The Annual Report 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Somrat Vol. 11 No. 1 Page 21-32.Pmd
Asian Biomedicine Vol. 11 No. 1 February 2017; 21 - 32 DOI: 10.5372/1905-7415.1101.535 Original article Perioperative and Anesthetic Adverse events in Thailand (PAAd Thai) incident reporting study: anesthetic profiles and outcomes Somrat Charuluxananan1, Wimonrat Sriraj2, Yodying Punjasawadwong3, Siriporn Pitimana-aree4, Varinee Lekprasert5, Thewarug Werawatganon1, Wirat Wasinwong6, Prapa Ratanachai7, Dujduen Sriramatr8, Sunida Atichat9, Wanna Angkasuvan7, Chuthamat Somchat10, Duangporn Tanutanud11, Thidarat Ariyanuchitkul12, Jaroonpong Choorat13, Krairerk Sintavanuruk14, Jeratkana Janngam15 1Department of Anesthesiology, Faculty of Medicine, Chulalongkorn University, Bangkok 10330, Thailand 2Department of Anesthesiology, Faculty of Medicine, Khon Kaen University, Khon Kaen 40000, Thailand 3Department of Anesthesiology, Faculty of Medicine, Chiang Mai University, Chiang Mai 50200, Thailand 4Department of Anesthesiology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand 5Department of Anesthesiology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok 10400, Thailand 6Department of Anesthesiology, Faculty of Medicine, Prince of Songkla University, Songkhla 90110, Thailand 7Department of Anesthesiology, Hatyai Hospital, Songkhla 90110, Thailand 8Department of Anesthesiology, Faculty of Medicine, Srinakharinwirot University, Nakhon Nayok 26120, Thailand 9Department of Anesthesiology, Chonburi Regional Hospital, Chonburi 20000, Thailand 10Department of Anesthesiology, Lamphun Hospital, Lamphun -
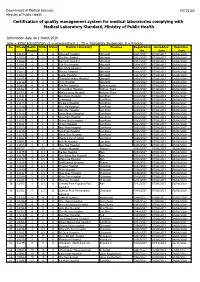
Certification of Quality Management System for Medical Laboratories Complying with Medical Laboratory Standard, Ministry of Public Health
Department of Medical Sciences F0715102 Ministry of Public Health Certification of quality management system for medical laboratories complying with Medical Laboratory Standard, Ministry of Public Health Information date on 1 March 2019 new = initial accreditation, r1 = reassessment 1 , TS = Temporary Suspension, P = Process No. HCode Health RMSc Status Medical Laboratory Province Registration Accredited Expiration Region No. Date Date 1 10673 2 2 r1 Uttaradit Hospital Uttaradit 0001/2557 07/08/2017 06/08/2020 2 11159 2 2 r1 Tha Pla Hospital Uttaradit 0002/2557 07/08/2017 06/08/2020 3 11160 2 2 r1 Nam Pat Hospital Uttaradit 0003/2557 07/08/2017 06/08/2020 4 11161 2 2 r1 Fak Tha Hospital Uttaradit 0004/2557 07/08/2017 06/08/2020 5 11162 2 2 r1 Ban Khok Hospital Uttaradit 0005/2557 07/08/2017 06/08/2020 6 11163 2 2 r1 Phichai Hospital Uttaradit 0006/2557 07/08/2017 06/08/2020 7 11164 2 2 r1 Laplae Hospital Uttaradit 0007/2557 07/08/2017 06/08/2020 8 11165 2 2 r1 ThongSaenKhan Hospital Uttaradit 0008/2557 07/08/2017 06/08/2020 9 11158 2 2 r1 Tron Hospital Uttaradit 0009/2557 07/08/2017 06/08/2020 10 10863 4 4 r1 Pak Phli Hospital Nakhonnayok 0010/2557 07/08/2017 06/08/2020 11 10762 4 4 r1 Thanyaburi Hospital Pathum Thani 0011/2557 07/08/2017 06/08/2020 12 10761 4 4 r1 Klong Luang Hospital Pathum Thani 0012/2557 07/08/2017 06/08/2020 13 11141 1 1 P Ban Hong Hospital LamPhun 0014/2557 07/08/2014 06/08/2017 14 11142 1 1 P Li Hospital LamPhun 0015/2557 07/08/2014 06/08/2017 15 11144 1 1 P Pa Sang Hospital LamPhun 0016/2557 07/08/2014 06/08/2017 -

Cover Tjs 35-4-57
