2020 Wolters Kluwer Health, Inc. All Rights Reserved. a Snapshot Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Curriculum Vitae
C URRICULUM V ITAE - A NNA D E G RASSI PERSONAL INFORMATION Surname Name De Grassi Anna Date of birth 03-02-1976 Department Bioscienze, Biotecnologie e Biofarmaceutica Institution Università degli Studi di Bari “Aldo Moro” Street Address Via Orabona 4, 70125 Bari - Italy. Phone/Fax +39 080 5443614/ +39 080 5442770 E-mail address [email protected] Researcher Orcid Identifier https://orcid.org/0000-0001-7273-4263 EDUCATION 2007 PhD in Genetics and Molecular Evolution, University of Bari – Italy 2004 Master Diploma in Bioinformatics, University of Turin – Italy, 110/110 2003 Qualification to practice the profession of Biologist 2002 University Diploma in Biological Sciences, University of Bari – Italy, 110/110 cum laude 1994 Secondary School Diploma, Liceo Classico Q. Orazio Flacco, Bari – Italy, 60/60 RESEARCH ACTIVITY IN ITALY From October 2012 Assistant Professor (BIO/13), Department of Biosciences, Biotechnology and Biopharmaceutics, University of Bari, Computational Genomics applied to Cancer and Rare Diseases 2007-2011 Post-Doc and Staff Scientist, Department of Experimental Oncology, European Institute of Oncology, Milan, Deep-Sequencing and Evolution of Cancer Genomes 2004-2007 PhD student, CNR – Institute of Biomedical Technologies (ITB), Bari, Comparative Genomics of gene families in vertebrates and Microarray Analysis of Human Cancer Cell Models 2003-2004 Master Diploma Student, Department of Clinical and Biological Sciences, University of Turin, Detection and Analysis of Genes Involved in Breast Tumor Progression in the her/neut Mouse Model Using Expression Microarrays 2003 Graduate Student, Cavalieri Ottolenghi Foundation, Turin, Actin-Tubulin Interaction in D. melanogaster Embryonic Cell Lines 2001-2002 Undergraduate Student, Department of Genetics, University of Bari, Evolution of Stellate-like and Crystal-like Sequences in the Genus Drosophila RESEARCH ACTIVITY ABROAD Dec. -

Utilizzi Primaria Posto Comune
UTILIZZI PRIMARIA POSTO COMUNE Procedura Classe di Posizione Punteggio Cognome Nome SEDE TITOLARITA' SEDE UTILIZZO concorsuale concorso DDG 1546/18 EEEE 40 84,4 DI LORENZO MARISA MILANO - DA VINCI - MILANO - IC STOPPANI - MIEE8B601N MIEE8FT01L DDG 1546/18 EEEE 53 83,9 CALIFANO RAFFAELLA PESCHIERA - DE ANDRE' - PAULLO - CURIEL - MIEE8A202R MIEE8AB01Q DDG 1546/18 EEEE 58 83,5 SCOTELLARO ALESSIA MILANO - GIACOSA - MILANO - UMBERTO ECO - MIEE8FZ01G MIEE8DD017 DDG 1546/18 EEEE 59 83,5 PINI GILDA CAMILLA MILANO - BAROZZI - MILANO - VIA PALMIERI - MIEE8FV018 MIEE8CB011 DDG 1546/18 EEEE 61 83,5 MUSCARNERA GIUSEPPE MILANO - CADORNA - MILANO - GIUSTI D'ASSISI - MIEE824012 MIEE8C402N DDG 1546/18 EEEE 75 83 SCISCIO VIVIANA CONCETTA MILANO - MOROSINI - MILANO - NOLLI ARQUATI - MIEE8FU03E MIEE8B9015 DDG 1546/18 EEEE 108 82 MILORO RAFFAELLA VARESE CESATE - GIOVANNI XXIII - MIEE8BA02G DDG 1546/18 EEEE 129 81,3 ATRIA ANGELA PIEVE E.- VIQUARTERIO - LOCATE T. - DON MILANI - MIEE88501D MIEE8D5024 DDG 1546/18 EEEE 177 80,1 CAVALLI ANTONIO MILANO - LORIA - MILANO - NARCISI - MIEE8CZ01L MIEE8FX01X DDG 1546/18 EEEE 178 80 GILLIO UMBERTO MILANO - GIACOSA - MILANO - V.LOCCHI - MIEE8CT01C MIEE8DD017 DDG 1546/18 EEEE 187 80 LAQUINTANA CRISTINA MILANO - MAFFUCCI - MILANO -RINNOVATA PIZZIGONI - MIEE8FP01X MIEE8D101Q DDG 1546/18 EEEE 201 80 PEZZUTO BARBARA SESTO - PASCOLI - MILANO -GB PERASSO - MIEE8GH02B MIEE8A014 DDG 1546/18 EEEE 219 79,8 RIZZO ANTONINO MILANO - CARDARELLI - CORSICO - COPERNICO - MIEE88901R MIEE815017 DDG 1546/18 EEEE 226 79,5 PROTO CARLO CORSICO -

