Courses of Lectures of Inflammatory Diseases, Localized in the Maxilla-Facial Region
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accidental Displacement of Mandibular Third Molar Root Into the Submandibular Space: a Case Report
Case Report ERA’S JOURNAL OF MEDICAL RESEARCH VOL.6 NO.1 ACCIDENTAL DISPLACEMENT OF MANDIBULAR THIRD MOLAR ROOT INTO THE SUBMANDIBULAR SPACE: A CASE REPORT Mayur Vilas Limbhore, Viren S Patil, Shandilya Ramanojam, Vrushika Mahajan, Pallavi Rathi, Kisna Tadas Department of Oral and Maxillofacial surgery Bharati Vidyapeeth Dental College, Katraj, Pune, Maharashtra, India-411030 Received on : 01-04-2018 Accpected on : 10-04-2018 ABSTRACT Address for correspondence Accidental displacement of an impacted third molar, either a crown, Dr. Mayur Vilas Limbhore root piece, or the entire tooth, is a rare complication that occurs Department of Oral and Maxillofacial Surgery during surgical removal. The most common sites of dislodgment of an impacted mandibular third molar root are the submandibular, Bharati Vidyapeth Dental College, sublingual and pterygomandibular spaces. Removal of a displaced Katraj, Pune, Maharashtra, India-411030 root from these spaces may be complex due to poor visualization Email: [email protected] and limited access. A thorough evaluation of all significant risk Contact no: +91-8552887325 factors must be performed in advance to prevent complications. This case report reveals the management of accidental displaced mandibular third molar root into the submandibular space. An 39 years-old male patient underwent a third mandibular molar extraction. Accidentally, the mandibular right third molar distal root was displaced into the submandibular space, making necessary a second surgical step. After 2 days awaiting an asymptomatic health status, the second surgical step was successfully performed using multislice CBCT as preoperative imaging guide. The present case report highlights the clinical usefulness of CBCT in proper treatment of the patient. -

CASE REPORT Fibromatosis of Infratemporal Space Riaz Ahmed Warraich, Tooba Saeed, Nabila Riaz, Asma Aftab
217 CASE REPORT Fibromatosis of infratemporal space Riaz Ahmed Warraich, Tooba Saeed, Nabila Riaz, Asma Aftab Abstract chemotherapy or non-cytotoxic drugs are also Fibromatosis is a rare benign mesenchymal neoplasm considerable modalities for AF management, to avoid which primarily originates in the muscle, connective sacrifising functional integrity as a price of attaining tissue, fascial sheaths, and musculoaponeurotic tumour-free margins. 3 structures. It is commonly seen as abdominal tumour but Case Report in maxillofacial region, the occurrence of these tumours is very rare and exceedingly rare in infratemporal space. A 35-year-old female visited Oral and Maxillofacial Often misdiagnosed due to its varied clinical behaviour, Department of Mayo Hospital on October 5, 2014. Written fibromatosis is benign, slow-growing, infiltrative tumour informed consent was obtained from the patient for without any metastatic potential, but is locally aggressive publication of this report and accompanying images. Her causing organ dysfunction along with high recurrence chief complaint was of progressive reduction in mouth rate. We report a case of fibromatosis involving the left opening gradually for the preceding 4 years. Medical infratemporal space in a 35-year-old female who history revealed that she had extra pulmonary presented with chief complaint of limited mouth opening tuberculous lesion in left side of her neck which was for the preceding 4 years. treated 10 years earlier. Clinical examination revealed slight thickening and fibrosis of left cheek with zero Keywords: Aggressive fibromatosis, Infratemporal, mouth opening. Overlying skin was normal. There was no Benign, Infiltrative. Introduction Aggressive fibromatosis (AF) or extra-abdominal desmoid tumours are rare tumours of fibroblastic origin involving the proliferation of cytologically benign fibrocytes. -
Anatomical Overview
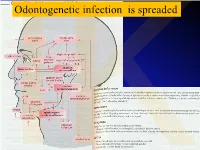
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Retained Surgical Items Evidence Table
Guideline for Prevention of Retained Surgical Items Evidence Table CITATION CONCLUSION(S) SAMPLE SIZE REFERENCE # POPULATION COMPARISON EVIDENCE TYPE INTERVENTIONS CONSENSUS SCORE OUTCOME MEASURE 1 Wilson C. Foreign bodies left in the Case series of foreign bodies left in the abdomen. Cases VC Literature n/a n/a n/a n/a Retained abdomen after laparotomy. Trans Am found through publication, interviews, and the author's own Review, Clinician sponges Gynecol Soc. 1884;9:94-117. experience. Experience, and Case Report 2 The Joint Commission. Preventing The Joint Commission recommends that facilities develop IVB Consensus n/a n/a n/a n/a n/a unintended retained foreign objects. effective processes and procedures for preventing Sentinel Event Alert. October 17, unintended retained foreign objects. Their recommendations 2013;51. include a standardized and highly reliable counting system; http://www.jointcommission.org/sea_i development of policies and procedures; practices for ssue_51/. Accessed November 10, counting, wound opening, and closing procedures; 2015. performance of intraoperative radiographs; use of effective communication to include briefings and debriefings; documentation of counts; and assistive technologies (ie, RF tags, RFID, radiopaque, bar coding). Also, the hospital should define a process for conducting RCA for sentinel events, such as URFO. Page 1 of 60 Guideline for Prevention of Retained Surgical Items Evidence Table CITATION CONCLUSION(S) SAMPLE SIZE REFERENCE # POPULATION COMPARISON EVIDENCE TYPE INTERVENTIONS CONSENSUS SCORE OUTCOME MEASURE 3 Moffatt-Bruce SD, Cook CH, Steinberg 7 elevated risk factors for RSI in pooled data in case-control IIIA Systematic USA hospitals, n/a n/a 3 studies: Estimated SM, Stawicki SP. -

