Readingsample
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Pubid-1446077038.Pdf
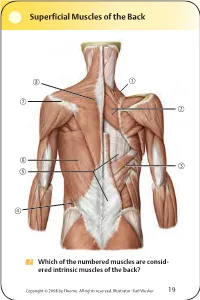
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

Cervical Arterial Collateral Network References Reply: Reference Age
Cervical Arterial Collateral Network Age and Gender Effects on Normal Regional Cerebral Purkayastha et al1 reported 3 cases of proatlantal intersegmental Blood Flow arteries of external carotid artery origin associated with Galen’s vein We read with great interest the article of Takahashi et al.1 The article malformation; however, because of their configuration, I believe that points out the use of 3D stereotactic surface projections (3D-SSP) to the 3 cases do not demonstrate this rare arterial variation, but rather study the age-effect on regional cerebral blood flow (rCBF). The show collateral blood flow from the occipital artery (OA) to the ver- greatest rCBF reduction observed was in the bilateral anterior cingu- tebral artery (VA). In patients with a vein of Galen malformation, the late. Although we generally agree with the conclusions, we would like intra-arterial blood pressure in the VA is lower than that in the OA to emphasize some methodologic issues that may have had an impact because of blood steal phenomenon at the malformation. It is well on the obtained results. known that there is a cervical arterial collateral network between OA, In the study, 31 healthy volunteers between 50 and 79 years were classified in 3 different age classes (50–59, 60–69, and 70–79 years). VA, and the deep cervical artery arising from the subclavian artery.2 If Statistical analysis was performed 2 by 2 by using unpaired Student t test. one of these arteries is occluded, the remaining arteries and their Rather than considering age as a discrete variable, the analysis would have branches are dilated and supply the distal segment of the occluded been strengthened by performing a multivariate analysis based on the artery. -

The Variations of the Subclavian Artery and Its Branches Ahmet H
Okajimas Folia Anat. Jpn., 76(5): 255-262, December, 1999 The Variations of the Subclavian Artery and Its Branches By Ahmet H. YUCEL, Emine KIZILKANAT and CengizO. OZDEMIR Department of Anatomy, Faculty of Medicine, Cukurova University, 01330 Balcali, Adana Turkey -Received for Publication, June 19,1999- Key Words: Subclavian artery, Vertebral artery, Arterial variation Summary: This study reports important variations in branches of the subclavian artery in a singular cadaver. The origin of the left vertebral artery was from the aortic arch. On the right side, no thyrocervical trunk was found. The two branches which normally originate from the thyrocervical trunk had a different origin. The transverse cervical artery arose directly from the subclavian artery and suprascapular artery originated from the internal thoracic artery. This variation provides a short route for posterior scapular anastomoses. An awareness of this rare variation is important because this area is used for diagnostic and surgical procedures. The subclavian artery, the main artery of the The variations of the subclavian artery and its upper extremity, also gives off the branches which branches have a great importance both in blood supply the neck region. The right subclavian arises vessels surgery and in angiographic investigations. from the brachiocephalic trunk, the left from the aortic arch. Because of this, the first part of the right and left subclavian arteries differs both in the Subjects origin and length. The branches of the subclavian artery are vertebral artery, internal thoracic artery, This work is based on a dissection carried out in thyrocervical trunk, costocervical trunk and dorsal the Department of Anatomy in the Faculty of scapular artery. -

Embolization for Hemoptysis—Angiographic Anatomy of Bronchial and Systemic Arteries
THIEME 184 Pictorial Essay Embolization for Hemoptysis—Angiographic Anatomy of Bronchial and Systemic Arteries Vikash Srinivasaiah Setty Chennur1 Kumar Kempegowda Shashi1 Stephen Edward Ryan1 1 1 Adnan Hadziomerovic Ashish Gupta 1Division of Angio-Interventional Radiology, Department of Medical Address for correspondence Ashish Gupta, MD, Division of Imaging, University of Ottawa, The Ottawa Hospital, Ottawa, Angio-Interventional Radiology, Department of Medical Imaging, Ontario, Canada University of Ottawa, The Ottawa Hospital, 501 Smyth Road, Ottawa, ON K1H 8L6, Canada (e-mail: [email protected]). J Clin Interv Radiol ISVIR 2018;2:184–190 Abstract Massive hemoptysis is a potentially fatal respiratory emergency. The majority of these patients are referred to interventional radiology for bronchial artery embolization (BAE). Immediate clinical success in stopping hemoptysis ranges from 70 to 99%. However, recurrent hemoptysis after BAE is seen in 10 to 55% patients. One of the main reasons for recurrence is incomplete embolization due to unidentified aberrant Keywords bronchial and/or non-bronchial systemic arterial supply. This pictorial essay aims to ► bronchial describe the normal and variant bronchial arterial anatomy and non-bronchial systemic ► embolization arterial feeders to the lungs on conventional angiography; the knowledge of which is ► hemoptysis critical for interventional radiologists involved in the care of patients with hemoptysis. Introduction Angiographic Anatomy of Bronchial Arteries Massive hemoptysis is a respiratory -

