Thesis Reference
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Walnut Polyphenol
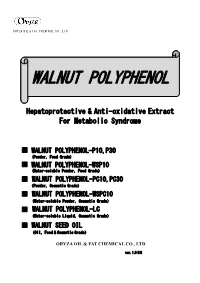
ORYZA OIL & FAT CHEMICAL CO., L TD. WALNUT POLYPHENOL Hepatoprotective & Anti-oxidative Extract For Metabolic Syndrome ■ WALNUT POLYPHENOL-P10,P30 (Powder,Food Grade) ■ WALNUT POLYPHENOL-WSP10 (Water-soluble Powder,Food Grade) ■ WALNUT POLYPHENOL-PC10,PC30 (Powder,Cosmetic Grade) ■ WALNUT POLYPHENOL-WSPC10 (Water-soluble Powder,Cosmetic Grade) ■ WALNUT POLYPHENOL-LC (Water-soluble Liquid,Cosmetic Grade) ■ WALNUT SEED OIL (Oil,Food & Cosmetic Grade) ORYZA OIL & FAT CHEMICAL CO., LTD ver. 1.0 HS WALNUT POLYPHENOL ver.1.0 HS WALNUT POLYPHENOL Hepatoprotective & Anti-oxidative Extract For Metabolic Syndrome 1. Introduction Recently, there is an increased awareness on metabolic syndrome – a condition characterized by a group of metabolic risk factors in one person. They include abdominal obesity, atherogenic dyslipidemia, elevated blood pressure, insulin resistance, prothrombotic state & proinflammatory state. The dominant underlying risk factors appear to be abdominal obesity and insulin resistance. In addition, non-alcoholic fatty liver disease (NAFLD) is the most commonly associated “liver” manifestation of metabolic syndrome which can progress to advance liver disease (e.g. cirrhosis) with associated morbidity and mortality. Lifestyle therapies such as weight loss significantly improve all aspects of metabolic syndrome, as well as reducing progression of NAFLD and cardiovascular mortality. Walnut (Juglans regia L. seed) is one the most popular nuts consumed in the world. It is loaded in polyunsaturated fatty acids – linoleic acid (LA), oleic acid and α-linolenic acid (ALA), an ω3 fatty acid. It has been used since ancient times and epidemiological studies have revealed that incorporating walnuts in a healthy diet reduces the risk of cardiovascular diseases. Recent investigations reported that walnut diet improves the function of blood vessels and lower serum cholesterol. -

Antibacterial, Antioxidant, and Anticholinesterase Activities of Plant Seed Extracts from Brazilian Semiarid Region
Hindawi Publishing Corporation BioMed Research International Volume 2013, Article ID 510736, 9 pages http://dx.doi.org/10.1155/2013/510736 Research Article Antibacterial, Antioxidant, and Anticholinesterase Activities of Plant Seed Extracts from Brazilian Semiarid Region Davi Felipe Farias,1 Terezinha Maria Souza,2 Martônio Ponte Viana,1 Bruno Marques Soares,3 Arcelina Pacheco Cunha,4 Ilka Maria Vasconcelos,1 Nágila Maria Pontes Silva Ricardo,4 Paulo Michel Pinheiro Ferreira,5,6 Vânia Maria Maciel Melo,7 and Ana Fontenele Urano Carvalho7 1 Departamento de Bioqu´ımica e Biologia Molecular, Universidade Federal do Ceara,´ 60440-970 Fortaleza, CE, Brazil 2 Netherlands Toxicogenomics Centre, Maastricht University, Universiteitssingel 50, 6229ER Maastricht, The Netherlands 3 Departamento de Fisiologia e Farmacologia, Faculdade de Medicina, Universidade Federal do Ceara,´ 60430-270 Fortaleza, CE, Brazil 4 Departamento de Qu´ımica Organicaˆ e Inorganica,ˆ Universidade Federal do Ceara,´ 60440-970 Fortaleza, CE, Brazil 5 Departamento de Cienciasˆ Biologicas,´ Campus Senador Helv´ıdio Nunes de Barros, Universidade Federal do Piau´ı, 64600-000 Picos, PI, Brazil 6 Programa de Pos-Graduac´ ¸ao˜ em Cienciasˆ Farmaceuticas,ˆ Universidade Federal do Piau´ı, Avenida Universitaria,´ s/n, 64049-550 Teresina, PI, Brazil 7 Departamento de Biologia, Universidade Federal do Ceara,´ Campus do Pici, 60451-970 Fortaleza, CE, Brazil Correspondence should be addressed to Ana Fontenele Urano Carvalho; [email protected] Received 9 July 2013; Accepted 28 October 2013 Academic Editor: Kazim Husain Copyright © 2013 Davi Felipe Farias et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Anticancer Effects of NSC‑631570 (Ukrain) in Head and Neck Cancer Cells: in Vitro Analysis of Growth, Invasion, Angiogenesis and Gene Expression
