Local and Regional Anesthesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nerve Blocks for Surgery on the Shoulder, Arm Or Hand
Nerve blocks for surgery on the shoulder, arm or hand Information for patients and families First Edition 2015 www.rcoa.ac.uk/patientinfo Nerve blocks for surgery on the shoulder, arm or hand This leaflet is for anyone who is thinking about having a nerve block for an operation on the shoulder, arm or hand. It will be of particular interest to people who would prefer not to have a general anaesthetic. The leaflet has been written with the help of patients who have had a nerve block for their operation. Throughout this leaflet we have used the above symbol to highlight key facts. Brachial plexus block? The brachial plexus is the group of nerves that lies between your neck and your armpit. It contains all the nerves that supply movement and feeling to your arm – from your shoulder to your fingertips. A brachial plexus block is an injection of local anaesthetic around the brachial plexus. It ‘blocks’ information travelling along these nerves. It is a type of nerve block. Your arm becomes numb and immobile. You can then have your operation without feeling anything. The block can also provide excellent pain relief for between three and 24 hours, depending on what kind of local anaesthetic is used. A brachial plexus block rarely affects the rest of the body so it is particularly advantageous for patients who have medical conditions which put them at a higher risk for a general anaesthetic. A brachial plexus block may be combined with a general anaesthetic or with sedation. This means you have the advantage of the pain relief provided by a brachial plexus block, but you are also unconscious or sedated during the operation. -

Femoral Nerve Block Versus Spinal Anesthesia for Lower Limb
Alexandria Journal of Anaesthesia and Intensive Care 44 Femoral Nerve Block versus Spinal Anesthesia for Lower Limb Peripheral Vascular Surgery By Ahmed Mansour, MD Assistant Professor of Anesthesia, Faculty of Medicine, Alexandria University. Abstract Perioperative cardiac complications occur in 4% to 6% of patients undergoing infrainguinal revascularization under general, spinal, or epidural anesthesia. The risk may be even greater in patients whose cardiac disease cannot be fully evaluated or treated before urgent limb salvage operations. Prompted by these considerations, we investigated the feasibility and results of using femoral nerve block with infiltration of the genito4femoral nerve branches in these high-risk patients. Methods: Forty peripheral vascular reconstruction of lower limbs were performed under either spinal anesthesia (20 patients) or femoral nerve block with infiltration of genito-femoral nerve branches supplemented with local infiltration at the site of dissection as needed (20 patients). All patients had arterial lines. Arterial blood pressure and electrocardiographic monitoring was continued during surgery, in PACU and in the intensive care units. Results: Operations included femoral-femoral, femoral-popliteal bypass grafting and thrombectomy. The intra-operative events showed that the mean time needed to perform the block and dose of analgesics and sedatives needed during surgery was greater in group I (FNB,) compared to group II [P=0.01*, P0.029* , P0.039*], however, the time needed to start surgery was shorter in group I than in group II [P=0. 039]. There were no block failures in either group, but local infiltration in the area of the dissection with 2 ml (range 1-5 ml) of 1% lidocaine was required in 4 (20%) patients in FNB group vs none in the spinal group. -