Solveig Tosi, Cv Personal Data Born
Solveig Tosi, c.v. Personal data Born: September 20, 1963 in Halden (Norway) Citizenship: Italy Work Address: Department of Earth Science and Environments, University of Pavia, via S. Epifanio 14, 27100 Pavia, Italy Phone: ++39-0382-984870, Fax: ++39-0382-34240 E-mail: [email protected] Fields of Study: fungal ecology and taxonomy, adaptation to cold extreme environments, biological control fungal agents, fungal bioremediation and biofertilization, antifungal activity of natural extracts, science and education. Education and Professional Experience November 2014 – current. Associate Professor, Department of Earth and Environmental Sciences 1998-October 2014. Permanent Researcher, Department of Earth Science and Environments, University of Pavia (Italy) 1991-1998. Technician in the Botanic Garden of Tuscia University (Viterbo, Italy). April 1990 qualification to practise the profession of Biologist. October 1989-October1990. Consultant for a fish farm September1988-February1989. Associate researcher, Biology Institute, Department of Zoology and Marine Chemistry, University of Oslo (Norway), funded by the Research Counsel of Norway. Focus on "Heavy metal concentration in Tmetonix cicada (Crustacea, Amphipoda) and Pandalus borealis (Crustacea, Dacapoda), from Oslo fjord (Norway)", supervisor Prof. M.I.Abdullah. October, 27 1987. B.S. and Masters in Biological Sciences at the University of Rome "La Sapienza" (110/110). Thesis: Teaching: Botany – Course A and B 6 CFU (Biological Science): A.A. 2013/2014 Botany - Course B (Mycology) 3CFU ( Biological Science) .- A.A. 2004/2005; 2005/2006; 2006/2007; 2008/2009; 2009/2010; 2011/2012 Botanic Laboratory 9 CFU (C.L. Experimental and Applied Biology) A. A. 2009/10 ; 2011/2012 Mycology Laboratory 4 CFU (L.S Natural Science) - A.A. -

Breaking up the Global Value Chain: Opportunities and Consequences Advances in International Management
BREAKING UP THE GLOBAL VALUE CHAIN: OPPORTUNITIES AND CONSEQUENCES ADVANCES IN INTERNATIONAL MANAGEMENT Series Editors: (To Volumes 22) Joseph L. C. Cheng and Michael A. Hitt (Volumes 23À30) Timothy M. Devinney, Torben Pedersen and Laszlo Tihanyi Recent Volumes: Volume 14: Edited by M. A. Hitt and J. L. C. Cheng Volume 15: Edited by J. L. C. Cheng and M. A. Hitt Volume 16: Edited by M. A. Hitt and J. L. C. Cheng Volume 17: Edited by Thomas Roehl and Allan Bird Volume 18: Edited by D. L. Shapiro, M. A. Von Glinow and J. L. C. Cheng Volume 19: Edited by M. Javidan, R. M. Steers and M. A. Hitt Volume 20: Edited by Jose´ Antonio Rosa and Madhu Viswanatha Volume 21: Edited by John J. Lawler and Gregory S. Hundley Volume 22: Edited by Joseph L. C. Cheng, Elizabeth Maitland and Stephen Nicholas Volume 23: Edited by Timothy M. Devinney, Torben Pedersen and Laszlo Tihanyi Volume 24: Edited by Christian Geisler Asmussen, Torben Pedersen, Timothy M. Devinney and Laszlo Tihanyi Volume 25: Edited by Laszlo Tihanyi, Timothy M. Devinney and Torben Pedersen Volume 26: Edited by Timothy M. Devinney, Torben Pedersen and Laszlo Tihanyi Volume 27: Edited by Torben Pedersen, Markus Venzin, Timothy M. Devinney and Laszlo Tihanyi Volume 28: Edited by Laszlo Tihanyi, Elitsa R. Banalieva, Timothy M. Devinney and Torben Pedersen Volume 29: Edited by Timothy M. Devinney, Gideon Markman, Laszlo Tihanyi, and Torben Pedersen ADVANCES IN INTERNATIONAL MANAGEMENT VOLUME 30 BREAKING UP THE GLOBAL VALUE CHAIN: OPPORTUNITIES AND CONSEQUENCES EDITED BY TORBEN PEDERSEN Bocconi University, Italy TIMOTHY M. -