ISSN 0125-6068 TheThai Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand www.surgeons.or.th/ejournal Volume 35 October-December 2014 Number 4 ORIGINAL ARTICLES 121 Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, Porn Narischart 126 Open Surgical Management of Atherosclerotic Aortoiliac Occlusive Diseases (AIOD) Type 1 Anuwat Chantip 130 “Sawanpracharak” Connector: A Single Tube Intercostal Drainage Connector Wanchai Manakijsirisuthi 134 The Trainee’s Operative Experiences for General Surgery in Thailand Potchavit Aphinives CASE REPORT 139 Mitral and Tricuspid Valve Replacement in Uncommon Case of Situs Inversus with Dextrocardia Nuttapon Arayawudhikul, Boonsap Sakboon, Jareon Cheewinmethasiri, Angsu Chartirungsun, Benjamaporn Sripisuttrakul ABSTRACTS 143 Abstracts of the 39th Annual Scientific Congress of the Royal College of Surgeons of Thailand, 10-13 July 2014, Ambassador City Jomtien Hotel, Jomtien, Pattaya, Cholburi, Thailand (Part II) 169 Index Secretariat Office : Royal Golden Jubilee Building, 2 Soi Soonvijai, New Petchaburi Road, Huaykwang, Bangkok 10310, Thailand Tel. +66 2716 6141-3 Fax +66 2716 6144 E-mail: [email protected] www.surgeons.or.th The THAI Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand Vol. 35 October - December 2014 No. 4 Original Article Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, MD Porn Narischart, MD Prasat Neurological Institute, Department of Medical Services, Ministry of Pubic Health, Bangkok, Thailand Abstract Background and Objective: Hydrocephalus is a common problem in neurosurgical field. In current clinical practice guidelines, ventriculoatrial shunt and ventriculoperitoneal shunt are recommended treatment options. No previous study reported differences between two procedures in term of complications and revision rates. -

Case Study, Thailand
Health Guidelines for Vegetation Fire Events, Lima, Peru, 6-9 October 1998. Background papers © WHO, 1999 SMOKE EPISODES EMISSIONS CHARACTERIZATION AND ASSESSMENT OF HEALTH RISKS RELATED TO DOWNWIND AIR QUALITY - CASE STUDY, THAILAND Kanchanasak Phonboon, Oranut Paisarn-uchapong, Proespichaya Kanatharana, Songkran Agsorn Environment and Health Program Health Systems Research Institute 5th Floor, Mental Health Bldg Tiwanon Rd, Nonthaburi 11000 Thailand INTRODUCTION With abnormally dry conditions from the 1997-98 El Niño/Southern Oscillation (ENSO) episode, widespread uncontrolled forest fires (originally as part of land clearing operations) occurred since June 1997 in Irian Jaya, Kalimantan (Borneo), Sulawesi, and Sumatra of Indonesia, a country in the South-East Asia region (1). Approximately one million hectares of forest were ablaze when most of the fires subsided three months later in November. From September, the thick haze due to fine particles suspended in the air from smoke and soot had darkened skies across the region—Malaysia, Indonesia, Singapore, Brunei, southern Thailand and parts of the Philippines. Indonesia declared a state of national emergency in September 1997. The Malaysian Government also declared a state of emergency in Sarawak on Borneo Island on 19 September. All private and public offices and schools in Sarawak were closed and the people advised to stay indoors. An increase in the number of people who required clinic (outpatient) visits or hospital admissions for various haze-related illnesses was reported from Malaysia, Singapore, and Thailand. More than 20,000 cases were reported from Malaysia, a surge of 20 percent was recorded in Singapore, and 334 Health Guidelines for Vegetation Fire Events, Lima, Peru, 6-9 October 1998. -

วารสาร พยาบาลสาร Nursing Journal ปีที่ 47 ฉบับที่ 1 มกราคม-มีนาคม พ.ศ