Nerve Injury After Peripheral Nerve Block: Allbest Rights Practices Reserved
PRINTER-FRIENDLY VERSION AVAILABLE AT ANESTHESIOLOGYNEWS.COM Nerve Injury After Peripheral Nerve Block: AllBest rights Practices reserved. Reproduction and Medical-Legal in whole or in part without Protection permission isStrategies prohibited. Copyright © 2015 McMahon Publishing Group unless otherwise noted. DAVID HARDMAN, MD, MBA Professor of Anesthesiology Vice Chair for Professional Affairs Department of Anesthesiology University of North Carolina at Chapel Hill Chapel Hill, North Carolina Dr. Hardman reports no relevant financial conflicts of interest. he risk for permanent or severe nerve injury after peripheral nerve blocks (PNBs) is Textremely low, irrespective of its etiology (ie, related to anesthesia, surgery or the patient). The risk inherent in a procedure should always be explicitly discussed with the patient (sidebar, page 4). In fact, it may be better to define this phenomenon ultrasound-guided axillary blocks were used, demon- as postoperative neurologic symptoms (PONS) or peri- strated a very low nerve injury rate of 0.0037% at hos- operative nerve injuries (PNI) in order to help stan- pital discharge.1-7 dardize terminology. Permanent injury rates, as defined A 2009 prospective case series involving more than by a neurologic abnormality present at or beyond 12 7,000 PNBs, conducted in Australia and New Zealand, months after the procedure, have consistently ranged demonstrated that when a postoperative neurologic from 0.029% to 0.2%, although the results of a recent symptom was diagnosed, it was 9 times more likely to multicenter Web-based survey in France, in which be due to a non–anesthesia-related cause than a nerve ANESTHESIOLOGY NEWS • JULY 2015 1 block–related cause.6 On the other hand, it is well doc- PNI rate of 1.7% in patients who received a single-injec- umented in the orthopedic and anesthesia literature tion interscalene block (ISB). -
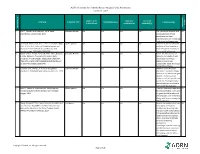
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table
AORN Guideline for Patients Receiving Local-Only Anesthesia Evidence Table SAMPLE SIZE/ CONTROL/ OUTCOME CITATION EVIDENCE TYPE INTERVENTION(S) CONCLUSION(S) POPULATION COMPARISON MEASURE(S) SCORE CONSENSUS REFERENCE # REFERENCE 1 Lirk P., Picardi S. and Hollmann, M. W. Local Literature Review n/a n/a n/a n/a The mechanism of action and VA anaesthetics: 10 essentials. 2014 access pathways of local anesthetics and their pharmokinetics are increasingly understood and appreciated. 2 Calatayud, Jesús, M.D.,D.D.S., Ph.D., González, Õngel, Expert Opinion n/a n/a n/a n/a A review of the discovery and VA M.D., D.D.S., Ph.D. History of the development and evolution of local anesthesia evolution of local anesthesia since the coca leaf. from the Spanish discovery of Anesthesiology. 2003;98(6):1503-1508. the coca leaf in America. 3 Gordh T, M.D., Gordh, Torsten E.,M.D., Ph.D., Lindqvist Literature Review n/a n/a n/a n/a Before the introduction of VA K, M.Sc. Lidocaine: The origin of a modern local lidocaine, the choice of local anesthetic. Anesthesiology. 2010;113(6):1433-1437. anesthetics was limited. https://doi.org/10.1097/ALN.0b013e3181fcef48. doi: Lidocaine's onset was 10.1097/ALN.0b013e3181fcef48. substantially faster and longer lasting than procaine. 4 Volcheck G.W., Mertes, P. M. Local and general Literature Review n/a n/a n/a n/a Whether to test the local VA anesthetics immediate hypersensitivity reactions. 2014 anesthetic causing the allergic reaction or an alternative agent depends on the expected future need of the specific local anesthetic. -

The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures
Volume 2- Issue 1 : 2018 DOI: 10.26717/BJSTR.2018.02.000695 Eduardo de Oliveira Duque-Estrada. Biomed J Sci & Tech Res ISSN: 2574-1241 Mini Review Open Access The Use of Buffering Solutions in the Pediatrics Local Anesthesia to Reduce the Pain of Minor Procedures Eduardo de Oliveira Duque-Estrada MD* Received: January 17, 2018; Published: January 25, 2018 *Corresponding author: Eduardo de Oliveira Duque-Estrada, Ex-Professor of Pediatrics and Pediatric Surgery, Teresópolis Schoolof Medicine, Rio de Janeiro, Rua Jose da Silva Ribeiro 119 apt 11 São Paulo, SP Brazil CEP: 05726-130, Email: Abstract The local anesthetics are widely u sed in minor pediatric surgical procedures. The major problem with their use is the resulted pain experienced by the patients at the time of injection. To discuss those situations in the light of the medical literature we present this mini-review. Key words: Local Injection; Pain; Buffer; pH; Lidocaine; Pediatric Surgery Procedure Introduction Table 1: Techniques for injection pain control*. a eutectic mixture of lidocaine and prilocaine (EMLA) cream [17] S.No Techniques for injection pain control before infiltration, and local external cooling (cryoanalgesia) have 1. Warming the anesthetic solution [18,19] (Table 1). also been used to reduce the pain of infiltration of local anesthetic 2. Buffering the anesthetic Buffering the Anesthetic 3. Injection technique 4. Distraction Local anesthesia is extremely useful either as the sole method the best results on the minor surgery in general [3,6]. Blocking 5. Combination anesthetic technique the pain pathway with local anesthetic solution will also reduce 6. Cooling of skin the family stress response to the surgical procedure. -

