Idiopathic Hypogonadotropic Hypogonadism Caused by Inactivating Mutations in SRA1 Leman Damla Kotan1, Charlton Cooper2, Şükran Darcan3, Ian M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anti- DDX17 Antibody
anti- DDX17 antibody Product Information Catalog No.: FNab02296 Size: 100μg Form: liquid Purification: Immunogen affinity purified Purity: ≥95% as determined by SDS-PAGE Host: Rabbit Clonality: polyclonal Clone ID: None IsoType: IgG Storage: PBS with 0.02% sodium azide and 50% glycerol pH 7.3, -20℃ for 12 months (Avoid repeated freeze / thaw cycles.) Background RNA-dependent ATPase activity. Involved in transcriptional regulation. Transcriptional coactivator for estrogen receptor ESR1. Increases ESR1 AF-1 domain-mediated transactivation. Synergizes with DDX5 and SRA1 RNA to activate MYOD1 transcriptional activity and probably involved in skeletal muscle differentiation. Required for zinc-finger antiviral protein ZC3HAV1- mediated mRNA degradation. Immunogen information Immunogen: DEAD(Asp-Glu-Ala-Asp) box polypeptide 17 Synonyms: DDX17, DEAD box protein 17, DEAD box protein p72, P72, RH70, RNA dependent helicase p72 Observed MW: 72 kDa, 80 kDa Uniprot ID : Q92841 Application Reactivity: Human, Mouse, Rat Tested Application: ELISA, IHC, IF, WB, IP 1 Wuhan Fine Biotech Co., Ltd. B9 Bld, High-Tech Medical Devices Park, No. 818 Gaoxin Ave.East Lake High-Tech Development Zone.Wuhan, Hubei, China(430206) Tel :( 0086)027-87384275 Fax: (0086)027-87800889 www.fn-test.com Recommended dilution: WB: 1:500-1:2000; IP: 1:500-1:2000; IHC: 1:500-1:2000; IF: 1:10-1:100 Image: Immunohistochemistry of paraffin-embedded human kidney using FNab02296(DDX17 antibody) at dilution of 1:100 Immunofluorescent analysis of Hela cells, using DDX17 antibody FNab02296 at 1:25 dilution and Rhodamine-labeled goat anti-rabbit IgG (red). IP Result of anti-DDX17,P72 (IP: FNab02296, 4ug; Detection: FNab02296 1:1000) with mouse brain tissue lysate 3000ug. -

1 Supporting Information for a Microrna Network Regulates
Supporting Information for A microRNA Network Regulates Expression and Biosynthesis of CFTR and CFTR-ΔF508 Shyam Ramachandrana,b, Philip H. Karpc, Peng Jiangc, Lynda S. Ostedgaardc, Amy E. Walza, John T. Fishere, Shaf Keshavjeeh, Kim A. Lennoxi, Ashley M. Jacobii, Scott D. Rosei, Mark A. Behlkei, Michael J. Welshb,c,d,g, Yi Xingb,c,f, Paul B. McCray Jr.a,b,c Author Affiliations: Department of Pediatricsa, Interdisciplinary Program in Geneticsb, Departments of Internal Medicinec, Molecular Physiology and Biophysicsd, Anatomy and Cell Biologye, Biomedical Engineeringf, Howard Hughes Medical Instituteg, Carver College of Medicine, University of Iowa, Iowa City, IA-52242 Division of Thoracic Surgeryh, Toronto General Hospital, University Health Network, University of Toronto, Toronto, Canada-M5G 2C4 Integrated DNA Technologiesi, Coralville, IA-52241 To whom correspondence should be addressed: Email: [email protected] (M.J.W.); yi- [email protected] (Y.X.); Email: [email protected] (P.B.M.) This PDF file includes: Materials and Methods References Fig. S1. miR-138 regulates SIN3A in a dose-dependent and site-specific manner. Fig. S2. miR-138 regulates endogenous SIN3A protein expression. Fig. S3. miR-138 regulates endogenous CFTR protein expression in Calu-3 cells. Fig. S4. miR-138 regulates endogenous CFTR protein expression in primary human airway epithelia. Fig. S5. miR-138 regulates CFTR expression in HeLa cells. Fig. S6. miR-138 regulates CFTR expression in HEK293T cells. Fig. S7. HeLa cells exhibit CFTR channel activity. Fig. S8. miR-138 improves CFTR processing. Fig. S9. miR-138 improves CFTR-ΔF508 processing. Fig. S10. SIN3A inhibition yields partial rescue of Cl- transport in CF epithelia. -