พยาบาลสาร : Nursing Journal คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ วารสาร พยาบาลสาร Nursing Journal ปีที่ 47 ฉบับที่ 1 มกราคม-มีนาคม พ.ศ. 2563 • Volume 47 No.1 January-March 2020 ISSN 0125-5118 ที่ปรึกษา (Consultant) ศาสตราจารย์ ดร.วิภาดา คุณาวิกติกุล คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Wipada Kunaviktikul, PhD, RN, FAAN Faculty of Nursing, Chiang Mai University ผู้ช่วยศาสตราจารย์ ดร.จุฑารัตน์ มีสุขโข คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Jutarat Mesukko, PhD, RN Faculty of Nursing, Chiang Mai University ที่ปรึกษากองบรรณาธิการ (Editorial Advisors) ศาสตราจารย์เกียรติคุณ ดร.วิจิตร ศรีสุพรรณ อดีตนายกสภาการพยาบาล Wichit Srisuphan, DrPH, RN Professor ศาสตราจารย์ ดร.ประนอม โอทกานนท์ ศาสตราจารย์ Pranom Othagnont, RN, M.E.D.,Ed.D. Professor ศาสตราจารย์ ดร.สมจิต หนุเจริญกุล ศาสตราจารย์ Somchit Hanucharurnkul, PhD, RN Professo บรรณาธิการ (Editor) ศาสตราจารย์ ดร. อารีวรรณ กลั่นกลิ่น คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Areewan Klunklin, PhD, RN Faculty of Nursing, Chiang Mai University รองบรรณาธิการ (Associate Editor) รองศาสตราจารย์ ดร.นันทพร แสนศิริพันธ์ คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Nantaporn Sansiriphun, PhD, RN, APN Faculty of Nursing, Chiang Mai University กองบรรณาธิการ (Editorial Board) ศาสตราจารย์ ดร.รุจา ภู่ไพบูลย์ คณะพยาบาลศาสตร์ มหาวิทยาลัยมหิดลศาสตราจารย์ Rutja Phuphaibul, DNS, RN Faculty of Nursing, Mahidol University ศาสตราจารย์ ดร.วีณา จีระแพทย์ คณะพยาบาลศาสตร์ จุฬาลงกรณ์มหาวิทยาลัย Veena Jirapaet, PhD, RN Faculty of Nursing, Chulalongkorn University ศาสตราจารย์ ดร.วารุณี ฟองแก้ว คณะพยาบาลศาสตร์ มหาวิทยาลัยเชียงใหม่ Warunee Fongkaew, -

Blood Group Genomics
BLOOD GROUP GENOMICS Matrix-assisted laser desorption/ionization time-of-flight mass spectrometry analysis of 36 blood group alleles among 396 Thai samples reveals region-specific variants Philaiphon Jongruamklang,1 Christoph Gassner,2 Stefan Meyer,2 Aksarakorn Kummasook,3 Marion Darlison,1 Chayanun Boonlum,4 Surin Chanta,5 Beat M. Frey,2 Martin L. Olsson,1,6* and Jill R. Storry 1,6* lood group antigen polymorphism shows great BACKGROUND: Blood group phenotype variation has variation in different world populations. The been attributed to potential resistance to pathogen reason for this is not completely understood; invasion. Variation was mapped in blood donors from however, it has been attributed to both Lampang (northern region) and Saraburi (central region), B Thailand, where malaria is endemic. The previously unknown blood group allele profiles were characterized ABBREVIATIONS: MALDI-TOF MS 5 matrix-assisted laser and the data were correlated with phenotypes. The high desorption/ionization time-of-flight mass spectrometry; PCR- incidence of the Vel-negative phenotype previously ASP 5 polymerase chain reaction with allele-specific reported in Thais was investigated. primers; SNP(s) 5 single nucleotide polymorphism(s). STUDY DESIGN AND METHODS: DNA from 396 From 1Hematology and Transfusion Medicine, Department of blood donors was analyzed by matrix-assisted laser Laboratory Medicine, Lund University, Lund, Sweden; desorption/ionization–time-of-flight mass spectrometry. 2Molecular Diagnostics & Research (MOC), Blood Transfusion Outliers were investigated by serology and DNA Service Zurich,€ Zurich-Schlieren,€ Switzerland; 3Department of sequencing. Allele discrimination assays for SMIM1 Medical Technology, School of Allied Health Sciences, rs1175550A/G and ACKR1 rs118062001C/T were University of Phayao, Phayao, Thailand; 4Transfusion Medicine, performed and correlated with antigen expression. -

Aw-Poster-Pongsak Pirom-0629
