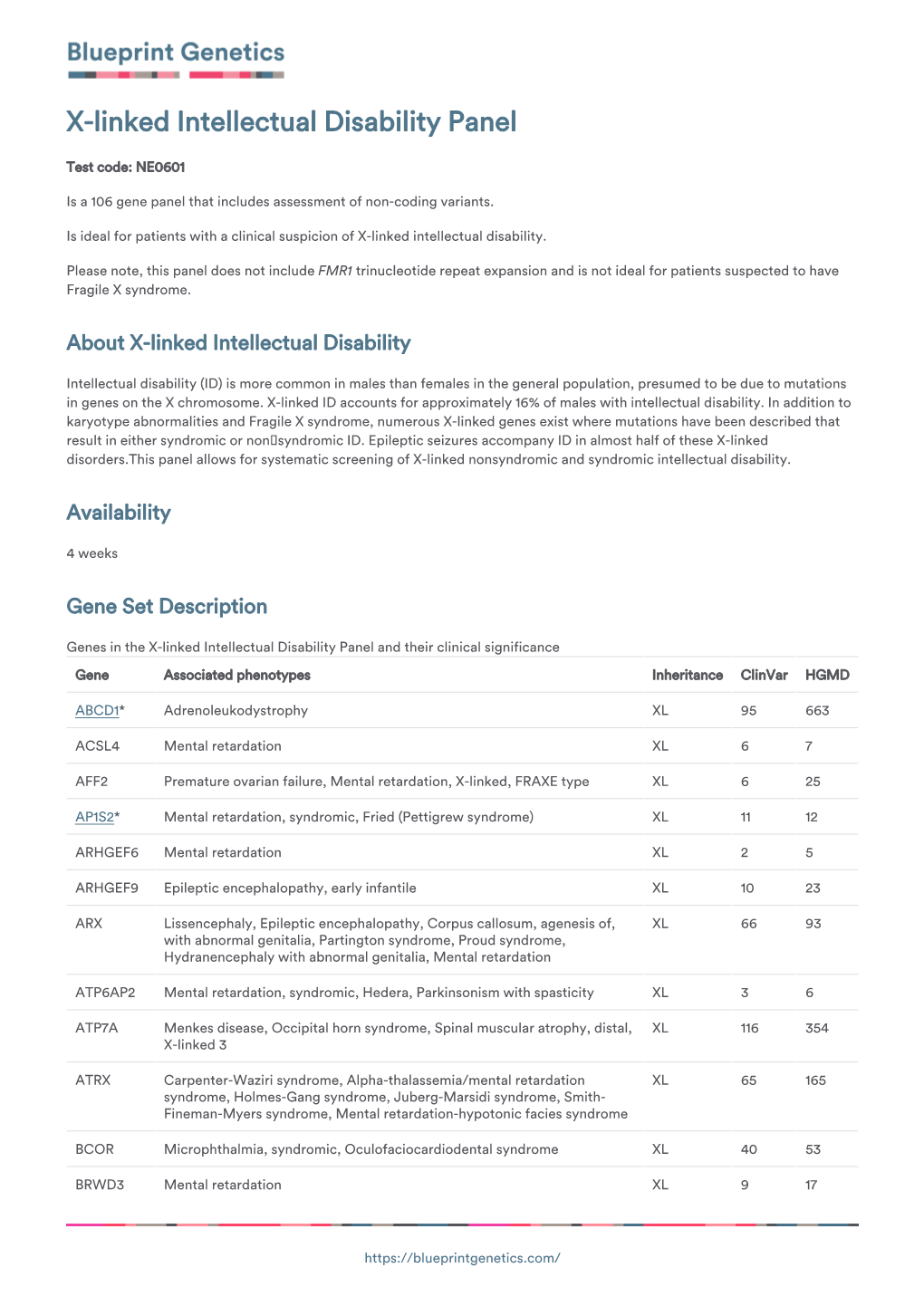
Blueprint Genetics X-Linked Intellectual Disability Panel
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reframing Psychiatry for Precision Medicine
Reframing Psychiatry for Precision Medicine Elizabeth B Torres 1,2,3* 1 Rutgers University Department of Psychology; [email protected] 2 Rutgers University Center for Cognitive Science (RUCCS) 3 Rutgers University Computer Science, Center for Biomedicine Imaging and Modelling (CBIM) * Correspondence: [email protected]; Tel.: (011) +858-445-8909 (E.B.T) Supplementary Material Sample Psychological criteria that sidelines sensory motor issues in autism: The ADOS-2 manual [1, 2], under the “Guidelines for Selecting a Module” section states (emphasis added): “Note that the ADOS-2 was developed for and standardized using populations of children and adults without significant sensory and motor impairments. Standardized use of any ADOS-2 module presumes that the individual can walk independently and is free of visual or hearing impairments that could potentially interfere with use of the materials or participation in specific tasks.” Sample Psychiatric criteria from the DSM-5 [3] that does not include sensory-motor issues: A. Persistent deficits in social communication and social interaction across multiple contexts, as manifested by the following, currently or by history (examples are illustrative, not exhaustive, see text): 1. Deficits in social-emotional reciprocity, ranging, for example, from abnormal social approach and failure of normal back-and-forth conversation; to reduced sharing of interests, emotions, or affect; to failure to initiate or respond to social interactions. 2. Deficits in nonverbal communicative behaviors used for social interaction, ranging, for example, from poorly integrated verbal and nonverbal communication; to abnormalities in eye contact and body language or deficits in understanding and use of gestures; to a total lack of facial expressions and nonverbal communication. -

Moderate the MAOA-L Allele Expression with CRISPR/Cas9 System
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 23 April 2018 doi:10.20944/preprints201804.0275.v1 1 Review 2 Moderate the MAOA-L Allele Expression with CRISPR/Cas9 System 3 Martin L. Nelwan 4 Department of Animal Science – Other 5 Nelwan Institution for Human Resource Development 6 Jl. A. Yani No. 24 7 Palu, Sulawesi Tengah, Indonesia 8 Email: [email protected] 9 Abstract: Antisocial behavior is a behavior disorder inherited according to the inheritance of X-linked 10 chromosome. Mutations in the MAOA gene can cause different behaviors in humans. These can comprise 11 violent behavior or antisocial behavior. Low MAOA (MAOA-L) allele activity can cause antisocial 12 behavior in both healthy and unhealthy people. Antisocial from healthy males can originate from 13 maltreatment during childhood. There are no drugs for the treatment of antisocial behavior permanently 14 at this time. MAOA inhibitor can reverse antisocial behavior in animal models. To cure antisocial 15 behavior in the future, the CRISPR/Cas9 system in combination with iPSCs or ssODN methods for 16 instance can be used. This system has succeeded to correct erroneous segments in the F8 gene and F9 17 gene. Both genes occupy the X chromosome. The MAOA gene also occupies the X chromosome. It seems 18 that CRISPR/Cas9 system may be a beneficial tool to edit erroneous segments in the MAOA gene to treat 19 antisocial behavior. 20 Keywords: advanced therapy, aggressive, antisocial, behavior, MAOA. 21 22 1. Introduction 23 Antisocial behavior is a hereditary disorder inherited through an X-linked recessive inheritance 24 pattern. -