Mice Fed Rapamycin Have an Increase in Lifespan Associated with Major Changes in the Liver Transcriptome
Mice Fed Rapamycin Have an Increase in Lifespan Associated with Major Changes in the Liver Transcriptome Fok WC, Chen Y, Bokov A, Zhang Y, Salmon AB, et al. (2014) Mice Fed Rapamycin Have an Increase in Lifespan Associated with Major Changes in the Liver Transcriptome. PLoS ONE 9(1): e83988. doi:10.1371/journal.pone.0083988 10.1371/journal.pone.0083988 Public Library of Science Version of Record http://hdl.handle.net/1957/47220 http://cdss.library.oregonstate.edu/sa-termsofuse Mice Fed Rapamycin Have an Increase in Lifespan Associated with Major Changes in the Liver Transcriptome Wilson C. Fok1, Yidong Chen3,4,5, Alex Bokov2,3, Yiqiang Zhang2,6, Adam B. Salmon2,7,11, Vivian Diaz2, Martin Javors8, William H. Wood, 3rd9, Yongqing Zhang9, Kevin G. Becker9, Viviana I. Pe´rez10, Arlan Richardson1,2,11* 1 Department of Cellular and Structural Biology, The University of Texas Health Science Center at San Antonio, San Antonio, Texas, United States of America, 2 Barshop Institute for Longevity and Aging Studies, The University of Texas Health Science Center at San Antonio, San Antonio, Texas, United States of America, 3 Department of Epidemiology & Biostatistics, The University of Texas Health Science Center at San Antonio, San Antonio, Texas, United States of America, 4 Greehey Children’s Cancer Research Institute, The University of Texas Health Science Center at San Antonio, San Antonio, Texas, United States of America, 5 Cancer Therapy and Research Center, The University of Texas Health Science Center at San Antonio, San Antonio, Texas, United -

SPEN Protein Expression and Interactions with Chromatin in Mouse Testicular Cells
156 3 REPRODUCTIONRESEARCH SPEN protein expression and interactions with chromatin in mouse testicular cells Joanna Korfanty1, Tomasz Stokowy2, Marek Chadalski1, Agnieszka Toma-Jonik1, Natalia Vydra1, Piotr Widłak1, Bartosz Wojtaś3, Bartłomiej Gielniewski3 and Wieslawa Widlak1 1Maria Sklodowska-Curie Institute – Oncology Center, Gliwice Branch, Gliwice, Poland, 2Department of Clinical Science, University of Bergen, Bergen, Norway and 3Laboratory of Molecular Neurobiology, Neurobiology Center, Nencki Institute of Experimental Biology, PAS, Warsaw, Poland Correspondence should be addressed to W Widlak; Email: [email protected] Abstract SPEN (spen family transcription repressor) is a nucleic acid-binding protein putatively involved in repression of gene expression. We hypothesized that SPEN could be involved in general downregulation of the transcription during the heat shock response in mouse spermatogenic cells through its interactions with chromatin. We documented predominant nuclear localization of the SPEN protein in spermatocytes and round spermatids, which was retained after heat shock. Moreover, the protein was excluded from the highly condensed chromatin. Chromatin immunoprecipitation experiments clearly indicated interactions of SPEN with chromatin in vivo. However, ChIP-Seq analyses did not reveal any strong specific peaks both in untreated and heat shocked cells, which might suggest dispersed localization of SPEN and/or its indirect binding to DNA. Using in situ proximity ligation assay we found close in vivo associations of SPEN with MTA1 (metastasis-associated 1), a member of the nucleosome remodeling complex with histone deacetylase activity, which might contribute to interactions of SPEN with chromatin. Reproduction (2018) 156 195–206 Introduction However, regulation of osteocalcin expression by SPEN depends on its interactions with other proteins. -
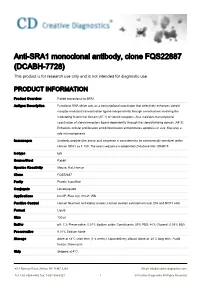
Anti-SRA1 Monoclonal Antibody, Clone FQS22887 (DCABH-7728) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-SRA1 monoclonal antibody, clone FQS22887 (DCABH-7728) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to SRA1 Antigen Description Functional RNA which acts as a transcriptional coactivator that selectively enhances steroid receptor-mediated transactivation ligand-independently through a mechanism involving the modulating N-terminal domain (AF-1) of steroid receptors. Also mediates transcriptional coactivation of steroid receptors ligand-dependently through the steroid-binding domain (AF-2). Enhances cellular proliferation and differentiation and promotes apoptosis in vivo. May play a role in tumorigenesis. Immunogen Synthetic peptide (the amino acid sequence is considered to be commercially sensitive) within Human SRA1 aa 1-100. The exact sequence is proprietary.Database link: Q9HD15 Isotype IgG Source/Host Rabbit Species Reactivity Mouse, Rat, Human Clone FQS22887 Purity Protein A purified Conjugate Unconjugated Applications ICC/IF, Flow Cyt, IHC-P, WB Positive Control Human fetal liver and kidney lysates; Human ovarian carcinoma tissue; 293 and MCF7 cells. Format Liquid Size 100 μl Buffer pH: 7.2; Preservative: 0.01% Sodium azide; Constituents: 59% PBS, 40% Glycerol, 0.05% BSA Preservative 0.01% Sodium Azide Storage Store at +4°C short term (1-2 weeks). Upon delivery aliquot. Store at -20°C long term. Avoid freeze / thaw cycle. Ship Shipped at 4°C. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 -

