Acne Vulgaris Handout
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Undiluted Tea-Tree Oil As a Cosmetic
Federal Institute for Risk Assessment (BfR) Use of undiluted tea-tree oil as a cosmetic Opinion of the Federal Insitute for Risk Assessment (BfR), 1th September 2003 Background Recently there has been an increasing amount of reports on contact-allergic eczema in con- junction with the use of tea-tree oil. Tea-tree oil is sold as a pure natural product, highly con- centrated and undiluted in cosmetics. Tea-tree oil is advertised as a universal remedy al- though there is no marketing authorisation as a pharmaceutical product. Concentrated tea-tree oil has been classified as harmful according to the self-classification of the International Fragrance Association (IFRA) and is labelled with R-phrases R 22 (harmful if swallowed) R 38 (irritating to skin) and R 65 (may cause lung damage if swallowed) as well as the symbol Xn (harmful) (IFRA Labelling Manual 1, 2001). These indications of health hazards are also part of the safety data sheets of raw material suppliers. At the 65th and 66th meetings of the Cosmetics Committee at the Federal Institute for Risk Assessment (BfR), health risks associated with the use of undiluted and highly concentrated tea-tree oil in cosmetic products were discussed extensively. Result Tea-tree oil is a mixture of various terpenes extracted from the Australian tea-tree. Undiluted tea-tree oil is a pure natural product. In the presence of atmospheric oxygen but also when exposed to light and higher temperatures, oxidation processes occur leading to the formation of peroxides, epoxides and endoperoxides which have a sensitising potency and may trigger allergic skin reactions. -

Outpatient Acne Care Guideline
Outpatient Acne Care Guideline Severity Mild Moderate Severe < 20 comedones or < 20-100 comedones or 15-50 > 5 cysts, >100 comedones, or inflammatory lesions inflammatory lesions >50 inflammatory lesions Initial Treatment Initial Treatment Initial Treatment Benzoyl Peroxide (BP) or Topical Combination Therapy Combination Therapy Topical Retinoid Retinoid + BP Oral antibiotic or OR + (Retinoid + Antibiotic) + BP Topical retinoid Topical Combination Therapy or + BP + Antibiotic Retinoid + (BP + Antibiotic) or OR BP Retinoid + BP Oral antibiotic + topical retinoid + +/- or BP Topical antibiotic Retinoid + Antibiotic + BP or Topical Dapsone IF Inadequate Response IF Inadequate Response IF Inadequate Consider dermatology Response referral Change topical retinoid Consider changing oral concentrations, type and/or antibiotic formulation AND or Add BP or retinoid, if not already Change topiocal combination Consider isotretinoin prescribed therapy Consider hormone therapy or and/or (females) Change topical retinoid Add or change oral antibiotic concentrations, type and/or or formulation Consider isotretinoin Additional Considerations or Consider hormone therapy (females) Change topical comination Previous treatment/history Side effects therapy Costs Psychosocial impact Vehicle selection Active scarring Ease of use Regimen complexity Approved Evidence Based Medicine Committee 1-18-17 Reassess the appropriateness of Care Guidelines as condition changes. This guideline is a tool to aid clinical decision making. It is not a standard of care. The physician should deviate from the guideline when clinical judgment so indicates. GOAL: Pediatricians should initiate treatment for cases of “Mild” to “Severe” acne (see algorithms attached). Pediatricians should also counsel patients in order to maximize adherence to acne treatment regimens: 1. Realistic expectations. Patients should be counseled that topical therapies typically take up to 6-8 weeks to start seeing results. -