Poster #0629 HEPATITIS B VIRUS DNA LEVEL CHANGES IN HBeAg+ PREGNANT WOMEN RECEIVING TDF FOR PREVENTION OF MOTHER-TO-CHILD TRANSMISSION IRD-CMU PHPT CROIConference on Retroviruses Nicole Ngo-Giang-Huong1, Nicolas Salvadori2, Woottichai Khamduang2, Tim R. Cressey2, Linda J. Harrison3, Luc Decker1, Camlin Tierney3, Jullapong Achalapong4, and Opportunistic Infections Trudy V. Murphy5, Noele Nelson5, George K. Siberry6, Raymond T. Chung7, Stanislas Pol8, Gonzague Jourdain1, for the iTAP study group 1IRD, Chiang Mai, Thailand, 2Chiang Mai University, Chiang Mai, Thailand, 3Harvard University, Boston, MA, USA, 4Chiangrai Prachanukroh Hospital, Chiang Rai, Thailand, 5CDC, Atlanta, GA, USA, 6USAID, Arlington, VA, USA, 7Massachusetts General Hospital, Boston, MA, USA, 8Cochin Hospital, Paris, France Background HBV DNA load measurements • 12% (19 of 161) did not achieve 5.3 log10 IU/ml at delivery; References • Population: all women assigned to the TDF arm + a randomly the median (range) HBV DNA for these women was 8.3 • High hepatitis B virus (HBV) DNA levels and positive hepatitis (7.1 to 9.1) log IU/mL at baseline, 7.4 (4.7 to 8.6) at • Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on selected subset of 50 women assigned to the placebo arm 10 B e antigen (HBeAg-an indicator of rapid viral replication and 32-weeks, 7.0 (3.9 to 8.5) at 36 weeks and 7.8 (5.3 to 8.9) the management of hepatitis B: a 2015 update. Hepatol Int 2016;10:1-98. • European Association for the Study of the Liver. Electronic address eee, high level of HBV DNA) are the main markers of risk for • Timing: at baseline (28 weeks gestation), at Weeks 32 and at delivery. -

Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveilla
applyparastyle “fig//caption/p[1]” parastyle “FigCapt” View metadata, citation and similar papers at core.ac.uk brought to you by CORE Open Forum Infectious Diseases provided by Apollo MAJOR ARTICLE Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveillance System Viriya Hantrakun,1, Somkid Kongyu,2 Preeyarach Klaytong,1 Sittikorn Rongsumlee,1 Nicholas P. J. Day,1,3 Sharon J. Peacock,4 Soawapak Hinjoy,2,5 and Direk Limmathurotsakul1,3,6, 1Mahidol-Oxford Tropical Medicine Research Unit (MORU), Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, 2 Epidemiology Division, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, 3 Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, Old Road Campus, University of Oxford, Oxford, United Kingdom, 4 Department of Medicine, University of Cambridge, Cambridge, United Kingdom, 5 Office of International Cooperation, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, and 6 Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand Background. National notifiable diseases surveillance system (NNDSS) data in developing countries are usually incomplete, yet the total number of fatal cases reported is commonly used in national priority-setting. Melioidosis, an infectious disease caused by Burkholderia pseudomallei, is largely underrecognized by policy-makers due to the underreporting of fatal cases via the NNDSS. Methods. Collaborating with the Epidemiology Division (ED), Ministry of Public Health (MoPH), we conducted a retrospec- tive study to determine the incidence and mortality of melioidosis cases already identified by clinical microbiology laboratories nationwide. A case of melioidosis was defined as a patient with any clinical specimen culture positive for B. -
Physical Activity and Sedentary Behaviour Research in Thailand: a Systematic Scoping Review Nucharapon Liangruenrom1,2, Kanyapat Suttikasem2, Melinda Craike1, Jason A