Anatomy of the Pterygomandibular Space — Clinical Implication and Review
FOLIA MEDICA CRACOVIENSIA 79 Vol. LIII, 1, 2013: 79–85 PL ISSN 0015-5616 MARCIN LIPSKI1, WERONIKA LIPSKA2, SYLWIA MOTYL3, Tomasz Gładysz4, TOMASZ ISKRA1 ANATOMY OF THE PTERYGOMANDIBULAR SPACE — CLINICAL IMPLICATION AND REVIEW Abstract: A i m: The aim of this study was to present review of the pterygomandibular space with some referrals to clinical practice, specially to the methods of lower teeth anesthesia. C o n c l u s i o n s: Pterygomandibular space is a clinically important region which is commonly missing in anatomical textbooks. More attention should be paid to it both from theoretical and practical point of view, especially in teaching the students of first year of dental studies. Key words: pterygomandibular space, Gow-Gates anesthesia, inferior alveolar nerve. INTRODUCTION Numerous cranial regions have been subjects of various anatomical and anthro- pological studies [1, 2]. Most of them indicate necessity of undertaking of such studies first of all because of clinical importance [3–5]. Inferior alveolar nerve blocs, one of the most common procedures in dentistry requires deep anatomical knowledge of the pterygomandibular space [6, 7]. This space is a narrow gap, which contains mostly loose areolar tissue. It communi- cates however through the mandibular foramen with the mandibular canal, which is traversed by inferior alveolar nerve, artery and comitant vein (IANAV). Many of the structures placed in this space are of certain importance for local anesthesia. Khoury at al. [8, 9] mention here the following: inferior alveolar nerve, artery and vein, lingual nerve, nerve to mylohyoid and the sphenomandibular ligament. The space contains mostly loose areolar tissue. -

Diapositiva 1
Ingegneria delle tecnologie per la salute Fondamenti di anatomia e istologia Lezione 4.a.b.c aa. 2018-19 Ingegneria delle tecnologie per la salute Fondamenti di anatomia e istologia aa. 2018-179 Sistema locomotore • Ossa 4.a • Articolazioni 4.b • Muscoli 4.c BONES 4.a BONE TISSUE & SKELETAL SYSTEM After this lesson, you will be able to: • List and describe the functions of bones • Describe the classes of bones • Discuss the process of bone formation and development Functions of the Skeletal System Bone (osseous tissue) = hard, dense connective tissue that forms most of the adult skeleton, the support structure of the body. Cartilage = a semi-rigid form of connective tissue, in the areas of the skeleton where bones move provides flexibility and smooth surfaces for movement. Skeletal system = body system composed of bones and cartilage and performing following functions: • supports the body • facilitates movement • protects internal organs • produces blood cells • stores and releases minerals and fat Bone Classification 206 bones composing skeleton, divided into 5 categories based on their shapes ( distinct function) Bone Classification Bone Structure Bone tissue differs greatly from other tissues in the body: is hard (many of its functions depend on this hardness) and also dynamic (its shape adjusts to accommodate stresses). histology gross anatomy Gross Anatomy of Bone structure of a LONG BONE, 2 parts: 1. diaphysis: tubular shaft that runs between the proximal and distal ends of the bone, where the hollow region is called medullary cavity (filled with yellow marrow) and the walls are composed of dense and hard compact bone 2. -