Cell Death Via Lipid Peroxidation and Protein Aggregation Diseases
biology Review Cell Death via Lipid Peroxidation and Protein Aggregation Diseases Katsuya Iuchi * , Tomoka Takai and Hisashi Hisatomi Department of Materials and Life Science, Faculty of Science and Technology, Seikei University, 3-3-1 Kichijojikitamachi, Musashino-shi, Tokyo 180-8633, Japan; [email protected] (T.T.); [email protected] (H.H.) * Correspondence: [email protected] or [email protected]; Tel.: +81-422-37-3523 Simple Summary: It is essential for cellular homeostasis that biomolecules, such as DNA, proteins, and lipids, function properly. Disturbance of redox homeostasis produces aberrant biomolecules, including oxidized lipids and misfolded proteins, which increase in cells. Aberrant biomolecules are removed by excellent cellular clearance systems. However, when excess aberrant biomolecules remain in the cell, they disrupt organelle and cellular functions, leading to cell death. These aberrant molecules aggregate and cause apoptotic and non-apoptotic cell death, leading to various protein aggregation diseases. Thus, we investigated the cell-death cross-linking between lipid peroxidation and protein aggregation. Abstract: Lipid peroxidation of cellular membranes is a complicated cellular event, and it is both the cause and result of various diseases, such as ischemia-reperfusion injury, neurodegenerative diseases, and atherosclerosis. Lipid peroxidation causes non-apoptotic cell death, which is associated with cell fate determination: survival or cell death. During the radical chain reaction of lipid peroxidation, Citation: Iuchi, K.; Takai, T.; various oxidized lipid products accumulate in cells, followed by organelle dysfunction and the Hisatomi, H. Cell Death via Lipid induction of non-apoptotic cell death. Highly reactive oxidized products from unsaturated fatty acids Peroxidation and Protein are detected under pathological conditions. -

Multiple Interactions Between an Arf/GEF Complex and Charged Lipids Determine Activation Kinetics on the Membrane
Multiple interactions between an Arf/GEF complex and charged lipids determine activation kinetics on the membrane Deepti Karandura,b,1, Agata Nawrotekc,d,1, John Kuriyana,b,2, and Jacqueline Cherfilsc,d,2 aDepartment of Molecular and Cell Biology, University of California, Berkeley, CA 94720; bHoward Hughes Medical Institute, University of California, Berkeley, CA 94720; cLaboratoire de Biologie et Pharmacologie Appliquée, CNRS, Cachan 94235, France; and dEcole Normale Supérieure Paris-Saclay, Cachan 94235, France Edited by Satyajit Mayor, National Centre for Biological Sciences, Bangalore, India, and approved August 28, 2017 (received for review May 15, 2017) Lipidated small GTPases and their regulators need to bind to which is surrounded by an assortment of regulatory domains (9). membranes to propagate actions in the cell, but an integrated Sec7-assisted nucleotide exchangeoccursinastep-by-step manner, understanding of how the lipid bilayer exerts its effect has whereby the Sec7 domain binds to the switch 1 and switch 2 regions remained elusive. Here we focused on ADP ribosylation factor of Arf to remodel the interswitch and inserts an invariant gluta- (Arf) GTPases, which