Intercostal Arteries a Single Posterior & Two Anterior Intercostal Arteries
Intercostal Arteries •Each intercostal space contains: . A single posterior & .Two anterior intercostal arteries •Each artery gives off branches to the muscles, skin, parietal pleura Posterior Intercostal Arteries In the upper two spaces, arise from the superior intercostal artery (a branch of costocervical trunk of the subclavian artery) In the lower nine spaces, arise from the branches of thoracic aorta The course and branching of the intercostal arteries follow the intercostal Posterior intercostal artery Course of intercostal vessels in the posterior thoracic wall Anterior Intercostal Arteries In the upper six spaces, arise from the internal thoracic artery In the lower three spaces arise from the musculophrenic artery (one of the terminal branch of internal thoracic) Form anastomosis with the posterior intercostal arteries Intercostal Veins Accompany intercostal arteries and nerves Each space has posterior & anterior intercostal veins Eleven posterior intercostal and one subcostal vein Lie deepest in the costal grooves Contain valves which direct the blood posteriorly Posterior Intercostal Veins On right side: • The first space drains into the right brachiocephalic vein • Rest of the intercostal spaces drain into the azygos vein On left side: • The upper three spaces drain into the left brachiocephalic vein. • Rest of the intercostal spaces drain into the hemiazygos and accessory hemiazygos veins, which drain into the azygos vein Anterior Intercostal Veins • The lower five spaces drain into the musculophrenic vein (one of the tributary of internal thoracic vein) • The upper six spaces drain into the internal thoracic vein • The internal thoracic vein drains into the subclavian vein. Lymphatics • Anteriorly drain into anterior intercostal nodes that lie along the internal thoracic artery • Posterioly drain into posterior intercostal nodes that lie in the posterior mediastinum . -

A Functional Perspective on the Embryology and Anatomy of the Cerebral Blood Supply
Journal of Stroke 2015;17(2):144-158 http://dx.doi.org/10.5853/jos.2015.17.2.144 Review A Functional Perspective on the Embryology and Anatomy of the Cerebral Blood Supply Khaled Menshawi,* Jay P Mohr, Jose Gutierrez Department of Neurology, Columbia University Medical Center, New York, NY, USA The anatomy of the arterial system supplying blood to the brain can influence the develop- Correspondence: Jose Gutierrez ment of arterial disease such as aneurysms, dolichoectasia and atherosclerosis. As the arteries Department of Neurology, Columbia University Medical Center, 710 W 168th supplying blood to the brain develop during embryogenesis, variation in their anatomy may Street, New York, NY, 10032, USA occur and this variation may influence the development of arterial disease. Angiogenesis, Tel: +1-212-305-1710 Fax: +1-212-305-3741 which occurs mainly by sprouting of parent arteries, is the first stage at which variations can E-mail: [email protected] occur. At day 24 of embryological life, the internal carotid artery is the first artery to form and it provides all the blood required by the primitive brain. As the occipital region, brain Received: December 18, 2014 Revised: February 26, 2015 stem and cerebellum enlarge; the internal carotid supply becomes insufficient, triggering the Accepted: February 27, 2015 development of the posterior circulation. At this stage, the posterior circulation consists of a primitive mesh of arterial networks that originate from projection of penetrators from the *This work was done while Mr. Menshawi was visiting research fellow at Columbia distal carotid artery and more proximally from carotid-vertebrobasilar anastomoses. -