Nerve Blocks for Surgery on the Shoulder, Arm Or Hand
The Association of Regional The Royal College of Anaesthetists of Great Anaesthesia – Anaesthetists Britain and Ireland United Kingdom Nerve blocks for surgery on the shoulder, arm or hand Information for patients and families www.rcoa.ac.uk/patientinfo First edition 2015 This leaflet is for anyone who is thinking about having a nerve block for an operation on the shoulder, arm or hand. It will be of particular interest to people who would prefer not to have a general anaesthetic. The leaflet has been written with the help of patients who have had a nerve block for their operation. You can find more information leaflets on the website www.rcoa.ac.uk/patientinfo. The leaflets may also be available from the anaesthetic department or pre-assessment clinic in your hospital. The website includes the following: ■ Anaesthesia explained (a more detailed booklet). ■ You and your anaesthetic (a shorter summary). ■ Your spinal anaesthetic. ■ Anaesthetic choices for hip or knee replacement. ■ Epidural pain relief after surgery. ■ Local anaesthesia for your eye operation. ■ Your child’s general anaesthetic. ■ Your anaesthetic for major surgery with planned high dependency care afterwards. ■ Your anaesthetic for a broken hip. Risks associated with your anaesthetic This is a collection of 14 articles about specific risks associated with having an anaesthetic or an anaesthetic procedure. It supplements the patient information leaflets listed above and is available on the website: www.rcoa.ac.uk/patients-and-relatives/risks. Throughout this leaflet and others in the series, we have used this symbol to highlight key facts. 2 NERVE BLOCKS FOR SURGERY ON THE SHOULDER, ARM OR HAND Brachial plexus block? The brachial plexus is the group of nerves that lies between your neck and your armpit. -

OHSU Regional Anesthesia Peripheral Nerve Block Overview
OHSU Regional Anesthesia Peripheral Nerve Block Overview Recommended information: To view 3 short informative videos about nerve blocks, how they are placed, and postoperative care, please search for OHSU Home Pump in your internet browser, or visit: http://www.ohsu.edu/xd/health/services/anesthesiology/for-patients/home-pump.cfm What does an anesthesiologist do? An anesthesiologist is a medical doctor who keeps you safe and comfortable during surgery. An anesthesiologist will meet with you prior to surgery to make sure you are prepared and medically fit to undergo surgery and anesthesia. Your anesthesiologist will discuss a plan for what kind of anesthesia you will receive. During the surgery, your anesthesiologist will monitor and regulate your critical life functions, such as your heart rate, blood pressure, and level of oxygen in the blood. And, they take care of you after surgery to make sure you’re as comfortable as possible as you recover. What are the types of anesthesia? 1. General anesthesia. This type of anesthesia is given as an anesthetic gas you breathe in, or as an intravenous medication given through an intravenous catheter (IV). It makes you lose consciousness. While the anesthesia is working, many of your body’s functions will slow down or need help to work effectively. A tube may be placed in your throat to help you breathe. Once your surgery is complete, your anesthesiologist will reverse the medication and be with you as you regain consciousness. It is used for major operations. 2. Monitored anesthesia care or IV sedation. IV sedation causes you to feel relaxed and can result in various levels of consciousness. -