282 ONCOLOGY REPORTS 43: 282-295, 2020 Anticancer effects of NSC‑631570 (Ukrain) in head and neck cancer cells: In vitro analysis of growth, invasion, angiogenesis and gene expression RUTH HERRMANN1, JOSEPH SKAF2, JEANETTE ROLLER1, CHRISTINE POLEDNIK1, ULRIKE HOLZGRABE2 and MARIANNE SCHMIDT1 1Department of Otorhinolaryngology, University of Würzburg, D-97080 Würzburg; 2Institute of Pharmacy and Food Chemistry, University of Würzburg, D-97074 Würzburg, Germany Received September 17, 2018; Accepted September 30, 2019 DOI: 10.3892/or.2019.7416 Abstract. NSC-631570 (Ukrain) is an aqueous extract of laminin). Microarray analysis revealed the downregulation of Chelidonium majus, a herbaceous perennial plant, one of two genes encoding key regulators, including EGFR, AKT2, JAK1, species in the genus Chelidonium, which has been demonstrated STAT3 and ß-catenin (CTNNB1), all of which are involved in to selectively kill tumor cells without affecting non-malignant cell proliferation, migration, angiogenesis, apoptosis as well as cells. In the present study, the components of NSC-631570 the radiation- and chemo-resistance of HNSCC. The strongest were examined by combined liquid chromatography/mass upregulation occurred for cytochrome P450 1A1 (CYP1A1) spectroscopy (LC-MS) and the effects of NSC-631570 on and 1B1 (CYP1B1), involved in the metabolism of xenobiotics. HNSCC cell lines, as well as primary cells, were analyzed Upregulation of CYP1A1 was at least partially caused by chel- with respect to growth, apoptosis, invasion, angiogenesis erythrine and allocryptopine, as shown by RT-qPCR in two and gene expression. LC-MS identified chelerythrine and HNSCC cell lines. In addition, NSC-631570 showed a high allocryptopine as the major alkaloids of the extract. -

Argemone Mexicana
Argemone mexicana General description Scientific Name with Author Argemone mexicana L. Synonyms Argemone leiocarpa Greene; Argemone ochroleuca Sweet; Echtrus trivialis Lour.; Echtrus mexicanus (L.) Nieuwl.; Argemone vulgaris Spach; Argemone versicolor Salisb.; Argemone spinosa Moench; Argemone sexvalis Stokes; Argemone mucronata Dum. Cours. ex Steud.; Argemone mexicana var. typica Prain; Argemone mexicana var. parviflora Kuntze; Argemone mexicana var. ochroleuca (Sweet) Lindl.; Argemone mexicana var. lutea Kuntze; Argemone mexicana fo. leiocarpa (Greene) G.B. Ownbey (Pires, 2009). Family Papaveraceae Vernacular Names Mexican poppy, prickly poppy, yellow thistle, Mexican thistle (En). Argémone, pavot épineux, pavot du Mexique, tache de l’œil, chardon du pays (Fr) (Bosch, 2008) Botanical Description Argemone mexicana is an annual herb, growing up to 150 cm with a slightly branched tap root. Its stem is branched and usually extremely prickly. It exudes a yellow juice when cut. It has showy yellow flowers. Leaves are thistle-like and alternate, without leaf stalks (petioles), toothed (serrate) and the margins are spiny. The grey-white veins stand out against the bluish-green upper leaf surface. The stem is oblong in cross-section. Flowers are at the tips of the branches (are terminal) and solitary, yellow and of 2.5-5 cm diameter. Fruit is a prickly oblong or egg-shaped (ovoid) capsule. Seeds are very numerous, nearly spherical, covered in a fine network of veins, brownish black and about 1 m m in diameter (Nacoulma, 1996; Bosch, 2008). 1 MEAMP – Appear Project – 75 September 2012 – August 2014 Photo LABIOCA 1. Argemone mexicana Origin and Distribution Argemone mexicana is native in Mexico and the West Indies, but has become pantropical after accidental introduction or introduction as an ornamental. -