Deep Neck Infections 55
Deep Neck Infections 55 Behrad B. Aynehchi Gady Har-El Deep neck space infections (DNSIs) are a relatively penetrating trauma, surgical instrument trauma, spread infrequent entity in the postpenicillin era. Their occur- from superfi cial infections, necrotic malignant nodes, rence, however, poses considerable challenges in diagnosis mastoiditis with resultant Bezold abscess, and unknown and treatment and they may result in potentially serious causes (3–5). In inner cities, where intravenous drug or even fatal complications in the absence of timely rec- abuse (IVDA) is more common, there is a higher preva- ognition. The advent of antibiotics has led to a continu- lence of infections of the jugular vein and carotid sheath ing evolution in etiology, presentation, clinical course, and from contaminated needles (6–8). The emerging practice antimicrobial resistance patterns. These trends combined of “shotgunning” crack cocaine has been associated with with the complex anatomy of the head and neck under- retropharyngeal abscesses as well (9). These purulent col- score the importance of clinical suspicion and thorough lections from direct inoculation, however, seem to have a diagnostic evaluation. Proper management of a recog- more benign clinical course compared to those spreading nized DNSI begins with securing the airway. Despite recent from infl amed tissue (10). Congenital anomalies includ- advances in imaging and conservative medical manage- ing thyroglossal duct cysts and branchial cleft anomalies ment, surgical drainage remains a mainstay in the treat- must also be considered, particularly in cases where no ment in many cases. apparent source can be readily identifi ed. Regardless of the etiology, infection and infl ammation can spread through- Q1 ETIOLOGY out the various regions via arteries, veins, lymphatics, or direct extension along fascial planes. -

Guidance for the Format and Content of the Protocol of Non-Interventional
PASS information Title Metformin use in renal impairment Protocol version identifier Version 2 Date of last version of 30 October 2013 protocol EU PAS register number Study not registered Active substance A10BA02 metformin Medicinal product Metformin Product reference N/A Procedure number N/A Marketing authorisation 1A Farma, Actavis, Aurobindo, Biochemie, Bluefish, holder(s) Hexal, Mylan, Orifarm, Pfizer, Sandoz, Stada, Teva Joint PASS No Research question and To assess the use and safety of metformin in patients objectives with and without renal insufficiency in current clinical practice in at least two EU Member States. Country(-ies) of study Denmark, United Kingdom Author Christian Fynbo Christiansen, MD, PhD Page 1/214 Marketing authorisation holder(s) Marketing authorisation N/A holder(s) MAH contact person N/A Page 2/214 1. Table of Contents PASS information .......................................................................................................... 1 Marketing authorisation holder(s) .................................................................................... 2 1. Table of Contents ...................................................................................................... 3 2. List of abbreviations ................................................................................................... 4 3. Responsible parties .................................................................................................... 5 4. Abstract .................................................................................................................. -

Infratemporal Abscess in an Adolescent Following a Dental Procedure
Central Annals of Pediatrics & Child Health Research Article *Corresponding author Vijay CS, Department of Pediatrics, West Virginia University, Medical Center Dr, Morgantown, USA, Tel: 304-293-6307; Fax: 304-293-1216; Email: Infratemporal Abscess in an Submitted: 30 November 2018 Adolescent Following a Dental Accepted: 02 January 2019 Published: 04 January 2019 ISSN: 2373-9312 Procedure Copyright © 2019 Vijay et al. Vijay CS* and Chen CB OPEN ACCESS Department of Pediatrics, West Virginia University, USA Keywords • Abscess Abstract • Infratemporal fossa Infections in the infratemporal region can be a major source of morbidity and have • Odontogenic infections been known to occur after dental procedures. Neurovascular structures running through the infratemporal fossa serve as a source for infections to track to different areas of the head and neck. The proximity of the infratemporal fossa to other major structures makes timely diagnosis critical. Infratemporal fossa abscesses are a rare complication and only a few cases have been described in the literature. As the clinical symptoms may be non-specific, the diagnosis may be challenging for healthcare providers. We describe a patient who presented with facial swelling and trismus following wisdom tooth extraction who was found to have an infratemporal fossa abscess. ABBREVIATIONS CASE PRESENTATION CT: Computed Tomography; MRI: Magnetic Resonance A 14-year-old previously healthy male presented with Imaging left-sided facial swelling and jaw stiffness. He complained of associated tenderness to palpation over the left side of his face INTRODUCTION The infratemporal fossa is an extremely important site, as it initially started three days after he had four wisdom teeth communicates with several surrounding structures including the extracted.and jaw and As his difficulty symptoms opening did not his resolve, mouth. -