Formulary Drug Removals
July 2018 Formulary Drug Removals Below is a list of medicines by drug class that have been removed from your plan’s formulary. If you continue using one of the drugs listed below and identified as a Formulary Drug Removal, you may be required to pay the full cost. If you are currently using one of the formulary drug removals, ask your doctor to choose one of the generic or brand formulary options listed below. Category Formulary Drug Formulary Options Drug Class Removals Allergies BECONASE AQ flunisolide spray, fluticasone spray, mometasone spray, triamcinolone spray, Nasal Steroids / Combinations OMNARIS DYMISTA QNASL ZETONNA Anticonvulsants ZONEGRAN carbamazepine, carbamazepine ext-rel, divalproex sodium, divalproex sodium ext-rel, gabapentin, lamotrigine, lamotrigine ext-rel, levetiracetam, levetiracetam ext-rel, oxcarbazepine, phenobarbital, phenytoin, phenytoin sodium extended, tiagabine, topiramate, valproic acid, zonisamide, FYCOMPA, OXTELLAR XR, TROKENDI XR, VIMPAT Anti-infectives, Antibacterials E.E.S. GRANULES erythromycins Erythromycins / Macrolides ERYPED Anti-infectives, Antibacterials MINOCIN minocycline Tetracyclines DORYX doxycycline hyclate DORYX MPC MONODOX Anti-infectives, Antibacterials MACRODANTIN nitrofurantoin Miscellaneous Anti-infectives, Antivirals VALCYTE valganciclovir Cytomegalovirus * Anti-infectives, Antivirals MAVYRET EPCLUSA (genotypes 1, 2, 3, 4, 5, 6), HARVONI (genotypes 1, 4, 5, 6), VOSEVI 1 Hepatitis C * DAKLINZA EPCLUSA (genotypes 1, 2, 3, 4, 5, 6), HARVONI (genotypes 1, 4, 5, 6) OLYSIO TECHNIVIE -

Mechanisms of Action of Azelaic Acid 15% Gel: Assessing Its Broad Antioxidant and Comedolytic Effects Zoe Diana Draelos, MD
CCOSMETIOSMETICC CCONSULTATIONONSULTATION Mechanisms of Action of Azelaic Acid 15% Gel: Assessing Its Broad Antioxidant and Comedolytic Effects Zoe Diana Draelos, MD wo small studies were undertaken to investi- Dermatologic medications can have a similar versatility gate the ability of azelaic acid (AzA) 15% gel of action. For example, tetracyclines are used for their T to function as a comedolytic and as a topical antibacterial and anti-inflammatory qualities to treat antioxidant. The first study compared AzA 15% gel with acne. Sodium sulfacetamide and sulfur combinations are benzoyl peroxide (BPO) 5% gel as a comedolytic. Ten used for antibacterial, antifungal, and anti-inflammatory participants were randomized to apply AzA 15% gel on purposes for acne, seborrheic dermatitis, and rosacea. one shoulder and BPO 5% gel on the other shoulder One could argue that versatile ingredients can often be twice daily for 4 weeks, with a nontreated site on the more valuable than those that deliver a single, albeit central back serving as the control in all participants. powerful, effect. Comedone counts were obtainedCOS at baseline and week DERM4 An alternate dermatologic prescription that has mul- by examination of cyanoacrylate biopsies taken from tiple mechanisms of action is AzA 15% gel. Also known each site. The AzA 15% gel and BPO 5% gel produced as nonanedioic acid, AzA is a saturated dicarboxylic acid substantial decreases in mean comedones (12 to 0.9 and found naturally in wheat, rye, and barley. It is also pro- 14.9 to 1.6, respectively) from baseline to week 4 as duced by the yeast Pityrosporum ovale, a natural compo- compared with controlsDo (14.6 to 10.9). -