Classification Et Influences Des Polyphénols Du Boisde Chêne Sur La Qualité Sensorielle Des Vins (Application Du Procédé Oakscan®) Julien Michel
Classification et influences des polyphénols du boisde chêne sur la qualité sensorielle des vins (Application du procédé OakScan®) Julien Michel To cite this version: Julien Michel. Classification et influences des polyphénols du bois de chêne sur la qualité sensorielle des vins (Application du procédé OakScan®). Ingénierie des aliments. Université de Bordeaux Ségalen (Bordeaux 2), 2012. Français. tel-02811201 HAL Id: tel-02811201 https://hal.inrae.fr/tel-02811201 Submitted on 6 Jun 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Université Bordeaux Segalen Année 2012 Thèse n° 1989 THESE pour le DOCTORAT DE L’UNIVERSITE BORDEAUX 2 Mention : Sciences, Technologie, Santé Option : Œnologie Présentée et soutenue publiquement le 14 décembre 2012 par MICHEL Julien Né le 8 mars 1984 à Bordeaux, France ****************************** Classification et influences des polyphénols du bois de chêne sur la qualité sensorielle des vins (Application du procédé Oakscan®) ****************************** Membres du Jury M. F. ZAMORA, Professeur, Universitat Rovira i Virgili ......................................... Rapporteur M.J. RICARDO DA SILVA, Professeur, Universidade de Lisbonne ........................ Rapporteur M. B. CHARRIER, Professeur, Université de Pau ..................................................... Examinateur M. M. JOURDES, Maître de Conférences, Université Bordeaux Segalen ................. Examinateur M. P.L. -
Information to Users
INFORMATION TO USERS This manuscript has been reproduced from the microfilm master. UMI films the text directly from the original or copy submitted. Thus, some thesis and dissertation copies are in typewriter face, while others may be from any type of computer printer. The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleedthrough, substandard margins, and improper alignment can adversely afreet reproduction. In the unlikely event that the author did not send UMI a complete manuscript and there are missing pages, these will be noted. Also, if unauthorized copyright material had to be removed, a note will indicate the deletion. Oversize materials (e.g., maps, drawings, charts) are reproduced by sectioning the original, beginning at the upper left-hand corner and continuing from left to right in equal sections with small overlaps. Each original is also photographed in one exposure and is included in reduced form at the back of the book. Photographs included in the original manuscript have been reproduced xerographically in this copy. Higher quality 6" x 9" black and white photographic prints are available for any photographs or illustrations appearing in this copy for an additional charge. Contact UMI directly to order. University Microfilms International A Bell & Howell Information Company 3 0 0 North Z eeb Road, Ann Arbor, Ml 4 8 1 06-1346 USA 313/761-4700 800/521-0600 Order Number 9130509 Allozyme variation and evolution inPolygonella (Polygonaceae) Lewis, Paul Ollin, Ph.D. The Ohio State University, 1991 Copyright ©1991 by Lewis, Paul Ollin. -