Laboratorio Di Ontologia
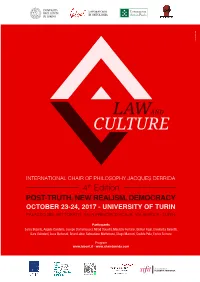
UNIVERSITÀ LABORATORIO DEGLI STUDI DI ONTOLOGIA DI TORINO estroverso.com Società Italiana di FILOSOFIA TEORETICA INTERNATIONAL CHAIR OF PHILOSOPHY JACQUES DERRIDA / LAW AND CULTURE FOURTH EDITION. POST-TRUTH, NEW REALISM, DEMOCRACY October 23rd October 24th Morning session Morning session 9.20 - 10.00 Greetings 10.00 - 10.30 Sanja Bojanic (University of Rijeka) Gianmaria Ajani (Rector, University of Turin) What Mocumentaries Tell Us about Truth? Renato Grimaldi (Director of the Department of Philosophy 10.30 - 11.00 Sebastiano Maffettone (LUISS Guido Carli University) and Educational Sciences, University of Turin) Derrida and the Political Culture of Post-colonialism Pier Franco Quaglieni (Director of Centro Pannunzio, Turin) Tiziana Andina (Director of LabOnt, University of Turin) 11.00 - 11.30 Coffee break 10.00 - 10.20 Prize Award Ceremony 11.30 - 12.00 Elisabetta Galeotti (University of Eastern Piedmont) Maurizio Ferraris (President of LabOnt, University of Turin) Types of Political Deception 10.20 - 11.10 Lectio Magistralis by Günter Figal (University of Freiburg) On Freedom Afternoon session 11.10 - 11.30 Coffee break 14.30 - 15.00 Jacopo Domenicucci (École Normale Supérieure, Paris) The Far We(b)st. Making Sense of Trust in Digital Contexts 11.30 - 12.00 Angela Condello (University of Roma Tre, University of Turin) 15.00 - 15.30 Davide Pala (University of Turin) Post-truth and Socio-legal Studies Citizens, Post-truth and Justice 12.00 - 12.30 Maurizio Ferraris (President of LabOnt, University of Turin) Deconstructing Post-truth 15.30 - 16.00 Break Afternoon session 16.00 - 16.30 Sara Guindani (Fondation Maison des sciences de l’homme, Paris) Derrida and the Impossible Transparency - Aesthetics and Politics 15.00 - 15.30 Luca Illetterati (University of Padua) Post-truth and Authority. -

Table of Contents
Table of Contents Welcome Message from the General Chair.......................................................... 2 M&N 2019 Organizers .......................................................................................... 3 Sponsors .............................................................................................................. 6 Patrons ................................................................................................................. 7 Exhibitors ............................................................................................................ 10 Monday, July 8 ....................................................................................................12 Tuesday, July 9 ................................................... ................................................19 Wednesday, July 10 ........................................................................................... 26 1 Welcome Message from the General Co-Chairs Dear colleagues and friends, On behalf of the entire Conference Committee, we are pleased to welcome you to the 5th IEEE International Symposium on Measurements and Networking (M&N 2019), which is held in Catania and hosted in Museo Diocesano in the heart of the city. The Symposium is mainly promoted by the IEEE IMS TC-37 Measurements and Networking, the IEEE IM Italy Chapter and by the IEEE Italy Section Systems Council Chapter. IEEE M&N is a privileged forum for the discussion of current and emerging trends on measurements, communications, computer science, -

About the Authors