Comparing 2.5%, 5%, and 10% Benzoyl Peroxide on Inflammatory
Pharmacology and Therapeutics Comparing 2.5%, 5%, and 10% Benzoyi Peroxide on Inflammatory Acne Vulgaris OTTO H. MILLS, JR., PH.D., ALBERT M. KLICMAN, M.D., PH.D., PETER POCHI, M.D., AND HARRIET COMITE, M.D. From the Departments of Dermatology, University of Subjects, Materials, and Methods Pennsy/vania School of Medicine, Philadelphia, Pennsylvania, and Boston University School of Medicine, Clinical Studies Boston, Massachusetts The same methods were used to conduct three double- blind studies. After giving informed consent, subjects with mild to moderately severe inflammatory acne vulgaris of the face (minimum of 10 inflammatory lesions) were assigned to one of the three treatment groups. A total of 153 subjects, 74 men and 79 women (average age of 20 years), participated ABSTRACT: A 2.5% formulation of benzoyi peroxide was in the three studies. In the first, 25 subjects used 2.5% ben- compared with its vehicle, and with a 5% and a 10% proprietary zoyi peroxide gel and 25, the gel vehicle for this formulation. benzoyi peroxide gel preparation in three double-blind studies In the second, 26 used the 2.5 gel and 27, a 5% gel. The involving 153 patients with mild to moderately severe acne third study consisted of 25 subjects who used the 2.5% gel vulgaris. The 2.5% benzoyi peroxide formulation was more and 25, a 10% benzoyi peroxide gel. The subjects received effective than its vehicle and equivalent to the 5% and 10% no medications for any reasor\s during \he 4-week period concentrations in reducing the number of inflammatory lesions prior to the start of the study. -

Long-Term Use of Spironolactone for Acne in Women: a Case Series of 403 Patients
Long-term use of spironolactone for acne in women: A case series of 403 patients Vaibhav Garg, BS,a JulianaK.Choi,MD,PhD,b William D. James, MD,b and John S. Barbieri, MD, MBAb Philadelphia, Pennsylvania Background: There are limited data regarding the long-term outcomes of spironolactone use for women with acne and its effect on truncal acne. Objective: To comprehensively describe outcomes of patients treated with spironolactone in routine clinical practice, including long-term outcomes. Methods: We performed a retrospective case series of 403 adult women treated for acne with spironolactone at an academic medical center between 2008 and 2019. Rates of objective, as assessed by Comprehensive Acne Severity Scale scores, and subjective acne clearance were evaluated, as well as rates of treatment discontinuation, dosage changes, and drug survival. Logistic regression was used to assess for association between incidence of menstrual adverse effects and combined oral contraceptive use. Results: As evaluated by Comprehensive Acne Severity Scale scores, at the first follow-up, 75.5%, 84.0%, and 80.2% of patients with available data had reduction or complete clearance of acne on the face, chest, and back, respectively. The mean drug survival was 470.7 days. Menstrual adverse effects were less common among those using combined oral contraception (odds ratio, 0.23; 95% confidence interval, 0.11-0.50). Limitations: This study was conducted at a single academic medical center. Conclusions: Spironolactone improves clinical outcomes and is well tolerated for many adult women with acne using it for an extended duration. ( J Am Acad Dermatol 2021;84:1348-55.) Key words: acne; acne vulgaris; birth control pill; combined oral contraceptive; comprehensive acne severity scale; oral antibiotics; outcomes; spironolactone. -

Therapeutic Drug Class
BUREAU FOR MEDICAL SERVICES WEST VIRGINIA MEDICAID EFFECTIVE PREFERRED DRUG LIST WITH PRIOR AUTHORIZATION CRITERIA 04/01/11 This is not an all-inclusive list of available covered drugs and includes only Version 2011.9 managed categories. Refer to cover page for complete list of rules governing this PDL. • Prior authorization for a non-preferred agent in any category will be given only if there has been a trial of the preferred brand/generic equivalent or preferred formulation of the active ingredient, at a therapeutic dose, that resulted in a partial response with a documented intolerance. • Prior authorization of a non-preferred isomer, pro-drug, or metabolite will be considered with a trial of a preferred parent drug of the same chemical entity, at a therapeutic dose, that resulted in a partial response with documented intolerance or a previous trial and therapy failure, at a therapeutic dose, with a preferred drug of a different chemical entity indicated to treat the submitted diagnosis. (The required trial may be overridden when documented evidence is provided that the use of these preferred agent(s) would be medically contraindicated.) • Unless otherwise specified, the listing of a particular brand or generic name includes all legend forms of that drug. OTC drugs are not covered unless specified. • PA criteria for non-preferred agents apply in addition to general Drug Utilization Review policy that is in effect for the entire pharmacy program, including, but not limited to, appropriate dosing, duplication of therapy, etc. • The use of pharmaceutical samples will not be considered when evaluating the members’ medical condition or prior prescription history for drugs that require prior authorization. -

