2022 Three Years Consulted with the Following Stakeholders
Antibiotic Guidelines for Ophthalmological Indications in Secondary Care Document Control Title Antibiotic guidelines for ophthalmological indications in Adults in Secondary Care Author Author’s job title Consultant Microbiologist Consultant Ophthalmologist Pharmacist Directorate Department Diagnostics Microbiology Date Version Status Comment / Changes / Approval Issued 0.1 Jan Draft First draft for consultation. After discussion with Mr 2011 Nestel. Further discussion with Ophthalmology. Changes to prophylaxis after penetrating injury. Changes to keratitis. Change to prophylaxis for globe injury 1.0 Sep Final Approved by DTG with minor amendments. 2011 1.1 Sep Revision Minor amendments to document control report, hyperlinks 2011 to appendices, and added headers and footers. Automatic table of contents. Change of co-amoxiclav frequency for pre-orbital cellulitis. 1.3 Jan Revision Corrected hyperlinks to Vancomycin guideline in 2012 appendices. 1.4 Feb Revision Change from cefuroxime to cefotaxime for orbital cellulitis 2012 to bring into line with published guidance. 2.0 Mar Final Approved by Drug and Therapeutics Committee on 8th 2012 March 2012 with minor amendments. 2.1 Jun Revision Minor amendment by Corporate Governance to document 2012 control report. 2.2 Nov Revision Minor changes to preparations (preservative free) and 2012 dosing intervals for keratitis 2.3 Mar Revision Keratitis – changed to preservative free drops. 2013 2.4 Jun Revision Guidance split into two: treatment and surgical 2017 prophylaxis. Added acanthamoeba guidance. 3.0 May Final Reviewed with Consultant Ophthalmologist. Information for 2019 intra-vitreal preparations deleted, to refer to on-site manual in theatres. Anti-fungal guidance added for keratitis, endophthalmitis, penetrating globe injury. Clinical diagnostics information added for all indications as per updated NICE requirements for antibiotic guidelines. -

Deep Brain Stimulation for Parkinson's Disease
Functional Neurosurgical Therapies for Movement Disorders and Epilepsy Seth F Oliveria, MD PhD The Oregon Clinic Neurosurgery Director of Functional Neurosurgery: Providence Brain and Spine Institute Portland, OR Providence St Vincent’s Providence Portland “Functional Neurosurgery” The use of ultra-precise neurosurgical techniques to surgically modulate abnormal physiologic processes in the nervous system Movement disorders Epilepsy Pain disorders Psychiatric disorders “Functional Neurosurgery” The use of ultra-precise neurosurgical techniques to surgically modulate abnormal physiologic processes in the nervous system Movement disorders Epilepsy Pain disorders Psychiatric disorders *Therapy is tailored to each individual patient Deep brain stimulation (DBS) • DBS is a surgical procedure used to treat many of the debilitating symptoms of Parkinson’s disease and other movement disorders • DBS is non-ablative: it is reversible and adjustable • It is currently indicated for movement disorders that are refractory to medical therapy Parkinson’s Disease • A complex, progressive degenerative neurologic disorder that causes loss of control over body movements • Primary motor symptoms: Tremor Rigidity Akinesia/bradykinesia Postural instability Parkinson’s Disease • Motor symptoms arise when the substantia nigra degenerates and DA neurons die • Medical treatment: replace dopamine—very effective • BUT, there are limitations… Increasing dosages Increasing side effects • Dyskinesia • Hallucinations • Wearing off • Unpredictability Parkinson’s Disease -

7. Headache Attributed to Non-Vascular Intracranial Disorder
Classification and Diagnosis of Secondary Headaches, Part II- Altered Intracerebral Pressure, Neoplasms, and Infections Lawrence C. Newman, M.D. Director, The Headache Institute Roosevelt Hospital Center New York, N.Y. 7. Headache7. Headache attributed attributed to to non-vascularnon-vascular intracranial intracranial disorder 7.1 Headache attributed to high cerebrospinal fluid pressure 7.2 Headache attributed to low cerebrospinaldisorder fluid pressure 7.3 Headache attributed to non-infectious inflammatory disease 7.4 Headache attributed to intracranial neoplasm 7.5 Headache attributed to intrathecal injection 7.6 Headache attributed to epileptic seizure 7.7 Headache attributed to Chiari malformation type I 7.8 Syndrome of transient Headache and Neurological Deficits with cerebrospinal fluid Lymphocytosis (HaNDL) 7.9 Headache attributed to other non-vascular intracranial disorder ICHD-II. Cephalalgia 2004; 24 (Suppl 1) ©International Headache Society 2003/4 Headaches attributed to alterations in CSF pressure: • Headache frequently accompanies alteration of CSF pressure, either high or low • Pressure alterations may be the result of disruptions of CSF production, flow, or absorption • Major source of CSF is choroid plexus; some also formed extra-choroidal • CSF absorbed primarily in pacchionian granulations arachnoid villi and vessels of subarachnoid space over hemispheres ® American Headache Society Increased Intracranial Pressure: Secondary Causes • Venous sinus occlusion • Medications (naladixic • Radical neck dissection acid,danocrine,