On the Anatomy of Intercostal Spaces in Man and Certain Other Mammals1 by Prof
ON THE ANATOMY OF INTERCOSTAL SPACES IN MAN AND CERTAIN OTHER MAMMALS1 BY PROF. M. A. H. SIDDIQI, M.B., D.L.O., M.S., F.R.C.S. (ENG.) AND DR A. N. MULLICK, M.B., B.S. Anatomy Department, King George's Medical College, Lucknow (India) TIHE standard description of the anatomy of the intercostal space has been discussed by Stibbe in a paper recently published in this Journal(2,3). Prof. Walmsley in 1916(1) showed that the intercostal nerves do not lie in the plane between the internal and external intercostal muscles but deep to the internal intercostal, and that they are separated from the pleura by a deeper musculo-fascial plane consisting of subcostal, intercostal and transversus thoracis muscles from behind forwards. According to Davies, Gladstone and Stibbe (3) there are four musculo-fascial planes in each space and in each space the main nerve lies with a collateral nerve deep to the internal intercostal. As the above paper effected a change in the teaching of the anatomy of intercostal space, we carried out the following investigations on human as well as on certain other Mammalian intercostal spaces. DISSECTION OF HUMAN INTERCOSTAL SPACES Sixty thoraces of different ages were dissected. From some of them the intercostal spaces were cut out en bloc to facilitate dissection; in others the thoracic wall was dissected as a whole. In the case of the foetuses microscopic sections were made to locate the muscular planes and the nerves. The results of our dissection were as follows: I. Intercostal muscles (fig. -

Comparing the Organs and Vasculature of the Head and Neck
in vivo 31 : 861-871 (2017) doi:10.21873/invivo.11140 Comparing the Organs and Vasculature of the Head and Neck in Five Murine Species MIN JAE KIM 1* , YOO YEON KIM 2* , JANET REN CHAO 3, HAE SANG PARK 1,4 , JIWON CHANG 1,4 , DAWOON OH 5, JAE JUN LEE 4,6 , TAE CHUN KANG 7, JUN-GYO SUH 2 and JUN HO LEE 1,4 1Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Hallym University, Chuncheon, Republic of Korea; 2Department of Medical Genetics, College of Medicine, Hallym University, Chuncheon, Republic of Korea; 3School of Medicine, George Washington University, Washington, DC, U.S.A.; 4Institute of New Frontier Research, Hallym University College of Medicine, Chuncheon, Republic of Korea; 5Department of Anesthesiology and Pain Medicine, Dongtan Sacred Heart Hospital, Hallym University, Dongtan, Republic of Korea; 6Department of Anesthesiology and Pain Medicine, College of Medicine, Hallym University, Chuncheon, Republic of Korea; 7Department of Anatomy and Neurobiology, College of Medicine, Hallym University, Chuncheon, Republic of Korea Abstract. Background/Aim: The purpose of the present Unique morphological characteristics were demonstrated by study was to delineate the cervical and facial vascular and comparing the five species, including symmetry of the associated anatomy in five murine species, and compare common carotid origin bilaterally in the Mongolian Gerbil, them for optimal use in research studies focused on a large submandibular gland in the hamster and an enlarged understanding the pathology and treatment of diseases in buccal branch in the Guinea Pig. In reviewing the humans. Materials and Methods: The specific adult male anatomical details, this staining technique proves superior animals examined were mice (C57BL/6J), rats (F344), for direct surgical visualization and identification. -

Ascending and Descending Thoracic Vertebral Arteries
CLINICAL REPORT EXTRACRANIAL VASCULAR Ascending and Descending Thoracic Vertebral Arteries X P. Gailloud, X L. Gregg, X M.S. Pearl, and X D. San Millan ABSTRACT SUMMARY: Thoracic vertebral arteries are anastomotic chains similar to cervical vertebral arteries but found at the thoracic level. Descending thoracic vertebral arteries originate from the pretransverse segment of the cervical vertebral artery and curve caudally to pass into the last transverse foramen or the first costotransverse space. Ascending thoracic vertebral arteries originate from the aorta, pass through at least 1 costotransverse space, and continue cranially as the cervical vertebral artery. This report describes the angiographic anatomy and clinical significance of 9 cases of descending and 2 cases of ascending thoracic vertebral arteries. Being located within the upper costotransverse spaces, ascending and descending thoracic vertebral arteries can have important implications during spine inter- ventional or surgical procedures. Because they frequently provide radiculomedullary or bronchial branches, they can also be involved in spinal cord ischemia, supply vascular malformations, or be an elusive source of hemoptysis. ABBREVIATIONS: ISA ϭ intersegmental artery; SIA ϭ supreme intercostal artery; VA ϭ vertebral artery he cervical portion of the vertebral artery (VA) is formed by a bral arteria lusoria8-13 or persistent left seventh cervical ISA of Tseries of anastomoses established between the first 6 cervical aortic origin.14 intersegmental arteries (ISAs) and one of the carotid-vertebral This report discusses 9 angiographic observations of descend- anastomoses, the proatlantal artery.1-3 The VA is labeled a “post- ing thoracic VAs and 2 cases of ascending thoracic VAs. costal” anastomotic chain (ie, located behind the costal process of cervical vertebrae or dorsal to the rib itself at the thoracic level) to CASE SERIES emphasize its location within the transverse foramina. -

