Project Information Document (PID)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MONUSCO, 20 Years in Democratic Republic of Congo. What
MONUSCO, 20 Years in Democratic Republic of Congo. What Are the Priorities For Its New Mandate? Analysis December 2019 / N° 746a Cover picture: The gates to the MONUSCO headquarters in Kinshasa, Democratic Republic of Congo (DRC), 19 February 2015. © Michael Kappeler / DPA/DPA Picture Alliance TABLE OF CONTENTS ACRONYMS 5 MAP OF MONUSCO’S PRESENCE IN DRC 6 EXECUTIVE SUMMARY 7 METHODOLOGY 9 INTRODUCTION 10 I. OVERVIEW OF THE POLITICAL, SECURITY AND HUMAN RIGHTS CONTEXT IN DRC 12 A. An uncertain context of emergence from political crisis and lifting of restrictions on democratic space 12 B. A worrying security context, marked by continuing violations of human rights and inter-communal tensions and conflicts throughout the country 14 II. OVERVIEW OF THE CONTEXT OF RENEWAL OF MONUSCO’S MANDATE 18 A. A nine-month interim mandate 18 B. Towards MONUSCO’s reconfiguration 19 III. PRIORITIES FOR THE NEW MONUSCO MANDATE ACCORDING TO FIDH AND ITS MEMBER ORGANISATIONS IN DRC 21 A. On democratic space and governance 21 1. Consolidate efforts already undertaken to open up democratic space 21 2. Encourage institutional reforms 22 B. On security and civilian protection 24 1. Prioritise a non-military community-based and local approach to civilian protection 24 2. Strengthen civil and military coordination 25 3. Provide a rapid response to protection needs 26 4. Adopt a regional approach to civilian protection 26 5. Pursue efforts to reform the UN peacekeeping system 26 C. On justice and the fight against impunity 27 1. Fight impunity for the most serious crimes 27 2. Build the capacities of the judicial system to increase its efficiency and independence 29 3. -

Report Ondemocratic Republic of Congo Seed Systems
i ii REPORT ON DEMOCRATIC REPUBLIC OF CONGO SEED SYSTEMS DEMOCRATIC REPUBLIC OF CONGO OCTOBER 2019 Professor ASANZI Christophe National Consultant iii TABLE OF CONTENTS TABLE OF CONTENTS ............................................................................................................................ i LIST OF TABLES ................................................................................................................................... iiv LIST OF ACRONYMS ............................................................................................................................ vv INTRODUCTION AND BACKGROUND .................................................................................................. 1 a. Agricultural production systems ............................................................................................. 1 b. Current and recent initiatives in agricultural development .................................................... 3 c. Scope for the development of agriculture .............................................................................. 3 I. CROP PRODUCTION SYSTEMS ..................................................................................................... 3 1.1. Current crop production levels of major staple food crops, average crop yields, and trends, by crop ............................................................................................................................ 4 1.2. Description of the country's main agro-ecological zones and their production systems -

DRC), AFRICA | Ebola Virus Disease Outbreak
OPERATION UPDATE Democratic Republic of the Congo (DRC), AFRICA | Ebola Virus Disease outbreak Appeal №: n° Operations Update n° 8 Timeframe covered by this update: MDRCD026 Date of issue: 12 March 2020 34 months (May 2018 –February 2021) Operation start date: 21 May 2018 Operation timeframe: 34 months (May 2018 –February 2021) Glide №: Overall operation budget: CHF 56 One International Appeal amount EP-2018-000049-COD million initially allocated: CHF 500,000 + CHF EP-2018-000129-COD Budget Coverage as of 08 March 2021: 300,000 (Uganda) EP-2020-000151-COD CHF46.8m (84%) EP-2021-000014-COD Budget Gap: CHF9.2m (16%) N° of people to be assisted: 8.7 million people Red Cross Red Crescent Movement partners currently actively involved in the operation: In addition to the Democratic Republic of Congo Red Cross (DRC RC), the International Federation of Red Cross and Red Crescent Societies (IFRC), the International Committee of the Red Cross (ICRC) there is also French Red Cross and other in- country partner National Societies (Belgium Red Cross, Spanish Red Cross and Swedish Red Cross) and other Partner National Societies who have made financial contributions (American, British, Canadian, Finnish, Icelandic, Norwegian, Swedish, Swiss). Other partner organizations actively involved in the operation: Alongside these Movement partners, other national and international organizations are directly involved in the response to the Ebola epidemic. These include the Ministry of Health of the Democratic Republic of Congo, WHO, UNICEF, MSF, Oxfam, Personnes vivant avec Handicap (PVH), Soutien action pour le développement de l’Afrique (SAD Africa), AMEF, ASEBO, MND, Humanitarian Action, Ministry of Primary and Secondary Education (EPSP), Border Hygiene, IMC, The Alliance for International Medicine Action (ALIMA), IRC, Caritas, Mercy Corps, FHI 360, Africa CDC, CDC Atlanta, Foreign, Commonwealth and Development Office (FCDO formerly DFID), OIM and the World Bank. -