orchestrate a variety of regulatory functions mate into the nucleotide-binding site to displace GDP (6, 7, 10). in lipid and membrane trafficking, and their activation by the In metazoans, Arf GTPases are activated at the plasma mem- guanine-nucleotide exchange factor (GEF) Brag2, which controls brane and on endosomes by members of three ArfGEF subfamilies: integrin endocytosis and cell adhesion and is impaired in cancer cytohesins, EFA6, and Brag/IQSEC. These ArfGEFs share a com- and developmental diseases. Biochemical and structural data are mon organization in which the Sec7 domain is immediately followed available that showed the exceptional efficiency of Arf activation by a pleckstrin homology (PH) domain that binds phosphoinositide by Brag2 on membranes. -

The Advantage of Genome-Wide Microarrays Over Targeted Approaches
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/70828 Please be advised that this information was generated on 2021-09-24 and may be subject to change. COPY NUMBER VARIATION AND MENTAL RETARDATION opmaak koolen.indd 1 10-09-2008 10:11:31 Copy number variation and mental retardation The studies presented in this thesis were performed at the Department of Human Genetics, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. The research was supported by a grant from the Netherlands Organization for Health Research and Development (ZonMw). Publication of this thesis was financially supported by the Department of Human Genetics, Radboud University Nijmegen Medical Center, Nijmegen, the Netherlands. ISBN/EAN 978-90-6464-290-6 © 2008 D.A. Koolen All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, by print or otherwise, without permission in writing from the author. Cover photo: Printed by: Ponsen & Looijen B.V., Wageningen opmaak koolen.indd 2 10-09-2008 10:11:31 Copy number variation and mental retardation Een wetenschappelijke proeve op het gebied van de Medische Wetenschappen Proefschrift ter verkrijging van de graad doctor aan de Radboud Universiteit Nijmegen op gezag van de rector magnificus prof. mr. S.C.J.J. Kortmann, volgens besluit van het College van Decanen in het openbaar te verdedigen op donderdag 6 november 2008 om 15.30 uur precies door David Aljosja Koolen geboren op 22 juni 1976 te ‘s-Gravenhage opmaak koolen.indd 3 10-09-2008 10:11:32 Promotor: Prof. -

Childhood Cerebral X-Linked Adrenoleukodystrophy with Atypical Neuroimaging Abnormalities and a No…
9/28/2018 Journal of Postgraduate Medicine: Childhood cerebral X-linked adrenoleukodystrophy with atypical neuroimaging abnormalities and a no… Open access journal indexed with Index Medicus & EMBASE Home | Subscribe | Feedback [Download PDF] CASE REPORT Year : 2018 | Volume : 64 | Issue : 1 | Page : 59-63 Childhood cerebral X-linked adrenoleukodystrophy with atypical neuroimaging abnormalities and a novel mutation M Muranjan1, S Karande1, S Sankhe2, S Eichler3, 1 Department of Pediatrics, Seth GS Medical College and KEM Hospital, Parel, Mumbai, Maharashtra, India 2 Department of Radiology, Seth GS Medical College and KEM Hospital, Parel, Mumbai, Maharashtra, India 3 Centogene AG, Schillingallee 68, Rostock, Germany Correspondence Address: Dr. M Muranjan Department of Pediatrics, Seth GS Medical College and KEM Hospital, Parel, Mumbai, Maharashtra India Abstract Childhood cerebral X-linked adrenoleukodystrophy (XALD) typically manifests with symptoms of adrenocortical insufficiency and a variety of neurocognitive and