Veterinary Anesthetic and Analgesic Formulary 3Rd Edition, Version G
Veterinary Anesthetic and Analgesic Formulary 3rd Edition, Version G I. Introduction and Use of the UC‐Denver Veterinary Formulary II. Anesthetic and Analgesic Considerations III. Species Specific Veterinary Formulary 1. Mouse 2. Rat 3. Neonatal Rodent 4. Guinea Pig 5. Chinchilla 6. Gerbil 7. Rabbit 8. Dog 9. Pig 10. Sheep 11. Non‐Pharmaceutical Grade Anesthetics IV. References I. Introduction and Use of the UC‐Denver Formulary Basic Definitions: Anesthesia: central nervous system depression that provides amnesia, unconsciousness and immobility in response to a painful stimulation. Drugs that produce anesthesia may or may not provide analgesia (1, 2). Analgesia: The absence of pain in response to stimulation that would normally be painful. An analgesic drug can provide analgesia by acting at the level of the central nervous system or at the site of inflammation to diminish or block pain signals (1, 2). Sedation: A state of mental calmness, decreased response to environmental stimuli, and muscle relaxation. This state is characterized by suppression of spontaneous movement with maintenance of spinal reflexes (1). Animal anesthesia and analgesia are crucial components of an animal use protocol. This document is provided to aid in the design of an anesthetic and analgesic plan to prevent animal pain whenever possible. However, this document should not be perceived to replace consultation with the university’s veterinary staff. As required by law, the veterinary staff should be consulted to assist in the planning of procedures where anesthetics and analgesics will be used to avoid or minimize discomfort, distress and pain in animals (3, 4). Prior to administration, all use of anesthetics and analgesic are to be approved by the Institutional Animal Care and Use Committee (IACUC). -

Universal Documentation Sheet for Peripheral Nerve Blocks
THE JOURNAL OF NEW YORK SCHOOL May 2009 V o l u m e OF REGIONAL ANESTHESIA 12 UNIVERSAL DOCUMENTATION SHEET FOR PERIPHERAL NERVE BLOCKS BY KISHOR GANDHI MD MPH, VIJAY PATEL MD, THOMAS MALIAKAL MD, DAQUAN XU MD, KAMIL FLISINSKI BS Author Affiliation: Department of Anesthesiology, St. Luke’s and Roosevelt Hospitals, New York, NY Reimbursements for peripheral nerve blocks (PNB’s) can be complicated by charge bundles that utilize specific procedure codes (CPT) and unit values.1-2 Individual providers use specific information contained in the patient’s medical records for reimbursement. Careful documentation for PNB’s should include: Surgical diagnosis, name of surgeon requesting regional service, and details of procedure (specific nerve block, reason of nerve block, type of needle and catheter used, ultrasound guided versus neurostimulation technique, and the local anesthetic used). In addition, attaching a printed photograph of the nerve block procedure (containing patient identification and localization of the nerve) will also aid in reimbursements from insurance providers. We at NYSORA have found huge discrepancies in billed amount for PNB’s compared to what is reimbursed by different providers.3 We have developed a universal billing sheet for institution to aid in reimbursements. The Journal of NYSORA 2009; 12: 23-24 REFERENCES 1. Mariano, ER. Billing for Peripheral Nerve Blocks (United States). Available at: http://edmariano.com/billing-for- regional-anesthesia 2. Gerancher JC, Viscusi ER, Liguori Ga, McCartney CI, Williams BA, Ilfeld BM, Grant SA, Hebl JR, Hadzic A. Development of a standardized peripheral nerve block procedure note form. Regional Anesthesia and Pain Medicine. -
Local Anesthesia for Carpal Tunnel Surgery
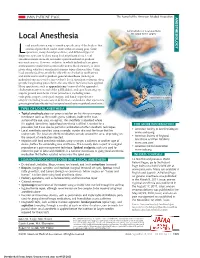
JAMA PATIENT PAGE The Journal of the American Medical Association ANESTHESIOLOGY Administration of local anesthetic Local Anesthesia for carpal tunnel surgery ocal anesthesia is a way to numb a specific area of the body so that a medical procedure can be done without causing pain. Some Loperations, many dental procedures, and different types of diagnostic tests can be done using local anesthesia alone. Local anesthesia medications do not make a person sedated or produce unconsciousness. However, sedation, in which individuals are given medications to make them comfortable and to block memory, is often given along with local anesthesia for many types of procedures. Using local anesthesia alone avoids the side effects of sedation medications and medications used to produce general anesthesia (making an individual unconscious for a procedure). Local anesthetic solutions often provide long-lasting pain relief to the area where they have been applied. Many operations, such as appendectomy (removal of the appendix), cholecystectomy (removal of the gallbladder), and open heart surgery, require general anesthesia. Other procedures, including some orthopedic surgery, urological surgery, and female reproductive Carpal tunnel surgery surgery (including most cesarean deliveries), can be done after a person is given regional anesthesia (such as spinal anesthesia or epidural anesthesia). TYPES OF LOCAL ANESTHESIA • Topical anesthesia places or sprays a solution on the skin or a mucous membrane (such as the mouth, gums, eardrum, inside of the nose, surface of the eye, anus, or vagina). The anesthetic is absorbed where it is applied. Sometimes topical local anesthesia is all that is needed for a FOR MORE INFORMATION procedure, but it can also be part of a combination of other anesthetic techniques. -