About the Authors Nicola Bellantuono is a Research Fellow in Operations Management at Politecnico di Bari (Italy). He holds a Laurea Degree in Management Engineering (2004) and a PhD in Environmental Engineering (2008). His main research interests deal with exchange mechanisms and coordination schemes for supply chain management, procurement of logistics services, open innovation processes, and corporate social responsibility. Valeria Belvedere is an Assistant Professor in Production and Operations Management at the Department of Management and Technology, Bocconi University, and Professor at the Operations and Technology Management Unit of the SDA Bocconi School of Management. Her main fields of research and publication concern: manufacturing and logistics performance measurement and management; manufacturing strategy; service operations management; and behavioral operations. Elliot Bendoly is an Associate Professor and Caldwell Research Fellow in Information Systems and Operations Management at Emory University’s Goizueta Business School. He currently serves as a senior editor at the Production and Operations Management journal, associate editor for the Journal of Operations Management (Business Week and Financial Times listed journals). Aside from these outlets, he has also published in such widely respected outlets at Information Systems Research, MIS Quarterly, Journal of Applied Psychology, Journal of Supply Chain Management, and Decision Sciences and Decision Support Systems. His research focuses on operational issues in IT utilization and behavioral dynamics in operations management. Stephanie Eckerd is an Assistant Professor at the University of Maryland’s Robert H. Smith School of Business where she teaches courses in supply chain management. Her research uses survey and experiment methodologies to investigate how social and psychological variables affect buyer–supplier relationships. -

Assistenza Domiciliare Integrata ADI Consultori Familiari E Consultori Adolescenti Servizi E Progetti Rivolti Alle Persone Fragili
1 Gli Ospedali Unità Operative Poliambulatori Ospedalieri 1 Presidio Vizzolo Predabissi – Cassano d’Adda Ospedale “Predabissi” Via Pandina 1 – Vizzolo Predabissi Anatomia Patologica Anestesia Rianimazione – Terapia Intensiva Attività Cure Subacuti Cardiologia - UTIC Chirurgia Generale Day Hospital Day Surgery Medicina Generale Nefrologia e Dialisi Neurologia - Stroke Unit Oculistica Oncologia Ortopedia Traumatologia Ostetricia Ginecologia Otorinolaringoiatria Pediatria - Nido Pronto Soccorso Generale Pronto Soccorso Pediatrico Psichiatria - SPDC Urologia Ospedale “Zappatoni” Dietologia e Nutrizione Clinica Via Q. di Vona 41 – Cassano Endoscopia Digestiva d’Adda Farmacia Riabilitazione specialistica: Laboratorio Analisi – SIMT Cardiologica Poliambulatorio Pneumologica Radiologia Neuromotoria Terapia Fisica CAL Blocco Operatorio Centrale di Sterilizzazione Terapia Fisica Piccola Guida al Ricovero Piccola Guida al Ricovero 2 OSPEDALE “PREDABISSI” VIZZOLO PREDABISSI AMBULATORI SPECIALISTICI Allergologia Angiologia Cardiologia Chirurgia Chirurgia Plastica Dermatologia Diabetologia Endocrinologia Nefrologia Neurochirurgia Neurologia Medicina Oculistica Oftalmologia Pediatria Oncologia Ortopedia Ostetricia Ginecologia Otorinolaringoiatria Pediatria Pneumologia Reumatologia Terapia del dolore Urologia OSPEDALE “ZAPPATONI – CASSANO D’ADDA AMBULATORI SPECIALISTICI Allergologia Cardiologia Cure Fisiche Fisiatria Geriatria Oculistica Ortopedia Otorinolaringoiatria Pneumatologia 3 Presidio Cernusco sul Naviglio – Vaprio d’Adda Ospedale “Uboldo” -

Erasmus+ Call 21/22