behavioral abnormalities. A major diagnostic clue is the characteristic neuroinflammatory parieto-occipital white matter lesions on magnetic resonance imaging. This study reports a 5-year 10-month old boy presenting with generalized skin hyperpigmentation since 3 years of age. Over the past 9 months, he had developed right-sided hemiparesis and speech and behavioral abnormalities, which had progressed over 5 months to bilateral hemiparesis. Retrospective analyses of serial brain magnetic resonance images revealed an unusual pattern of lesions involving the internal capsules, corticospinal tracts in the midbrain and brainstem, and cerebellar white matter. The clinical diagnosis of childhood cerebral adrenoleukodystrophy was confirmed by elevated basal levels of adrenocorticotropin hormone and plasma very long chain fatty acid levels. Additionally, sequencing of the ABCD1 gene revealed a novel mutation. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Cdc42 and Rac1 Activity Is Reduced in Human Pheochromocytoma and Correlates with FARP1 and ARHGEF1 Expression
234 P Croisé et al. Rho-GTPase activity in human 23:4 281–293 Research pheochromocytoma Cdc42 and Rac1 activity is reduced in human pheochromocytoma and correlates with FARP1 and ARHGEF1 expression Pauline Croisé1, Sébastien Houy1, Mathieu Gand1, Joël Lanoix2, Valérie Calco1, Petra Tóth1, Laurent Brunaud3, Sandra Lomazzi4, Eustache Paramithiotis2, Daniel Chelsky2, Stéphane Ory1,* and Stéphane Gasman1,* Correspondence 1Institut des Neurosciences Cellulaires et Intégratives (INCI), CNRS UPR 3212, Strasbourg, France should be addressed 2Caprion Proteome, Inc., Montréal, Québec, Canada to S Ory or S Gasman 3Service de Chirurgie Digestive, Hépato-bilaire et Endocrinienne, CHRU Nancy, Hôpitaux de Brabois, Email Vandoeuvre les Nancy, France [email protected] or 4Centre de Ressources Biologiques (CRB), CHRU Nancy, Hôpitaux de Brabois, Vandoeuvres les Nancy, France [email protected] *(S Ory and S Gasman contributed equally to this work) Abstract Among small GTPases from the Rho family, Cdc42, Rac, and Rho are well known to mediate Key Words a large variety of cellular processes linked with cancer biology through their ability to cycle f Rho-GTPases between an inactive (GDP-bound) and an active (GTP-bound) state. Guanine nucleotide f pheochromocytoma exchange factors (GEFs) stimulate the exchange of GDP for GTP to generate the activated f mass spectrometry form, whereas the GTPase-activating proteins (GAPs) catalyze GTP hydrolysis, leading to f Rho-GEF Endocrine-Related Cancer Endocrine-Related the inactivated form. Modulation of Rho GTPase activity following altered expression of Rho-GEFs and/or Rho-GAPs has already been reported in various human tumors. However, nothing is known about the Rho GTPase activity or the expression of their regulators in human pheochromocytomas, a neuroendocrine tumor (NET) arising from chromaffin cells of the adrenal medulla. -

Neurodegenerative Triplet Repeat Expansion Disorders