New Insights Into the Long Non-Coding RNA SRA
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Edinburgh Research Explorer Edinburgh Research Explorer New Insights Into the Long Non-coding RNA SRA Citation for published version: Sheng, L, Ye, L, Zhang, D, Cawthorn, W & Xu, B 2018, 'New Insights Into the Long Non-coding RNA SRA: Physiological Functions and Mechanisms of Action' Frontiers in Medicine, vol. 5, pp. 244. DOI: 10.3389/fmed.2018.00244 Digital Object Identifier (DOI): 10.3389/fmed.2018.00244 Link: Link to publication record in Edinburgh Research Explorer Document Version: Peer reviewed version Published In: Frontiers in Medicine General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 05. Apr. 2019 REVIEW published: 06 September 2018 doi: 10.3389/fmed.2018.00244 New Insights Into the Long Non-coding RNA SRA: Physiological Functions and Mechanisms of Action Liang Sheng 1,2, Lan Ye 3, Dong Zhang 3, William P. Cawthorn 4 and -

Gene Expression Barcode Values Reveal a Potential Link Between Parkinson's Disease and Gastric Cancer
University of Kentucky UKnowledge Internal Medicine Faculty Publications Internal Medicine 2-16-2021 Gene Expression Barcode Values Reveal a Potential Link between Parkinson's Disease and Gastric Cancer Suyan Tian First Hospital of Jilin University, China Shishun Zhao Jilin University, China Mingbo Tang First Hospital of Jilin University, China Chi Wang University of Kentucky, [email protected] Follow this and additional works at: https://uknowledge.uky.edu/internalmedicine_facpub Part of the Geriatrics Commons, Internal Medicine Commons, and the Oncology Commons Right click to open a feedback form in a new tab to let us know how this document benefits ou.y Repository Citation Tian, Suyan; Zhao, Shishun; Tang, Mingbo; and Wang, Chi, "Gene Expression Barcode Values Reveal a Potential Link between Parkinson's Disease and Gastric Cancer" (2021). Internal Medicine Faculty Publications. 231. https://uknowledge.uky.edu/internalmedicine_facpub/231 This Article is brought to you for free and open access by the Internal Medicine at UKnowledge. It has been accepted for inclusion in Internal Medicine Faculty Publications by an authorized administrator of UKnowledge. For more information, please contact [email protected]. Gene Expression Barcode Values Reveal a Potential Link between Parkinson's Disease and Gastric Cancer Digital Object Identifier (DOI) https://doi.org/10.18632/aging.202623 Notes/Citation Information Published by Aging, v. 13. © 2021 Tian et al. This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. This article is available at UKnowledge: https://uknowledge.uky.edu/internalmedicine_facpub/231 www.aging-us.com AGING 2021, Vol. -