Product Information
G30 Latin VASA CAPITIS et CERVICIS ORGANA INTERNA 1 V. frontalis 49 Pulmo sinister 2 V. temporalis superficialis 50 Atrium dextrum 3 A. temporalis superficialis 51 Atrium sinistrum 3 a A. maxillaris 52 Ventriculus dexter 4 A. occipitalis 53 Ventriculus sinister 5 A. supratrochlearis 54 Valva aortae 6 A. et V. angularis 55 Valva trunci pulmonalis 7 A. et V. facialis 56 Septum interventriculare 7 a A. lingualis 57 Diaphragma 9 V. retromandibularis 58 Hepar 10 V. jugularis interna 11 A. thyroidea superior VASA ORGANORUM INTERNORUM 12 A. vertebralis 59 Vv. hepaticae 13 Truncus thyrocervicalis 60 V. gastrica dextra et sinistra 14 Truncus costocervicalis 61 A. hepatica communis 15 A. suprascapularis 61 a Truncus coeliacus 16 A. et V. subclavia dextra 62 V. mesenterica superior 17 V. cava superior 63 V. cava inferior 18 A. carotis communis 64 A. et V. renalis 18 a A. carotis externa 65 A. mesenterica superior 19 Arcus aortae 66 A. et V. lienalis 20 Pars descendens aortae 67 A. gastrica sinistra 68 Pars abdominalis® aortae VASA MEMBRII SUPERIORIS 69 A. mesenterica inferior 21 A. et V. axillaris 22 V. cephalica VASA REGIONIS PELVINAE 22 a A. circumflexa humeri anterior 72 A. et V. iliaca communis 22 b A. circumflexa humeri posterior 73 A. et V. iliaca externa 23 A. thoracodorsalis 74 A. sacralis mediana 24 A. et V. brachialis 75 A. et V. iliaca interna 25 A. thoracoacromialis 26 A. subclavia sinistra VASA MEMBRI INFERIORIS 27 V. basilica 76 Ramus ascendens a. circumflexae femoris 28 A. collateralis ulnaris superior lateralis 29 A. ulnaris 77 Ramus descendens a. -

An Unusual Origin and Course of the Thyroidea Ima Artery, with Absence of Inferior Thyroid Artery Bilaterally
Surgical and Radiologic Anatomy (2019) 41:235–237 https://doi.org/10.1007/s00276-018-2122-1 ANATOMIC VARIATIONS An unusual origin and course of the thyroidea ima artery, with absence of inferior thyroid artery bilaterally Doris George Yohannan1 · Rajeev Rajan1 · Akhil Bhuvanendran Chandran1 · Renuka Krishnapillai1 Received: 31 May 2018 / Accepted: 21 October 2018 / Published online: 25 October 2018 © Springer-Verlag France SAS, part of Springer Nature 2018 Abstract We report an unusual origin and course of the thyroidea ima artery in a male cadaver. The ima artery originated from the right subclavian artery very close to origin of the right vertebral artery. The artery coursed anteriorly between the common carotid artery medially and internal jugular vein laterally. It then coursed obliquely, from below upwards, from lateral to medial superficial to common carotid artery, to reach the inferior pole of the right lobe of thyroid and branched repeatedly to supply the anteroinferior and posteroinferior aspects of both the thyroid lobes and isthmus. The superior thyroid arteries were normal. Both the inferior thyroid arteries were absent. The unusual feature of this thyroidea ima artery is its origin from the subclavian artery close to vertebral artery origin, the location being remarkably far-off from the usual near midline position, and the oblique and relatively superficial course. This report is a caveat to neck surgeons to consider such a superficially running vessel to be a thyroidea ima artery. Keywords Thyroid vascular anatomy · Thyroidea ima artery · Artery of Neubauer · Blood supply of thyroid · Variations Introduction (1.1%), transverse scapular (1.1%), or pericardiophrenic or thyrocervical trunk [8, 10].