Liangruenrom et al. BMC Public Health (2018) 18:733 https://doi.org/10.1186/s12889-018-5643-y RESEARCH ARTICLE Open Access Physical activity and sedentary behaviour research in Thailand: a systematic scoping review Nucharapon Liangruenrom1,2, Kanyapat Suttikasem2, Melinda Craike1, Jason A. Bennie3, Stuart J. H. Biddle3 and Zeljko Pedisic1* Abstract Background: The number of deaths per year attributed to non-communicable diseases is increasing in low- and middle-income countries, including Thailand. To facilitate the development of evidence-based public health programs and policies in Thailand, research on physical activity (PA) and sedentary behaviour (SB) is needed. The aims of this scoping review were to: (i) map all available evidence on PA and SB in Thailand; (ii) identify research gaps; and (iii) suggest directions for future research. Methods: A systematic literature search was conducted through 10 bibliographic databases. Additional articles were identified through secondary searches of reference lists, websites of relevant Thai health organisations, Google, and Google Scholar. Studies written in Thai or English were screened independently by two authors and included if they presented quantitative or qualitative data relevant to public health research on PA and/or SB. Results: Out of 25,007 screened articles, a total of 564 studies were included in the review. Most studies included PA only (80%), 6.7% included SB only, and 13.3% included both PA and SB. The most common research focus was correlates (58.9%), followed by outcomes of PA/SB (22.2%), prevalence of PA/SB (12.4%), and instrument validation (3.2%). Most PA/SB research was cross-sectional (69.3%), while interventions (19.7%) and longitudinal studies (2.8%) were less represented. -

Estimation of Non-Point Source BOD Loading in Urban Area
Research Article Science, Engineering and Health Studies 2018, 12(1), 33-45 An assessment of health-related quality of life using generic and HIV-specific instruments among patients receiving antiretroviral therapy at a general hospital in central Thailand Tipaporn Pongmesa1*, Pranee Luckanajantachote2, Kulvaree Kositchaiwat1, 1 1 1 Jantapa Waewpunyasin , Panida Trongtrakarn and Arunroj Oransuwanchai 1Department of Pharmacy, Faculty of Pharmacy, Silpakorn University, Nakhon Pathom 73000, Thailand 2Department of Pharmacy, Samutsakhon Hospital, Samutsakhon 74000, Thailand *Corresponding author: [email protected] Received: May 5, 2017; Accepted: December 7, 2017 ABSTRACT This cross-sectional study aimed to assess the health-related quality of life (HRQoL) among 210 HIV- positive patients receiving antiretroviral therapy (ART) at a general hospital in Central Thailand, and to analyze correlations between scores from HIV-specific and generic HRQoL instruments. A small majority of the participants were female (56.2%) with a mean (SD) age of 43.3 (7.9) years. An assessment using the World Health Organization Quality of Life-HIV Brief Version (WHOQOL-HIV BREF) demonstrated that most participants reported moderate levels for overall HRQoL (71.9%) and general health (40.5%). The mean scores of the six domains ranged from 12.64 to 16.20 out of a total score of 20, with the lowest and highest scores being reported for ‘social relationships’ and ‘spiritual/personal beliefs/religion’. For the 5-level EuroQol-5 dimension (EQ-5D-5L), most participants reported ‘no problems’ in any of the five health dimensions, with mean (SD) EQ-5D-5L utility and EQ VAS scores of 0.93 (0.08) and 81.43 (15.75) respectively. -

JIRAKIATTIKUL Sopin 2 Curriculum Vitae