Computational Analysis of Protein Function Within Complete Genomes
Computational Analysis of Protein Function within Complete Genomes Anton James Enright Wolfson College A dissertation submitted to the University of Cambridge for the degree of Doctor of Philosophy European Molecular Biology Laboratory, European Bioinformatics Institute, Wellcome Trust Genome Campus, Hinxton, Cambridge, CB10 1SD, United Kingdom. Email: [email protected] March 7, 2002 To My Parents and Kerstin This thesis is the result of my own work and includes nothing which is the outcome of work done in collaboration except where specifically indicated in the text. This thesis does not exceed the specified length limit of 300 pages as de- fined by the Biology Degree Committee. This thesis has been typeset in 12pt font using LATEX2ε accordingtothe specifications defined by the Board of Graduate Studies and the Biology Degree Committee. ii Computational Analysis of Protein Function within Complete Genomes Summary Anton James Enright March 7, 2002 Wolfson College Since the advent of complete genome sequencing, vast amounts of nucleotide and amino acid sequence data have been produced. These data need to be effectively analysed and verified so that they may be used for biologi- cal discovery. A significant proportion of predicted protein sequences from these complete genomes have poorly characterised or unknown functional annotations. This thesis describes a number of approaches which detail the computational analysis of amino acid sequences for the prediction and analy- sis of protein function within complete genomes. The first chapter is a short introduction to computational genome analysis while the second and third chapters describe how groups of related protein sequences (termed protein families) may be characterised using sequence clustering algorithms. -

N6-Methyladenosine (M6a)-Mediated Messenger RNA Signatures and the Tumor Immune Microenvironment Can Predict the Prognosis of Hepatocellular Carcinoma
59 Original Article Page 1 of 12 N6-methyladenosine (m6A)-mediated messenger RNA signatures and the tumor immune microenvironment can predict the prognosis of hepatocellular carcinoma Shen Shen1,2#, Jingya Yan1,2#, Yize Zhang1,2, Zihui Dong1,2, Jiyuan Xing1,2, Yuting He1 1Gene Hospital of Henan Province, Precision Medicine Center, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China; 2Department of Infectious Diseases, the First Affiliated Hospital of Zhengzhou University, Zhengzhou, China Contributions: (I) Conception and design: All authors; (II) Administrative support: Y He, S Shen; (III) Provision of study materials or patients: J Yan, Z Dong; (IV) Collection and assembly of data: Y Zhang; (V) Data analysis and interpretation: S Shen, J Xing; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. #These authors contributed equally to this work. Correspondence to: Yuting He. Gene Hospital of Henan Province, Precision Medicine Center, The First Affiliated Hospital of Zhengzhou University, No.1 Jianshe Road, Zhengzhou 450052, China. Email: [email protected]. Background: N6-methyladenosine (m6A)-mediated ribonucleic acid (RNA) methylation is considered to be the most significant and abundant epigenetic modification in eukaryotic cells, and plays an essential role in the carcinogenesis and molecular pathogenesis of hepatocellular carcinoma (HCC). However, the relationship between m6A regulation and immune cell infiltration of the tumor immune microenvironment (TIME) has not yet been clarified. We aimed to investigate the roles of m6A RNA gene regulators in HCC immune regulation and prognosis. Methods: The Cancer Genome Atlas (TCGA) database was used, and unsupervised clustering of 21 m6A regulators was performed based on differential gene expression. -

DDX5 Antibody Purified Mouse Monoclonal Antibody Catalog # Ao2243a
10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 DDX5 Antibody Purified Mouse Monoclonal Antibody Catalog # AO2243a Specification DDX5 Antibody - Product Information Application E, WB, FC, IHC Primary Accession P17844 Reactivity Human, Mouse, Monkey Host Mouse Clonality Monoclonal Isotype IgG2a Calculated MW 69.1kDa KDa Description DEAD box proteins, characterized by the conserved motif Asp-Glu-Ala-Asp (DEAD), are putative RNA helicases. They are implicated in a number of cellular processes involving alteration of RNA secondary structure, such as translation initiation, nuclear and mitochondrial splicing, and ribosome and spliceosome assembly. Based on their distribution patterns, some members of this family are believed to be involved in embryogenesis, spermatogenesis, and cellular growth and division. This gene encodes a DEAD box protein, which is a RNA-dependent ATPase, and also a proliferation-associated nuclear antigen, specifically reacting with the simian virus 40 tumor antigen. This gene consists of 13 exons, and alternatively spliced transcripts containing several intron sequences have been detected, but no isoforms encoded by these transcripts have been identified. Immunogen Purified recombinant fragment of human DDX5 (AA: 475-614) expressed in E. Coli. Formulation Purified antibody in PBS with 0.05% sodium azide DDX5 Antibody - Additional Information Gene ID 1655 Page 1/3 10320 Camino Santa Fe, Suite G San Diego, CA 92121 Tel: 858.875.1900 Fax: 858.622.0609 Other Names Probable ATP-dependent RNA helicase DDX5, 3.6.4.13, DEAD box protein 5, RNA helicase p68, DDX5, G17P1, HELR, HLR1 Dilution E~~1/10000 WB~~1/500 - 1/2000 FC~~1/200 - 1/400 IHC~~1/200 - 1/1000 Storage Maintain refrigerated at 2-8°C for up to 6 months. -