Universidade Federal Do Rio De Janeiro Kim Ohanna
UNIVERSIDADE FEDERAL DO RIO DE JANEIRO KIM OHANNA PIMENTA INADA EFFECT OF TECHNOLOGICAL PROCESSES ON PHENOLIC COMPOUNDS CONTENTS OF JABUTICABA (MYRCIARIA JABOTICABA) PEEL AND SEED AND INVESTIGATION OF THEIR ELLAGITANNINS METABOLISM IN HUMANS. RIO DE JANEIRO 2018 Kim Ohanna Pimenta Inada EFFECT OF TECHNOLOGICAL PROCESSES ON PHENOLIC COMPOUNDS CONTENTS OF JABUTICABA (MYRCIARIA JABOTICABA) PEEL AND SEED AND INVESTIGATION OF THEIR ELLAGITANNINS METABOLISM IN HUMANS. Tese de Doutorado apresentada ao Programa de Pós-Graduação em Ciências de Alimentos, Universidade Federal do Rio de Janeiro, como requisito parcial à obtenção do título de Doutor em Ciências de Alimentos Orientadores: Profa. Dra. Mariana Costa Monteiro Prof. Dr. Daniel Perrone Moreira RIO DE JANEIRO 2018 DEDICATION À minha família e às pessoas maravilhosas que apareceram na minha vida. ACKNOWLEDGMENTS Primeiramente, gostaria de agradecer a Deus por ter me dado forças para não desistir e por ter colocado na minha vida “pessoas-anjo”, que me ajudaram e me apoiaram até nos momentos em que eu achava que ia dar tudo errado. Aos meus pais Beth e Miti. Eles não mediram esforços para que eu pudesse receber uma boa educação e para que eu fosse feliz. Logo no início da graduação, a situação financeira ficou bem apertada, mas eles continuaram fazendo de tudo para me ajudar. Foram milhares de favores prestados, marmitas e caronas. Meu pai diz que fez anos de curso de inglês e espanhol, porque passou anos acordando cedo no sábado só para me levar no curso que eu fazia no Fundão. Tinha dia que eu saía do curso morta de fome e quando eu entrava no carro, tinha uma marmita com almoço, com direito até a garrafa de suco. -

(Diptera: Cecidomyiidae) from Subterranean Stem Galls of Licania Michauxii (Chrysobalanaceae) in Florida
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln USDA Systematic Entomology Laboratory Entomology Collections, Miscellaneous 1996 A New Species of Gall Midge (Diptera: Cecidomyiidae) from Subterranean Stem Galls of Licania Michauxii (Chrysobalanaceae) in Florida Raymond Gagne ARS, USDA Kenneth Hibbard Florida Department of Agriculture and Consumer Services Fort Pierce, FL Follow this and additional works at: https://digitalcommons.unl.edu/systentomologyusda Part of the Entomology Commons Gagne, Raymond and Hibbard, Kenneth, "A New Species of Gall Midge (Diptera: Cecidomyiidae) from Subterranean Stem Galls of Licania Michauxii (Chrysobalanaceae) in Florida" (1996). USDA Systematic Entomology Laboratory. 13. https://digitalcommons.unl.edu/systentomologyusda/13 This Article is brought to you for free and open access by the Entomology Collections, Miscellaneous at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in USDA Systematic Entomology Laboratory by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. 428 Florida Entomologist 79(3) September, 1996 A NEW SPECIES OF GALL MIDGE (DIPTERA: CECIDOMYIIDAE) FROM SUBTERRANEAN STEM GALLS OF LICANIA MICHAUXII (CHRYSOBALANACEAE) IN FLORIDA RAYMOND J. GAGNÉ1 AND KENNETH L. HIBBARD2 1Systematic Entomology Laboratory, PSI, ARS, USDA c/o National Museum of Natural History MRC-168 Washington, D. C. 20560 2Division of Plant Industry Florida Department of Agriculture and Consumer Services Fort Pierce, FL 34945-3045 ABSTRACT A new species of gall midge is described from subterranean stem galls on Licania michauxii Prance from Florida. The gall former is a new species of Lopesia and the first record of this genus in North America. The limits of Lopesia, a genus previously recorded only from South America and Africa, are enlarged to accept the new species. -