ERASMUS+ PROGRAMME STUDY IN EUROPE FOR THE ACADEMIC YEAR 2021/2022 APPLICATION WINDOW: FROM THE 5TH TO THE 26TH OF FEBRUARY 2021, AT 13:00 (1 PM) 1. WHAT IS THE ERASMUS+ PROGRAMME ......................................................................... 1 2. WHO CAN APPLY................................................................................................................ 2 3. LEARNING AGREEMENT AND TRANSFER CREDITS ...................................................... 3 4. LANGUAGE SKILLS ............................................................................................................. 4 5. ENROLMENT AND DEADLINE ........................................................................................... 5 6. SELECTION PROCESS ......................................................................................................... 6 7. ERASMUS+ MOBILITY GRANT ........................................................................................... 8 8. MINISTRY- AND UNIVERSITY-FUNDED SUPPLEMENTARY GRANT ............................. 9 9. FOREIGN LANGUAGE COURSES ..................................................................................... 10 10. STUDENTS WITH SPECIAL NEEDS ................................................................................. 11 11. PERSONAL DATA PROCESSING ...................................................................................... 11 ANNEXE A PLEASE NOTE: the present Call is to be considered under condition; specifically, the publication of the call for funding and -

Creating Value in the Entrepreneurial University: Marketization and Merchandising Strategies
administrative sciences Article Creating Value in the Entrepreneurial University: Marketization and Merchandising Strategies Chiara Fantauzzi *, Rocco Frondizi , Nathalie Colasanti and Gloria Fiorani Department of Management and Law, University of Rome Tor Vergata, 00133 Roma, Italy; [email protected] (R.F.); [email protected] (N.C.); gloria.fi[email protected] (G.F.) * Correspondence: [email protected] Received: 9 August 2019; Accepted: 14 October 2019; Published: 18 October 2019 Abstract: Higher education institutions are called to expand their role and responsibilities, by enhancing their entrepreneurial mindset and redefining relationships with stakeholders. In order to cope with these new challenges, they have started to operate in a strategic manner, by performing marketing and merchandising activities. Indeed, in a sector characterized by the presence of competitive funding models, several forms of accountability, and performance indicators, universities have become open systems and have started to operate like enterprises, considering students as customers. Given this premise, the aim of the paper is to individuate marketing and merchandising strategies in higher education and to evaluate their effectiveness in order to foster stakeholders engagement. This is in line with the entrepreneurial university model that represents the starting point of the theoretical study, then a literature review of “marketization” in higher education institutions is presented, showing how this field is not yet completely investigated. Data refer to the Italian context and are analyzed through a qualitative method. Findings suggest that most Italian universities perform merchandising strategies, but currently there is not sufficient information to evaluate their effectiveness in higher education, it was only possible to make hypotheses. -

67Th Economic Policy Panel