Aetna Formulary Exclusions Drug List
Covered and non-covered drugs Drugs not covered – and their covered alternatives 2020 Advanced Control Plan – Aetna Formulary Exclusions Drug List 05.03.525.1B (7/20) Below is a list of medications that will not be covered without a Key prior authorization for medical necessity. If you continue using one of these drugs without prior approval, you may be required UPPERCASE Brand-name medicine to pay the full cost. Ask your doctor to choose one of the generic lowercase italics Generic medicine or brand formulary options listed below. Preferred Options For Excluded Medications1 Excluded drug name(s) Preferred option(s) ABILIFY aripiprazole, clozapine, olanzapine, quetiapine, quetiapine ext-rel, risperidone, ziprasidone, VRAYLAR ABSORICA isotretinoin ACANYA adapalene, benzoyl peroxide, clindamycin gel (except NDC^ 68682046275), clindamycin solution, clindamycin-benzoyl peroxide, erythromycin solution, erythromycin-benzoyl peroxide, tretinoin, EPIDUO, ONEXTON, TAZORAC ACIPHEX, esomeprazole, lansoprazole, omeprazole, pantoprazole, DEXILANT ACIPHEX SPRINKLE ACTICLATE doxycycline hyclate capsule, doxycycline hyclate tablet (except doxycycline hyclate tablet 50 mg [NDC^ 72143021160 only], 75 mg, 150 mg), minocycline, tetracycline ACTOS pioglitazone ACUVAIL bromfenac, diclofenac, ketorolac, PROLENSA acyclovir cream acyclovir (except acyclovir cream), valacyclovir ADCIRCA sildenafil, tadalafil ADZENYS XR-ODT amphetamine-dextroamphetamine mixed salts ext-rel†, dexmethylphenidate ext-rel, dextroamphetamine ext-rel, methylphenidate ext-rel†, MYDAYIS, -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -
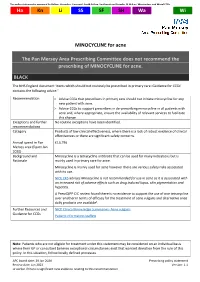
MINOCYCLINE for Acne
This policy statement is approved by Halton, Knowsley, Liverpool, South Sefton, Southport and Formby, St Helens, Warrington, and Wirral CCGs Ha Kn Li SS SF SH Wa Wi MINOCYCLINE for acne The Pan Mersey Area Prescribing Committee does not recommend the prescribing of MINOCYCLINE for acne. BLACK The NHS England document ‘Items which should not routinely be prescribed in primary care: Guidance for CCGs’ contains the following advice.1 Recommendation Advise CCGs that prescribers in primary care should not initiate minocycline for any new patient with acne. Advice CCGs to support prescribers in de-prescribing minocycline in all patients with acne and, where appropriate, ensure the availability of relevant services to facilitate this change. Exceptions and further No routine exceptions have been identified. recommendations Category Products of low clinical effectiveness, where there is a lack of robust evidence of clinical effectiveness or there are significant safety concerns. Annual spend in Pan £13,796 Mersey area (Epact Jan. 2020) Background and Minocycline is a tetracycline antibiotic that can be used for many indications but is Rationale mainly used in primary care for acne. Minocycline is mainly used for acne however there are various safety risks associated with its use. NICE CKS advises Minocycline is not recommended for use in acne as it is associated with an increased risk of adverse effects such as drug induced lupus, skin pigmentation and hepatitis. A PrescQIPP CIC review found there is no evidence to support the use of one tetracycline over another in terms of efficacy for the treatment of acne vulgaris and alternative once daily products are available2. -