The Pharma Innovation Journal 2018; 7(11): 34-40 ISSN (E): 2277- 7695 ISSN (P): 2349-8242 NAAS Rating: 5.03 Neurodegenerative triplet repeat expansion disorders: TPI 2018; 7(11): 34-40 © 2018 TPI A review www.thepharmajournal.com Received: 15-09-2018 Accepted: 20-10-2018 Mitesh Patel, RK Patel, Tushar Chauhan, Jigar Suthar and Sanjay Dave Mitesh Patel Genetics Group of Gujarat Abstract Diagnostic Centre, Mehsana, Epigenetic alterations are the major causes of triplet repeat expansion. The repetitive DNA expands of its Gujarat, India normal length results in sever neurodegenerative conditions. The common types of triplet repeat expansion (TNE) disorders are: Huntington disease, Friedreich ataxia, myotonic dystrophy, SBMA and RK Patel SCA1 out of which Huntington disease, SBMA and SCA1 are categorized as a poly glutamine disorder Sandor Animal Biogenics Pvt. due to the repeat of CAG. In contrast, the friedreich ataxia is occurred due to expansion of the GAA Ltd., Hyderabad, Telangana, whereas myotonic dystrophy is due to the expansion of CTG. The triplet disease follows the mechanism India of anticipation in which the onset of the disease increases with age. Conclusively, no clear mechanism can explain the origin of the disease. The pre mutation can be expanded in full mutation in successive Tushar Chauhan Genetics Group of Gujarat generations and the number of repeats increased with each generation. TNE can observe in both somatic Diagnostic Centre, Mehsana, as well as germ line tissues. Gujarat, India Keywords: triplet repeat expansion disorder, trinucleotide repeats, Huntington disease, SBMA, SCA1, Jigar Suthar friedreich ataxia Genetics Group of Gujarat Diagnostic Centre, Mehsana, Introduction Gujarat, India Since the early 1990s, a new class of molecular disease has been characterized based upon the Sanjay Dave presence of unstable and abnormal expansions of DNA-triplets (Trinucleotides). -

Focus on Cdc42 in Breast Cancer: New Insights, Target Therapy Development and Non-Coding Rnas
Review Focus on Cdc42 in Breast Cancer: New Insights, Target Therapy Development and Non-Coding RNAs Yu Zhang †, Jun Li †, Xing-Ning Lai, Xue-Qiao Jiao, Jun-Ping Xiong and Li-Xia Xiong * Department of Pathophysiology, Jiangxi Province Key Laboratory of Tumor Pathogenesis and Molecular Pathology, Medical College, Nanchang University, 461 Bayi Road, Nanchang 330006, China; [email protected] (Y.Z.); [email protected] (J.L.); [email protected] (X.-N.L.); [email protected] (X.-Q.J.); [email protected] (J.-P.X.) * Correspondence: [email protected]; Tel.: +86-791-8636-0556 † These authors contributed equally to this work. Received: 30 December 2018; Accepted: 8 February 2019; Published: 11 February 2019 Abstract: Breast cancer is the most common malignant tumors in females. Although the conventional treatment has demonstrated a certain effect, some limitations still exist. The Rho guanosine triphosphatase (GTPase) Cdc42 (Cell division control protein 42 homolog) is often upregulated by some cell surface receptors and oncogenes in breast cancer. Cdc42 switches from inactive guanosine diphosphate (GDP)-bound to active GTP-bound though guanine-nucleotide- exchange factors (GEFs), results in activation of signaling cascades that regulate various cellular processes such as cytoskeletal changes, proliferation and polarity establishment. Targeting Cdc42 also provides a strategy for precise breast cancer therapy. In addition, Cdc42 is a potential target for several types of non-coding RNAs including microRNAs and lncRNAs. These non-coding RNAs is extensively involved in Cdc42-induced tumor processes, while many of them are aberrantly expressed. Here, we focus on the role of Cdc42 in cell morphogenesis, proliferation, motility, angiogenesis and survival, introduce the Cdc42-targeted non-coding RNAs, as well as present current development of effective Cdc42-targeted inhibitors in breast cancer. -

Genes in Eyecare Geneseyedoc 3 W.M