Survey on the Production of Traditional Bioenergy in the Democratic Republic of the Congo: the Case Study of Kwilu Province
Britain International of Exact Sciences (BIoEx) Journal ISSN: 2686-1208 (Online), 2686-1216 (Print) Vol. 2, No. 3, September 2020, Page: 609-614 Survey on the Production of Traditional Bioenergy in the Democratic Republic of the Congo: The Case Study of Kwilu Province Masens Da-Musa Y.B.1*, Koto-te-Nyiwa Ngbolua2, Briki C. Kakesa3, Muhammad Ridwan4 1,2Department of Biology, Faculty of Science, University of Kinshasa, Kinshasa, Democratic Republic of the Congo 2Department of Environment, Faculty of Science, University of Gbado-Lite, Gbado-Lite, Democratic Republic of the Congo 3University of Kikwit, Kikwit, Democratic Republic of the Congo 4Universitas Islam Negeri Sumatera Utara, Indonesia Abstract: The present research has been carried out in three different groupings, namely Mudikwiti, Tanganga and Nkata in Kwilu province, in the Democratic Republic of the Congo. 165 coalmen from eighteen villages have been considered as the sample used in this work. They are selected from all social strata, and their ages vary from 18 to 30 years old and from 44 to 56 years old. They have made 21,899 ovens, among which there were 12, 287 ovens of small dimensions, that is, 1 m x 6 m x 3 m, and 9,612 ovens of big dimensions: 6 m x 20 m x 3 m. They have cut 196,694 trees of different species to fill in the two kinds of ovens, say 99,984 trees for filling in small ovens and 96,710 trees to fill in big ovens. On the whole, they have produced 852,708 sacks of charcoal per year. -

Emergency Plan of Action Operations Update: Democratic Republic of the Congo (DRC) Ebola Virus Disease Outbreak
P a g e | 1 Emergency Plan of Action Operations Update: Democratic Republic of the Congo (DRC) Ebola Virus Disease outbreak GLIDE n°: EP-2018-000049-COD One International Appeal n° MDRCD026 EP-2018-000129-COD EP-2020-000151-COD Operations Update n° 7 Timeframe covered by this update: 32 Date of issue: 02 February 2021 months (May 2018 – December 2020) Operation timeframe: end date 30 June Operation start date: 21 May 2018 2021 OIA amount initially allocated: CHF Overall operation budget: CHF 56 million 500,000 + CHF 300,000 (Uganda) N° of people to be assisted: 8.7 million people Red Cross Red Crescent Movement partners actively involved in the operation: In addition to the Democratic Republic of Congo Red Cross (DRC RC), the International Federation of Red Cross and Red Crescent Societies (IFRC), the International Committee of the Red Cross (ICRC) there is also French Red Cross and other in-country partner National Societies (Belgium Red Cross, Spanish Red Cross and Swedish Red Cross) and other Partner National Societies who have made financial contributions (American, British, Canadian, Finnish, Icelandic, Norwegian, Swedish, Swiss). Alongside these Movement partners, other national and international organizations are directly involved in the response to the Ebola epidemic. These include the Ministry of Health of the Democratic Republic of Congo, WHO, UNICEF, MSF, Oxfam, Personnes vivant avec Handicap (PVH), Soutien action pour le développement de l’Afrique (SAD Africa), AMEF, ASEBO, MND, Humanitarian Action, Ministry of Primary and Secondary Education (EPSP), Border Hygiene, IMC, The Alliance for International Medicine Action (ALIMA), IRC, Caritas, Mercy Corps, FHI 360, Africa CDC, CDC Atlanta, Foreign, Commonwealth and Development Office (FCDO formerly DFID), OIM and the World Bank. -