67th Economic Policy Panel Hosted by the Swiss National Bank Venue: Great Guild Hall, 2nd Floor, Zunfthaus zur Zimmerleuten Limmatquai 40, 8001 Zurich, Switzerland 12-13 April 2018 Programme Each session is 70 minutes in duration Author: 25 mins | Discussant: 15 mins (each) | Panel discussion: 15 mins * indicates presenting author Thursday 12 April 14:00 Registration and coffee on arrival 14:30 – 14:45 Opening Remarks Mr Thomas Moser, Alternate Member of the Governing Board, Swiss National Bank 14:45 – 15:55 Can Education Compensate the Effect of Population Aging on Macroeconomic Performance? Evidence from Panel Data Rainer Kotschy (LMU Munich) * Uwe Sunde (LMU Munich) Discussants: Francesco Drago (University of Messina) Pietro Biroli (University of Zurich) 15:55 – 17:05 Monetary Policy and Bank Profitability in a Low Interest Rate Environment * Carlo Altavilla (European Central Bank) Miguel Boucinha (European Central Bank) José-Luis Peydró (ICREA-UPF, CREI & BGSE) Discussants: Ralph De Haas (EBRD) Vasso Ioannidou (University of Lancaster) 17:05 – 17:20 coffee break 17:20 – 18:30 The Walking Dead?: Zombie Firms and Productivity Performance in OECD Countries Müge Adalet McGowan (OECD) Dan Andrews (OECD) * Valentine Millot (OECD) Discussants: Martin Brown (University of St.Gallen) Elena Carletti (Bocconi University) 20:00 Conference dinner at The Ballroom of the Savoy Hotel Baur en Ville Address: Poststrasse 12, 8001 Zurich Welcome address by Ms Andréa M. Maechler, Member of the Governing Board, Swiss National Bank Friday 13 April 08:30 – 09:40 Where Do People Get Their News? * Patrick Kennedy (Columbia University) Andrea Prat (Columbia University) Discussants: Roberto Galbiati (Sciences Po) David Hémous (University of Zurich) 09:40 – 10:50 Populism and Civil Society * Tito Boeri (Bocconi University) Prachi Mishra (IMF) Chris Papageorgiou (IMF) Antonio Spilimbergo (IMF) Discussants: Christina Gathmann (Heidelberg University) 10:50 – 11:10 Coffee break 11:10 – 12:20 The Gains from Economic Integration David Comerford (University of Strathclyde) * José V. -

Isu Bocconi Housing Application Requirements and Regulations
ISU BOCCONI HOUSING APPLICATION REQUIREMENTS AND REGULATIONS BOCCONI UNIVERSITY 2018-2019 A/Y FINAL REGULATIONS These Application Requirements and Regulations are to be considered final unless further dispositions concerning the evaluation of the applicants’ economic condition are issued by the relevant authorities. Student Affairs Division ISU Bocconi Fees, Funding and Housing Office Centro per il Diritto allo Studio Universitario TABLE OF CONTENTS SECTION 1: GENERAL INFORMATION 1.1 List of Bocconi Residence Halls for A/Y 2018-19 1.2 Housing rates 1.3 Who may reside in Bocconi Residence Halls 1.4 General access and cohabitation rules SECTION 2: HOUSING RENEWAL 2.1 REDUCED RATE: RENEWAL APPLICATION 2.1.1 Requirements for submitting application 2.1.2 Timescales and methods for submitting application and necessary documentation 2.1.3 Publication of outcomes and assignment 2.2 FULL RATE: RENEWAL APPLICATION 2.2.1 Requirements for submitting application 2.2.2 Timescales and methods for submitting application 2.2.3 Publication of outcomes and assignment SECTION 3: NEW HOUSING ADMISSION – FIRST ASSIGNMENTS 3.1 REDUCED RATE: NEW ADMISSION APPLICATION FOR FIRST YEAR STUDENTS AND LATER YEARS 3.1.1 Requirements for submitting application 3.1.2 Timescales and methods for submitting application and documentation 3.1.3 Publication of outcomes and assignment 3.1.4 Housing renewal criteria from A/Y 2019-20 3.2 FULL RATE: NEW ADMISSION APPLICATION FOR FIRST YEAR STUDENTS 3.2.1 Requirements for submitting application 3.2.2 Timescales and methods for submitting