Flora of the Carolinas, Virginia, and Georgia, Working Draft of 17 March 2004 -- BIBLIOGRAPHY
Flora of the Carolinas, Virginia, and Georgia, Working Draft of 17 March 2004 -- BIBLIOGRAPHY BIBLIOGRAPHY Ackerfield, J., and J. Wen. 2002. A morphometric analysis of Hedera L. (the ivy genus, Araliaceae) and its taxonomic implications. Adansonia 24: 197-212. Adams, P. 1961. Observations on the Sagittaria subulata complex. Rhodora 63: 247-265. Adams, R.M. II, and W.J. Dress. 1982. Nodding Lilium species of eastern North America (Liliaceae). Baileya 21: 165-188. Adams, R.P. 1986. Geographic variation in Juniperus silicicola and J. virginiana of the Southeastern United States: multivariant analyses of morphology and terpenoids. Taxon 35: 31-75. ------. 1995. Revisionary study of Caribbean species of Juniperus (Cupressaceae). Phytologia 78: 134-150. ------, and T. Demeke. 1993. Systematic relationships in Juniperus based on random amplified polymorphic DNAs (RAPDs). Taxon 42: 553-571. Adams, W.P. 1957. A revision of the genus Ascyrum (Hypericaceae). Rhodora 59: 73-95. ------. 1962. Studies in the Guttiferae. I. A synopsis of Hypericum section Myriandra. Contr. Gray Herbarium Harv. 182: 1-51. ------, and N.K.B. Robson. 1961. A re-evaluation of the generic status of Ascyrum and Crookea (Guttiferae). Rhodora 63: 10-16. Adams, W.P. 1973. Clusiaceae of the southeastern United States. J. Elisha Mitchell Sci. Soc. 89: 62-71. Adler, L. 1999. Polygonum perfoliatum (mile-a-minute weed). Chinquapin 7: 4. Aedo, C., J.J. Aldasoro, and C. Navarro. 1998. Taxonomic revision of Geranium sections Batrachioidea and Divaricata (Geraniaceae). Ann. Missouri Bot. Gard. 85: 594-630. Affolter, J.M. 1985. A monograph of the genus Lilaeopsis (Umbelliferae). Systematic Bot. Monographs 6. Ahles, H.E., and A.E. -

Dr. Duke's Phytochemical and Ethnobotanical Databases Chemicals Found in Papaver Somniferum
Dr. Duke's Phytochemical and Ethnobotanical Databases Chemicals found in Papaver somniferum Activities Count Chemical Plant Part Low PPM High PPM StdDev Refernce Citation 0 (+)-LAUDANIDINE Fruit -- 0 (+)-RETICULINE Fruit -- 0 (+)-RETICULINE Latex Exudate -- 0 (-)-ALPHA-NARCOTINE Inflorescence -- 0 (-)-NARCOTOLINE Inflorescence -- 0 (-)-SCOULERINE Latex Exudate -- 0 (-)-SCOULERINE Plant -- 0 10-HYDROXYCODEINE Latex Exudate -- 0 10-NONACOSANOL Latex Exudate Chemical Constituents of Oriental Herbs (3 diff. books) 0 13-OXOCRYPTOPINE Plant -- 0 16-HYDROXYTHEBAINE Plant -- 0 20-HYDROXY- Fruit 36.0 -- TRICOSANYLCYCLOHEXA NE 0 4-HYDROXY-BENZOIC- Pericarp -- ACID 0 4-METHYL-NONACOSANE Fruit 3.2 -- 0 5'-O- Plant -- DEMETHYLNARCOTINE 0 5-HYDROXY-3,7- Latex Exudate -- DIMETHOXYPHENANTHRE NE 0 6- Plant -- ACTEONLYDIHYDROSANG UINARINE 0 6-METHYL-CODEINE Plant Father Nature's Farmacy: The aggregate of all these three-letter citations. 0 6-METHYL-CODEINE Fruit -- 0 ACONITASE Latex Exudate -- 32 AESCULETIN Pericarp -- 3 ALANINE Seed 11780.0 12637.0 0.5273634907250652 -- Activities Count Chemical Plant Part Low PPM High PPM StdDev Refernce Citation 0 ALKALOIDS Latex Exudate 50000.0 250000.0 ANON. 1948-1976. The Wealth of India raw materials. Publications and Information Directorate, CSIR, New Delhi. 11 volumes. 5 ALLOCRYPTOPINE Plant Father Nature's Farmacy: The aggregate of all these three-letter citations. 15 ALPHA-LINOLENIC-ACID Seed 1400.0 5564.0 -0.22115561650586155 -- 2 ALPHA-NARCOTINE Plant Jeffery B. Harborne and H. Baxter, eds. 1983. Phytochemical Dictionary. A Handbook of Bioactive Compounds from Plants. Taylor & Frost, London. 791 pp. 17 APOMORPHINE Plant Father Nature's Farmacy: The aggregate of all these three-letter citations. 0 APOREINE Fruit -- 0 ARABINOSE Fruit ANON. -