Democratic Republic of the Congo 17 April 2020
UPDATE ON COVID-19 RESPONSE Democratic Republic of the Congo 17 April 2020 Main highlights As of 16 April, there were 287 confirmed cases of COVID-19 in the DRC, with 23 reported deaths. No case has been detected amongst UNHCR’s persons of concern in the DRC so far. The Ebola epidemic continues: two individuals died of the disease just days before the declaration of the end of the epidemic in DRC was to be declared on 12 April. On 3 April, UNHCR and partner INTERSOS launched a mobile money cash distribution using a hopscotch game to promote social distancing for nearly 6,000 internally displaced persons (IDPs) living in Beni and Butembo towns, North Kivu Province. The use of mobile money is a way to reduce direct contact amidst the COVID-19 pandemic. In Kinshasa, 238 urban refugees, including 57 with specific needs, received either cash assistance to supplement their food rations, or assistance to buy food provisions, as a response to restrictions in place amidst COVID-19. A displaced woman receives cash assistance from UNHCR through mobile money in Beni, North Kivu Province, amidst the COVID-19 pandemic. © UNHCR/Ibrahima Diane Operational context On 6 April, the capital Kinshasa’s Gombe commune, which is the epicenter of COVID-19 in the country, went into a total lockdown until at least 20 April, whereby inhabitants cannot leave their homes. For the same period, all outward movements from Goma, Beni and Butembo towns (North Kivu Province) have been suspended. Lastly, all movements between Goma and Bukavu (South Kivu Province) are suspended. -

Emergencies Preparedness, Response Monkeypox – Democratic Republic of the Congo
Emergencies preparedness, response Monkeypox – Democratic Republic of the Congo Disease outbreak news 1 October 2020 From 1 January through 13 September 2020, a total of 4,594 suspected cases of monkeypox, including 171 deaths (case fatality ratio 3.7%), have been reported in 127 health zones from 17 out of 26 provinces in the Democratic Republic of the Congo. The first epidemic peak was observed at the beginning of March 2020 (epi week 10), with 136 cases reported weekly (Figure1). From 1 January through 7 August, the Institut National de Recherche Biomédicale (INRB) received 80 samples from suspected cases of monkeypox, of which 39 samples were confirmed positive by polymerase chain reaction. Four out of the 80 specimens were skin lesions (crusts/vesicles), the remaining samples were blood. There is no further information at this time regarding the outcome of these 80 patients whose samples were tested. Confirmatory testing remains ongoing. During the same period in 2019, 3,794 suspected cases and 73 deaths (CFR 1.9%) were reported in 120 health zones from 16 provinces while a total of 2,850 suspected cases (CFR 2.1%) were reported in 2018. Figure 1: Distribution of suspected cases of monkeypox and case fatality ratio, by epi week, from 1 January 2019 through 13 September 2020. Enlarge image The provinces reporting the highest number of suspected cases include Sankuru with 973 (21.2%) suspected cases, Mai-Ndombe with 964 (21%) suspected cases, Equateur with 586 (12.8%) suspected cases, Tshuapa with 520 (11.3%) suspected cases and Mongala with 518 (11.3%) suspected cases (Figure 2). -
Cod200506.Fe
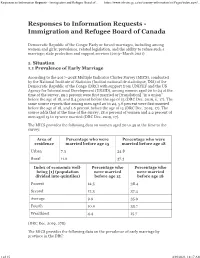
Responses to Information Requests - Immigration and Refugee Board of... https://www.irb-cisr.gc.ca/en/country-information/rir/Pages/index.aspx?... Democratic Republic of the Congo: Early or forced marriages, including among women and girls; prevalence, related legislation, and the ability to refuse such a marriage; state protection and support services (2019–March 2021) 1. Situation 1.1 Prevalence of Early Marriage According to the 2017–2018 Multiple Indicator Cluster Survey (MICS), conducted by the National Institute of Statistics (Institut national de statistique, INS) of the Democratic Republic of the Congo (DRC) with support from UNICEF and the US Agency for International Development (USAID), among women aged 20 to 24 at the time of the survey, 29.1 percent were first married or [translation] “in a union” before the age of 18, and 8.4 percent before the age of 15 (DRC Dec. 2019, ii, 17). The same source reports that among men aged 20 to 24, 5.6 percent were first married before the age of 18, and 1.6 percent before the age of 15 (DRC Dec. 2019, 17). The source adds that at the time of the survey, 18.0 percent of women and 2.2 percent of men aged 15 to 19 were married (DRC Dec. 2019, 17). The MICS provides the following data on women aged 20 to 49 at the time to the survey: Area of Percentage who were Percentage who were residence married before age 15 married before age 18 Urban 7.3 24.8 Rural 11.6 37.3 Index of economic well- Percentage who Percentage who being [1] (population were married were married divided into quintiles) before age 15 before age 18 Poorest 12.5 38.4 Second 12.3 37.4 Average 9.9 35.9 Fourth 10.0 33.7 Wealthiest 4.4 15.7 (DRC Dec. -