Australian Statistics on Medicines 1997 Commonwealth Department of Health and Family Services
Australian Statistics on Medicines 1997 Commonwealth Department of Health and Family Services Australian Statistics on Medicines 1997 i © Commonwealth of Australia 1998 ISBN 0 642 36772 8 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be repoduced by any process without written permission from AusInfo. Requests and enquiries concerning reproduction and rights should be directed to the Manager, Legislative Services, AusInfo, GPO Box 1920, Canberra, ACT 2601. Publication approval number 2446 ii FOREWORD The Australian Statistics on Medicines (ASM) is an annual publication produced by the Drug Utilisation Sub-Committee (DUSC) of the Pharmaceutical Benefits Advisory Committee. Comprehensive drug utilisation data are required for a number of purposes including pharmacosurveillance and the targeting and evaluation of quality use of medicines initiatives. It is also needed by regulatory and financing authorities and by the Pharmaceutical Industry. A major aim of the ASM has been to put comprehensive and valid statistics on the Australian use of medicines in the public domain to allow access by all interested parties. Publication of the Australian data facilitates international comparisons of drug utilisation profiles, and encourages international collaboration on drug utilisation research particularly in relation to enhancing the quality use of medicines and health outcomes. The data available in the ASM represent estimates of the aggregate community use (non public hospital) of prescription medicines in Australia. In 1997 the estimated number of prescriptions dispensed through community pharmacies was 179 million prescriptions, a level of increase over 1996 of only 0.4% which was less than the increase in population (1.2%). -

Benzoyl Peroxide Vs. Salicylic Acid WHAT to USE and WHEN
benzoyl peroxide vs. salicylic acid WHAT TO USE AND WHEN BENZOYL PEROXIDE AND SALICYLIC ACID ARE THE TWO MAIN INGREDIENTS IN MOSI OVER-THE-COUNTER TOPICAL ACNE PRODUCTS. BUT HOW DO THEY WORK, HOW ARE qr' THEY DIFFERENT AND WHICH ONE IS RIGHT FOR YOU7 > salicylic acid PREVENTS CLOGGED PORES BY AIDING ExFoLImIoN Atne forms wheh skin ceUs inside the hair falltck clump together and phq up the fulUcle. Salicylic HOW TO USE acid help sped cot1 twrnovgr on the surfate and slow the shedding of cells inside the foliicte tcr I.i pkwnt the clogging that causes a pimple. 5~lieylicacid aLo breaks down whiteheads ad San Francisco dermatologist blackheads. Technicalty a beta hydraxy acid, salicylic acid exfoliates and reduces oiliness, acne and Kathy Fields. MD, recommends 4 the appeal-nee of fine lines. It Is availableover-thecaunter in concentrstiom of 0.5 ta 246. but those a leave-on product or gentle , with sensitive skin shwld start with a lcHnier contentratton before trying stronger prcrducts. scrub or wash that doesn't strip ' the skin of moisture. "The key is to find a product you like using so you stick with it." she says. This ingredient can be irritating to sensitive skin, especially when combined with benzoyl peroxide, sulfur or other acne treatments. Mild stinging upon application is common. Salicylic acid may cause increased sun sensitivity, so be sure to use sunscreen daily. Salicylic acid must be used con- tinuously for results. If you stop, your pores will get clogged once again and your acne will return. KINERASE CLEAR SKlX w6xLERAGNOSw MWiUo CUIIEtFflNG Salicylic acid does not have an BLtSHlSH OIssOlVER OVERNIM ACNE CtEAmml effect on the production of REPAIR LOTION This spot treatment contains In addition to salitylic acid, sebum Ithe skin's natural oil], salicylic acid and glycolic acid Fight acne and aging with one this daily cleanser contains tri- or P.