Fumaria Parviflora Lam. (Fumitory): a Traditional Herbal Medicine with Modern Evidence
Asian Journal of Pharmacy and Pharmacology 2017; 3(6): 200-207 200 Review Article Fumaria parviflora Lam. (Fumitory): A traditional herbal medicine with modern evidence Suresh Kumar* 1, 2, Anil Kumar Sharma 3 , Anjoo Kamboj 4 1Lord Shiva College of Pharmacy Sirsa, Haryana, India-125055 2Research Scholar, Department of Pharmacy, IK Gujral Punjab Technical University, Jalandhar, Punjab, India-144001 3Formerly Director and Principal in CT Institute of Pharmaceutical Sciences, Jalandhar, Punjab, India-144020 4Chandigarh College of Pharmacy, Landran, Mohali, Punjab, India-140110 Received: 2 November 2017 Revised: 4 December 2017 Accepted: 5 December 2017 Abstract Fumaria parviflora is an important medicinal herb which is used in various traditional medicines to cure many diseases. The herbal extracts have been reported to possess anti-inflammatory, antispasmodic, antidiarrheal, bronchodilator, hypoglycemic, anthelmintic, laxative, antiprotozoal, dermatological diseases, enhance male fertility and antinociceptive effect. Their biological activity is primarily associated with the presence of alkaloids such as protopine, cryptopine, parfumine, berberine, oxyberberine, fumarine, protocatechuic acid and caffeic acid. Some other bioactive are fatty acids, volatile oils and sesquterpenoids and aromatic hydrocarbons in plant. The present review is therefore, an effort to give a detailed survey of the literature on its botany, phytochemistry and biological activities of Fumaria parviflora, chronologically. Keywords: Fumaria parviflora, Protopine, fumitory, -

Redalyc.Identification of Isoquinoline Alkaloids from Berberis Microphylla
Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas ISSN: 0717-7917 [email protected] Universidad de Santiago de Chile Chile MANOSALVA, Loreto; MUTIS, Ana; DÍAZ, Juan; URZÚA, Alejandro; FAJARDO, Víctor; QUIROZ, Andrés Identification of isoquinoline alkaloids from Berberis microphylla by HPLC ESI-MS/MS Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas, vol. 13, núm. 4, 2014, pp. 324-335 Universidad de Santiago de Chile Santiago, Chile Available in: http://www.redalyc.org/articulo.oa?id=85631435002 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative © 2014 Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas 13 (4): 324 - 335 ISSN 0717 7917 www.blacpma.usach.cl Artículo Original | Original Article In memorian Professor Luis Astudillo, Universidad de Talca, Chile Identification of isoquinoline alkaloids from Berberis microphylla by HPLC ESI-MS/MS [Identificación de alcaloides isoquinolínicos en Berberis microphylla G. Forst mediante CLAE IES-MS/MS] Loreto MANOSALVA1, Ana MUTIS2, Juan DÍAZ3, Alejandro URZÚA4, Víctor FAJARDO5 & Andrés QUIROZ2 1Doctorado en Ciencias de Recursos Naturales; 2Laboratorio de Ecología Química, Departamento de Ciencias Químicas y Recursos Naturales; 3Laboratory of Mass Spectrometry, Scientific and Technological Bioresource Nucleus (Bioren), Universidad de La Frontera, Temuco, Chile 4Laboratory of Chemical Ecology, Department of Environmental Sciences, Faculty of Chemistry and Biology, Universidad de Santiago de Chile 5Chile Laboratorio de Productos Naturales, Universidad de Magallanes, Punta Arenas, Chile Contactos | Contacts: Andrés QUIROZ - E-mail address: [email protected] Abstract: Berberis microphylla (G.