Coronavirus (COVID-19) Situation Report # 4
DEMOCRATIC REPUBLIC OF CONGO Coronavirus (COVID-19) Situation Report # 4 Reporting period: 3 to 10 April 2020 Current situation – key figures (DRC Ministry of Health & World Health Organization) KEY FIGURES AND FACTS As of 10 April 2020, there are: 215 confirmed cases in DRC • 223 confirmed cases • 20 deaths 1,521,252 confirmed cases globally • 10 per cent Case Fatality Ratio (CFR) • 16 persons recovered • 104 suspected cases under investigation 20 deaths in DRC • 139 patients progressing well • 39 being treated in hospital 10% Case Fatality Rate (CRF) in DRC • 5 provinces affected : Kinshasa, Nord Kivu, Sud Kivu, Ituri, 92,798 deaths globally Kwilu • 29 health zones affected 16 people recovered in DRC The province of Kinshasa continues to register the vast majority of 376,102 people recovered confirmed cases (94,2%). globally A total of 1,258 contacts were followed up as of 08/04/2020; 56 percent (n=700) of these were seen in the last 24 hours. On 08/04/2020, 143 confirmed cases were being treated, 39 of which were in health facilities and 104 at home. Of the 104 confirmed cases at home, 68 are being transferred to health facilities. 56 per cent of contacts were followed up. 48 per cent of travelers were followed up. 78 per cent of alerts were investigated in the last 24 hours. 68.9 per cent of cases were male (126/183), which equals a sex ratio M/F of 2.3. Ten health workers were among the 126 confirmed cases for which information was available, which is equivalent to 7.9 per cent of all infections. -

United Nations Organization Stabilization Mission in the Democratic Republic of the Congo
United Nations S/2019/575 Security Council Distr.: General 17 July 2019 Original: English United Nations Organization Stabilization Mission in the Democratic Republic of the Congo Report of the Secretary-General I. Introduction 1. The present report, submitted pursuant to paragraph 46 of Security Council resolution 2463 (2019), covers major developments in the Democratic Republic of the Congo from 8 March to 28 June 2019. The report describes progress in the implementation of the mandate of the United Nations Organization Stabilization Mission in the Democratic Republic of the Congo (MONUSCO) since my report of 7 March 2019 (S/2019/218); provides an overview of political developments; outlines progress in adjustments to the Mission’s priorities, posture and presence, as well as the pursuit of its comprehensive approach to the protection of civilians; and provides information on the performance of MONUSCO uniformed personnel. II. Political developments 2. Following the peaceful transition of power in the Democratic Republic of the Congo on 24 January 2019, national and provincial legislative and executive institutions were installed in accordance with the Constitution. The return of opposition leaders to the Democratic Republic of the Congo contributed to evolving dynamics in the emerging balance of power among the country’s political forces. The President, Félix Tshisekedi, pursued his initiatives aimed at strengthening bilateral and regional cooperation, implementing the national emergency programme, opening the political space and improving the security situation in the country. 3. On 20 May, Sylvestre Ilunga was appointed Prime Minister by the President. The new Prime Minister served in various senior capacities under former President Mobutu Sese Seko and was, until his appointment, the Director General of the Société nationale des chemins de fer du Congo. -