Refractory Odontogenic Infection Associated to Candida Albicans: a Case Report
Case Report Clinics in Surgery Published: 31 Mar, 2017 Refractory Odontogenic Infection Associated to Candida Albicans: A Case Report Daya A Mikhail*, Mederos Heidi BS and McClure Shawn Department of Oral and Maxillofacial Surgery, Nova Southeastern University /Broward Health Medical Center, USA Abstract Background: Multifascial space infections from an odontogenic origin have been attributed to a different number of microorganisms. These infections can be serious, involving multiple deep spaces in the head and neck, and potentially compromising the airway. Fungal etiology including C. albicans has been reported in the past as a rare agent involving multifascial space infections. Case Description: We present an unusual case of a severe deep space infection associated with carious teeth numbers 31 and 32. This specific infection proved to be resistant to multiple antibiotic therapy and required incision and drainage on two different occasions. After the initial surgery, the patient remained febrile with an elevated white blood cell count; thus, the patient was taken to the operating room again for a re-drainage and new cultures. Cultures obtained during the second surgery were positive for C. albicans. The patient was responsive to antifungal therapy, showing quick improvement in his condition. Conclusion: Although multiple factors could have contributed to this patient’s vulnerability to odontogenic infection of fungal etiology including history of alcoholism and broad spectrum antibiotic therapy, it remains an infrequent finding in the literature. This case illustrates the need to consider a fungal cause in patients with odontogenic infections who are not responsive to broad spectrum antibiotics and surgical drainage. Keywords: Odontogenic infection; Candida albicans; Microorganisms Introduction OPEN ACCESS Many microorganisms have been identified in multifascial space infections of the head and *Correspondence: neck region. -

Tests Spring 2012
Tests spring 2013 Test 1 Oral cavity 1. Vestibulum oris does not communicate with proper oral cavity through: :r1 oral part of pharynx :r2 tremata :r3 space behind last molar :r4 space when tooth is missing :r5 communicates through all mentioned ways -- 2. Into vestibule of oral cavity opens out: :r1 caruncula sublingualis :r2 papilla parotidea :r3 ductus nasolacrimalis :r4 plica sublingualis :r5 none of mentioned answers is correct -- 3. The underlay of lips is: :r1 m. labialis :r2 m. orbicularis oculi :r3 m. orbicularis oris :r4 m. buccalis :r5 none of mentioned answers is correct -- 4. The upper lip is partially connected with alveolar process using: :r1 lig. labii superioris :r2 m. platysma :r3 frenulum labii superioris :r4 plica labii superioris :r5 none of mentioned answers is correct -- 5. Cheek is not made up of: :r1 skin :r2 adipose body :r3 muscular layer :r4 adventitia :r5 none of mentioned answers is correct -- 6. Parotid duct passes through: :r1 m. masseter :r2 m. buccinator :r3 m. orbicularis oris :r4 m. pterygoideus lateralis :r5 none of mentioned answers is correct -- 7. The underlay of hard palate is not: :r1 praemaxilla :r2 vomer :r3 processus palatinus maxillae :r4 lamina horizontalis ossis palatini :r5 all mentioned bones form the underlay of hard palate -- 8. Which statement describing mucosa of hard palate is not correct: :r1 it contains big amount of submucosal connective tissue :r2 it is covered by columnar epithelium :r3 firmly grows together with periosteum :r4 it is almost not movable against the bottom :r5 it contains glandulae palatinae -- 9. Mark the true statement describing the palate: :r1 there is papilla incisiva positioned there :r2 mucosa contains glandulae palatinae :r3 there are plicae palatinae transversae positioned there :r4 the basis of soft palate is made by fibrous aponeurosis palatina :r5 all mentioned statements are correct -- 10. -

Fig. 2-32 Facial Muscles. Fig. 2-33 Trigeminal Nerve (CN V)
Fig. 2-32 Facial Muscles. Fig. 2-33 Trigeminal Nerve (CN V) leaving the Skull. 51 thetic agent at the infraorbital foramen or in the infraor- posterior to its head and anterior to the auricle. It then bital canal (e.g., for treatment of wounds of the upper crosses over the root of the zygomatic process of the lip and cheek or for repairing the maxillary incisor teeth). temporal bone, deep to the superficial temporal artery. The site of emergence of this nerve can easily be deter- As its name suggests, it supplies parts of the auricle, mined by exerting pressure on the maxilla in the region external acoustic meatus, tympanic membrane (ear- of the infraorbital foramen and nerve. Pressure on the drum), and skin in the temporal region. The inferior al- nerve causes considerable pain. Care is exercised when veolar nerve is the large terminal branch of the posterior performing an infraorbital nerve block because compan- division of CN V3; the lingual nerve is the other terminal ion infraorbital vessels leave the infraorbital foramen with branch. It enters the mandibular canal through the man- the nerve. Careful aspiration of the syringe during injec- dibular foramen. In the canal it gives off branches that tion prevents inadvertent injection of the anesthetic fluid supply the mandibular (lower) teeth. Opposite the mental into a blood vessel. The orbit is located just superior to foramen, the inferior alveolar nerve divides into its ter- the injection site. A careless injection could result in minal incisive and mental branches. The incisive nerve the passage of anesthetic fluid into the orbit, causing supplies the incisor teeth, the adjacent gingiva, and temporary paralysis of the extraocular muscles.