Fine Mapping of a Linkage Peak with Integration of Lipid Traits Identifies
Nolan et al. BMC Genetics 2012, 13:12 http://www.biomedcentral.com/1471-2156/13/12 RESEARCHARTICLE Open Access Fine mapping of a linkage peak with integration of lipid traits identifies novel coronary artery disease genes on chromosome 5 Daniel K Nolan1, Beth Sutton1, Carol Haynes1, Jessica Johnson1, Jacqueline Sebek1, Elaine Dowdy1, David Crosslin1, David Crossman4, Michael H Sketch Jr2, Christopher B Granger2, David Seo3, Pascal Goldschmidt-Clermont3, William E Kraus2, Simon G Gregory1,2, Elizabeth R Hauser1,2 and Svati H Shah1,2* Abstract Background: Coronary artery disease (CAD), and one of its intermediate risk factors, dyslipidemia, possess a demonstrable genetic component, although the genetic architecture is incompletely defined. We previously reported a linkage peak on chromosome 5q31-33 for early-onset CAD where the strength of evidence for linkage was increased in families with higher mean low density lipoprotein-cholesterol (LDL-C). Therefore, we sought to fine-map the peak using association mapping of LDL-C as an intermediate disease-related trait to further define the etiology of this linkage peak. The study populations consisted of 1908 individuals from the CATHGEN biorepository of patients undergoing cardiac catheterization; 254 families (N = 827 individuals) from the GENECARD familial study of early-onset CAD; and 162 aorta samples harvested from deceased donors. Linkage disequilibrium-tagged SNPs were selected with an average of one SNP per 20 kb for 126.6-160.2 MB (region of highest linkage) and less dense spacing (one SNP per 50 kb) for the flanking regions (117.7-126.6 and 160.2-167.5 MB) and genotyped on all samples using a custom Illumina array. -

DDX17 Antibody Order 021-34695924 [email protected] Support 400-6123-828 50Ul [email protected] 100 Ul √ √ Web
TD12935 DDX17 Antibody Order 021-34695924 [email protected] Support 400-6123-828 50ul [email protected] 100 uL √ √ Web www.ab-mart.com.cn Description: As an RNA helicase, unwinds RNA and alters RNA structures through ATP binding and hydrolysis. Involved in multiple cellular processes, including pre-mRNA splicing, alternative splicing, ribosomal RNA processing and miRNA processing, as well as transcription regulation. Regulates the alternative splicing of exons exhibiting specific features. For instance, promotes the inclusion of AC-rich alternative exons in CD44 transcripts. This function requires the RNA helicase activity. Affects NFAT5 and histone macro- H2A.1/MACROH2A1 alternative splicing in a CDK9-dependent manner. In NFAT5, promotes the introduction of alternative exon 4, which contains 2 stop codons and may target NFAT5 exon 4-containing transcripts to nonsense-mediated mRNA decay, leading to the down- regulation of NFAT5 protein. Affects splicing of mediators of steroid hormone signaling pathway, including kinases that phosphorylates ESR1, such as CDK2, MAPK1 and GSK3B, and transcriptional regulators, such as CREBBP, MED1, NCOR1 and NCOR2. By affecting GSK3B splicing, participates in ESR1 and AR stabilization. In myoblasts and epithelial cells, cooperates with HNRNPH1 to control the splicing of specific subsets of exons. In addition to binding mature mRNAs, also interacts with certain pri-microRNAs, including MIR663/miR- 663a, MIR99B/miR-99b, and MIR6087/miR-6087. Binds pri-microRNAs on the 3' segment flanking the stem loop via the 5'-[ACG]CAUC[ACU]-3' consensus sequence. Required for the production of subsets of microRNAs, including MIR21 and MIR125B1. May be involved not only in microRNA primary transcript processing, but also stabilization (By similarity).