Assessing the Impact of Data Aggregation in Model Predictions of HAT Transmission and Control Activities
medRxiv preprint doi: https://doi.org/10.1101/19005991; this version posted October 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY 4.0 International license . Assessing the impact of data aggregation in model predictions of HAT transmission and control activities M. Soledad Casta~no1,2*, Martial L. Ndeffo-Mbah3,4, Kat S. Rock5,6, Cody Palmer7, Edward Knock5,8, Erick Mwamba Miaka9, Joseph M. Ndung'u10, Steve Torr11, Paul Verl´e12, Simon E.F. Spencer5,8, Alison Galvani3, Caitlin Bever7, Matt J. Keeling5,6, Nakul Chitnis1,2 1 Department of Epidemiology and Public Health, Swiss Tropical and Public Health Institute, Basel, Switzerland 2 University of Basel, Basel, Switzerland 3 School of Public Health, Yale University, New Haven, Connecticut, USA 4 College of Veterinary Medicine and Biosciences, Texas A&M University, College Station, Texas, USA 5 Zeeman Institute for Systems Biology and Infectious Disease Epidemiology Research, University of Warwick, Coventry, UK 6 Mathematics Institute, University of Warwick, Coventry, UK 7 Institute of Disease Modeling, Seattle, Washington, USA 8 Department of Statistics, University of Warwick, Coventry, UK 9 Programme National de Lutte contre la Trypanosomiase Humaine Africaine, Kinshasa, the Democratic Republic of the Congo 10 Foundation for Innovative New Diagnostics, Geneva, Switzerland 11 Department of Vector Biology, Liverpool School of Tropical Medicine, Liverpool, UK 12 Department of Public Health, Institute of Tropical Medicine, Antwerp, Belgium *[email protected] (MSC) 1/27 NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. -

COVID-19 Situation Report
UNICEF DRC | COVID-19 Situation Report COVID-19 Chudeau - Situation Report #16 /Rice 23 September 2020 - UNICEF 21 October 2020 © Highlights COVID-19 overview (as of 19 October 2020) • More than 8 million children have access to distance learning thanks to partnerships with 322 radio stations and 23 TV channels 11,078 confirmed cases • 1.2 million community masks distributed 303 deaths • 25 million people reached with key messages on how to prevent COVID-19 through mass media channels (300 radio stations and 50 TV channels) people 10,337 recovered • 64,283 calls managed by the COVID-19 Hotline 2.7 % Fatality Rate • 71,532 people (including 21,415 children) affected by COVID-19 and 6,005 frontline workers provided with psychosocial support since the beginning of Kinshasa recorded 74% (8,290) of all confirmed cases. Other the epidemic affected provinces including # of cases are: North Kivu (1,069) Haut Katanga (344) Kongo Central UNICEF’s COVID-19 Response (524) South Kivu (318) Ituri (178) Lualaba (120) Haut Uele (90) Tshopo (56) North Ubangi (37) # of people reached on COVID-19 through Kwilu (6) Equateur (20) South 86% messaging on prevention and access to… Ubangi (7) Tanganyika (6) Kwango RCCE* (1) Haut Lomami (1) Kasai (1) Kasai # of people reached with critical WASH Central (1) Maniema (2) Kasai 162% supplies (including hygiene items) and… IPC** Oriental (4) Tshuapa (1) # of children who are victims of violence, 72% DRC COVID-19 including GBV, abuse, neglect or living… PSS*** Response Funding Status # of children and women receiving essential 46% healthcare services in UNICEF supported… Health Funding Gap # of caregivers of children (0-23 months) 34% DRC COVID-19 n 75% Funding reached with messages on breadstfeeding… requirements* : Nutritio $ 58,036,209 # of children supported with Funds n 53% available* distance/home-based learning 66% Educatio 0% 20% 40% 60% 80%100%120%140%160%180% * Funds available include 9 million USD UNICEF regular resources allocated by the office for first response needs.