Genes in Eyecare geneseyedoc 3 W.M. Lyle and T.D. Williams 15 Mar 04 This information has been gathered from several sources; however, the principal source is V. A. McKusick’s Mendelian Inheritance in Man on CD-ROM. Baltimore, Johns Hopkins University Press, 1998. Other sources include McKusick’s, Mendelian Inheritance in Man. Catalogs of Human Genes and Genetic Disorders. Baltimore. Johns Hopkins University Press 1998 (12th edition). http://www.ncbi.nlm.nih.gov/Omim See also S.P.Daiger, L.S. Sullivan, and B.J.F. Rossiter Ret Net http://www.sph.uth.tmc.edu/Retnet disease.htm/. Also E.I. Traboulsi’s, Genetic Diseases of the Eye, New York, Oxford University Press, 1998. And Genetics in Primary Eyecare and Clinical Medicine by M.R. Seashore and R.S.Wappner, Appleton and Lange 1996. M. Ridley’s book Genome published in 2000 by Perennial provides additional information. Ridley estimates that we have 60,000 to 80,000 genes. See also R.M. Henig’s book The Monk in the Garden: The Lost and Found Genius of Gregor Mendel, published by Houghton Mifflin in 2001 which tells about the Father of Genetics. The 3rd edition of F. H. Roy’s book Ocular Syndromes and Systemic Diseases published by Lippincott Williams & Wilkins in 2002 facilitates differential diagnosis. Additional information is provided in D. Pavan-Langston’s Manual of Ocular Diagnosis and Therapy (5th edition) published by Lippincott Williams & Wilkins in 2002. M.A. Foote wrote Basic Human Genetics for Medical Writers in the AMWA Journal 2002;17:7-17. A compilation such as this might suggest that one gene = one disease. -

Centre for Arab Genomic Studies a Division of Sheikh Hamdan Award for Medical Sciences
Centre for Arab Genomic Studies A Division of Sheikh Hamdan Award for Medical Sciences The Catalogue for Transmission Genetics in Arabs CTGA Database tRNA Methyltransferase 1, S. Cerevisiae, Homolog of Alternative Names planus. These findings are further bolstered by the TRMT1 fact that mutations in two other RNA- N2,N2-Dimethylguanosine-26 tRNA methyltransferase genes, NSUN2 and FTSJ1, have Methyltransferase been associated with intellectual disability. tRNA(m(2,2)G26)Dimethyltransferase Record Category Molecular Genetics Gene locus The TRMT1 gene is located on the short arm of chromosome 19 and spans a length of 12.6 kb of WHO-ICD DNA. Its coding sequence is spread across 18 N/A to gene loci exons and it encodes a 72.2 kDa protein product comprised of 659 amino acids. An additional 69.3 Incidence per 100,000 Live Births kDa isoform of the TRMT1 protein exists due to an N/A to gene loci alternatively spliced transcript variant. The gene is widely expressed in the human body, particularly in OMIM Number the nervous system, intestine, spleen, kidney and 611669 lung. Mode of Inheritance Epidemiology in the Arab World N/A to gene loci Saudi Arabia Monies et al. (2017) studied the findings of 1000 Gene Map Locus diagnostic panels and exomes carried out at a next 19p13.13 generation sequencing lab in Saudi Arabia. One patient, a 13-year-old male, presented with speech Description delay, intellectual disability, learning disability, The TRMT1 gene encodes a methyltransferase hypotonia and seizures. Using whole exome enzyme that acts on tRNA. This enzyme, which sequencing, a homozygous mutation consists of a zinc finger motif and an (c.1245_1246del, p.L415fs) was identified in exon arginine/proline rich region at its C-terminus, is 10 of the patient’s TRMT1 gene.