Veterinary Anesthesia and Pain Management Secrets / Edited by Stephen A
Publisher: HANLEY & BELFUS, INC. Medical Publishers 210 South 13th Street Philadelphia, PA 19107 (215) 546-7293; 800-962-1892 FAX (215) 790-9330 Web site: http://www.hanleyandbelfus.com Note to the reader Although the information in this book has been carefully reviewed for cor rectness of dosage and indications, neither the authors nor the editor nor the publisher can accept any legal responsibility for any errors or omissions that may be made. Neither the publisher nor the editor makes any warranty, expressed or implied, with respect to the material contained herein. Before prescribing any drug. the reader must review the manu facturer's correct product information (package inserts) for accepted indications, absolute dosage recommendations. and other information pertinent to the safe and effective use of the product described. This is especially important when drugs are given in combination or as an adjunct to other forms of therapy Library of Congress Cataloging-in-Publication Data Veterinary anesthesia and pain management secrets / edited by Stephen A. Greene. p. em. - (The Secrets Series®) Includes bibliographical references (p.). ISBN 1-56053-442-7 (alk paper) I. Veterinary anesthesia-Examinations, questions. etc. 2. Pain in animals Treatment-Examinations, questions, etc. I. Greene, Stephen A., 1956-11. Series. SF914.V48 2002 636 089' 796'076--dc2 I 2001039966 VETERINARY ANESTHESIA AND PAIN MANAGEMENT SECRETS ISBN 1-56053-442-7 © 2002 by Hanley & Belfus, Inc. All rights reserved. No part of this book may be repro duced, reused, republished. or transmitted in any form, or stored in a database or retrieval system, without written permission of the publisher Last digit is the print number: 9 8 7 6 5 4 3 2 CONTRIBUTORS G. -

Fascia Iliaca Block in the Emergency Department
The Royal College of Emergency Medicine Best Practice Guideline Fascia Iliaca Block in the Emergency Department 1 Revised: July 2020 Contents Summary of recommendations ...................................................................................................... 3 Scope ..................................................................................................................................................... 4 Reason for development ................................................................................................................. 4 Introduction .......................................................................................................................................... 4 Considerations ..................................................................................................................................... 4 Safety of FIB ...................................................................................................................................... 4 Improving safety of FIB .................................................................................................................. 5 Controversies regarding FIB ......................................................................................................... 5 Efficacy of FIB ................................................................................................................................... 6 Procedures within ED ....................................................................................................................