Sopin JIRAKIATTIKUL (Ph.D. Economics) Faculty of Economics e-mail: [email protected] Prince of Songkla University, Had Yai Campus Had Yai, Songkhla 90112 THAILAND. FACULTY APPOINTMENTS Assistant Professor Associate Dean for Academic Affairs and International Affairs January, 2018 to present. Associate Dean for Academic Affairs (Acting) November, 2012 to September 2013 Associate Dean for Academic Affairs and Organization Development June 15, 2011 to September 2012. Lecturer February, 1995 to present Faculty of Economics, Prince of Songkla University (PSU), Hat yai Campus, Songkhla, THAILAND. OTHER APPOINTMENTS Committee member and resource person of the Southern Woman Group, 1995 to 1998 Committee member of the 8th National Social and Economic Development Plan, Office of Research and Development, PSU, 1995 to 1996 Head of fundamental subjects, Department of Business Administration, Faculty of Management Sciences, PSU, 2002 to 2003 Committee member and resource person of the development ethics group, Department of Business Administration, Faculty of Management Sciences, PSU, 2002 to 2003 Executive committee member for the « Association des Doctorants et Docteurs en Economie et en Gestion de Montpellier » (Economics and Business Association of Ph.D. and Ph.D. Students from Montpellier), Université Montpellier I, Faculté de Sciences Economiques, 2008 to 2009 Member of the sub-committee for university welfare, Prince of Songkla University. (since January18, 2011) Committee member for the Academic Affairs, Prince of Songkla University. (since 2012-2013) Committee member for the Academic Affairs, Prince of Songkla University. (since January, 2018 to present) Committee member of the Center for Social and Behavioral Sciences Institutional Review Board, Prince of Songkla University. (since January, 2019 to present) JIRAKIATTIKUL Sopin 2 Curriculum vitae EDUCATION University of Montpellier I Ph.D (1st Hons, Political and Development Economics), 2010. -

8Th Thailand Orthopaedic Trauma Annual Congress (TOTAC) 'How
8th Thailand Orthopaedic Trauma Annual Congress (TOTAC) February, 20-22, 2019 @Somdej Phra BorommaRatchathewi Na Si ‘How can we operate as an expert? Pearls and pitfalls’ Racha Hospital, Chonburi TOTAC 2019 “Trauma Night, Dinner Symposium” Feb 20,2019 Room Speaker 18.00-19.00 Fractures of the upper extremity (Thai) Panelist : Chanakarn Phornphutkul Nathapon Chantaraseno Vajarin Phiphobmongkol Surasak Jitprapaikulsarn 18.00-18.15 Fracture-Dislocation of Elbow Sanyakupta Boonperm 18.15-18.30 Neglected fracture of proximal humerus Vantawat Umprai 18.30-18.45 Complex scapular fracture Wichai Termsombatborworn 18.45-19.00 Failed plate of humeral shaft Chonlathan Iamsumang 19.00-20.00 Fractures of the lower extremity (Thai) Panelist : Apipop Kritsaneephaiboon Noratep Kulachote Vajara Phiphobmongkol Pongpol Petchkam 19.00-19.15 Complex fracture of femoral shaft Preecha Bunchongcharoenlert 19.15-19.30 Complex Tibial Plateau Fracture Sasipong Rohitotakarn 19.30-19.45 Posterior Hip Dislocation with Femoral Head Fracture Phoonyathorn Phatthanathitikarn 19.45-20.00 Complex Tibial plafond Fracture Pissanu Reingrittha Page 1 of Feb 21,2019 Room A Speaker Feb 21,2019 Room B Speaker Feb 21,2019 Room C 8.30-10.00 Module 1 : Complex tibial plateau fracture : The art of reconstruction (Thai) Moderator Likit Rugpolmuang Komkrich Wattanapaiboon 8.30-8.40 Initial management and staged approach Puripun Jirangkul 8.40-8.50 Three-column concept and preoperative planning Sorawut Thamyongkit 8.50-9.00 Single or dual implants : how to make a decision? Eakachit Sikarinkul