Ear Disorders External Ear Congenital Aural Atresia (744.01)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -

Direct Sagittal CT in the Evaluation of Temporal Bone Disease
371 Direct Sagittal CT in the Evaluation of Temporal Bone Disease 1 Mahmood F. Mafee The human temporal bone is an extremely complex structure. Direct axial and coronal Arvind Kumar2 CT sections are quite satisfactory for imaging the anatomy of the temporal bone; Christina N. Tahmoressi1 however, many relationships of the normal and pathologic anatomic detail of the Barry C. Levin2 temporal bone are better seen with direct sagittal CT sections. The sagittal projection Charles F. James1 is of interest to surgeons, as it has the advantage of following the plane of surgical approach. This article describes the advantages of using direct sagittal sections for Robert Kriz 1 1 studying various diseases of the temporal bone. The CT sections were obtained with Vlastimil Capek the aid of a new headholder added to our GE CT 9800 scanner. The direct sagittal projection was found to be extremely useful for evaluating diseases involving the vertical segment of the facial nerve canal, vestibular aqueduct, tegmen tympani, sigmoid sinus plate, sinodural angle, carotid canal, jugular fossa, external auditory canal, middle ear cavity, infra- and supra labyrinthine air cells, and temporo mandibular joint. CT has contributed greatly to an understanding of the complex anatomy and spatial relationship of the minute structures of the hearing and balance organs, which are packed into a small pyramid-shaped petrous temporal bone [1 , 2]. In the past 6 years, high-resolution CT scanning has been rapidly replacing standard tomography and has proved to be the diagnostic imaging method of choice for studying the normal and pathologic details of the temporal bone [3-14]. -

Definitions and Background
1 Definitions and Background Tinnitus is a surprisingly complex subject. Numer- ears.” And, in fact, the word “tinnitus” is derived ous books would be required to adequately cover the from the Latin word tinniere, which means “to current body of knowledge. The present handbook ring.” Patients report many different sounds—not focuses on describing procedures for providing just ringing—when describing the sound of their clinical services for tinnitus using the methodology tinnitus, as we discuss later in this chapter. of progressive tinnitus management (PTM). In this opening chapter we establish common ground with respect to terminology and contextual Transient Ear Noise information. Relevant definitions are provided, many of which are operational due to lack of consensus It seems that almost everyone experiences “tran- in the field. Additional background information sient ear noise,” which typically is described as a includes brief descriptions of epidemiologic data, sudden whistling sound accompanied by the per- patient data, and conditions related to reduced tol- ception of hearing loss (Kiang, Moxon, & Levine, erance (hypersensitivity) to sound. 1970). No systematic studies have been published to date describing the prevalence and properties of transient ear noise; thus, anything known about Basic Concepts and Terminology this phenomenon is anecdotal. The transient auditory event is unilateral and seems to occur completely at random without any- Tinnitus is the experience of perceiving sound that thing precipitating the sudden onset of symptoms. is not produced by a source outside of the body. The Often the ear feels blocked during the episode. The “phantom” auditory perception is generated some- symptoms generally dissipate within a period of where in the auditory pathways or in the head or about a minute. -
Tympanic Membrane Perforations: the Safe Versus the Unsafe
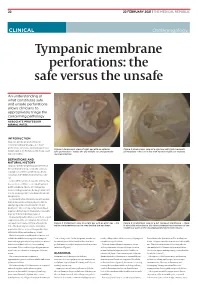
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -

Bachmann.Pdf
Pediatric Vestibular Dysfunction: More Than a Balancing Act Kay Bachmann, PhD 1 2 Introduction Childhood Hearing Loss 1. The learner will be able to identify 3 causes of vestibular • 1.4 in 1,000 newborns have hearing loss (CDC) disorders in children. • 5 in 1,000 children have hearing loss ages 3-17 yrs (CDC) 2. The learner will be able to identify at least 3 common symptoms of vestibular dysfunction in children. 3. The learner will be able to administer a short screening to assess balance function in children. 3 4 1 Childhood Vestibular Loss • Balance disorders may make up .45% of chief complaints per chart review in a Pediatric ENT department. (O’Reilly et al 2010) • Children with hearing impairment are twice as likely to have vestibular loss than healthy children • Studies show vestibular loss in 30-79% of children with HL • There is 10% increase in vestibular loss as a result of trauma from receiving a CI (Jacot et al, 2009) 5 6 Common Disorders with Hearing Loss and Vestibular Abnormalities • Syndromes What Does a Typically Functioning Vestibular System Do? – Usher Syndrome Type 1 – Pendred Syndrome (also non syndromic Enlarged vestibular Aqueduct Syndrome) Two Main Reflexes: – Branchio-oto-renal Syndrome Vestibular Ocular Reflex- Helps hold an object – CHARGE association steady when the head/body are in motion. • Cochlear Malformations • VIII Nerve Defects • Cytomegalovirus (CMV) Vestibular Spinal Reflex- Helps keep our posture • Meningitis • Cochlear implant patients and body steady when it senses movement. 7 8 2 What Does an -
Instruction Sheet: Otitis Externa
University of North Carolina Wilmington Abrons Student Health Center INSTRUCTION SHEET: OTITIS EXTERNA The Student Health Provider has diagnosed otitis externa, also known as external ear infection, or swimmer's ear. Otitis externa is a bacterial/fungal infection in the ear canal (the ear canal goes from the outside opening of the ear to the eardrum). Water in the ear, from swimming or bathing, makes the ear canal prone to infection. Hot and humid weather also predisposes to infection. Symptoms of otitis externa include: ear pain, fullness or itching in the ear, ear drainage, and temporary loss of hearing. These symptoms are similar to those caused by otitis media (middle ear infection). To differentiate between external ear infection and middle ear infection, the provider looks in the ear with an instrument called an otoscope. It is important to distinguish between the two infections, as they are treated differently: External otitis is treated with drops in the ear canal, while middle ear infection is sometimes treated with an antibiotic by mouth. MEASURES YOU SHOULD TAKE TO HELP TREAT EXTERNAL EAR INFECTION: 1. Use the ear drops regularly, as directed on the prescription. 2. The key to treatment is getting the drops down into the canal and keeping the medicine there. To accomplish this: Lie on your side, with the unaffected ear down. Put three to four drops in the infected ear canal, then gently pull the outer ear back and forth several times, working the medicine deeper into the ear canal. Remain still, good-ear-side-down for about 15 minutes. -

Noise-Induced Cochlear Neuronal Degeneration and Its Role in Hyperacusis- and Tinnitus-Like Behavior
Noise-Induced Cochlear Neuronal Degeneration and Its Role in Hyperacusis- and Tinnitus-Like Behavior by Ann E. Hickox B.A. French Arizona State University, 2006 MSc Speech and Hearing Sciences University College London, 2007 SUBMITTED TO THE HARVARD-MIT DIVISION OF HEALTH SCIENCES AND TECHNOLOGY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN SPEECH AND HEARING BIOSCIENCE AND TECHNOLOGY AT THE MASSACHUSETTS INSTITUTE OF TECHNOLOGY FEBRUARY 2013 @2013 Ann E. Hickox. All rights reserved The author hereby grants to MIT permission to reproduce and to distribute publicly paper and electronic copies of this thesis document in whole or in part in any medium now known or hereafter created. Signature of Author: Ann E. Hickox Harvard-MIT Division of e lthSciences and Technology f/ / I / January 2, 2013 Certified by: M. Charles Liberman, Ph.D. Thesis Supervisor Director, Eaton-Peabody Laboratory, Massachusetts Eye & Ear Infirmary Harold F. Schuknecht Professor of Otology and Laryngology, Harvard Medical School Accepted by Emery Brown, MD, PhD Director, Harvard-MIT Division of Health Sciences and Technology Professor of Computational Neuroscience and Health Sciences and Technology 1 2 Noise-Induced Cochlear Neuronal Degeneration and Its Role in Hyperacusis- and Tinnitus-Like Behavior by Ann E. Hickox Submitted to the Harvard-MIT Division of Health Sciences and Technology on January 2, 2013 in partial fulfillment of the requirements for the Degree of Doctor of Philosophy in Speech and Hearing Bioscience and Technology Abstract Perceptual abnormalities such as hyperacusis and tinnitus often occur following acoustic overexposure. Although such exposure can also result in permanent threshold elevation, some individuals with noise-induced hyperacusis or tinnitus show clinically normal thresholds. -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired -

Hearing Loss, Vertigo and Tinnitus
HEARING LOSS, VERTIGO AND TINNITUS Jonathan Lara, DO April 29, 2012 Hearing Loss Facts S Men are more likely to experience hearing loss than women. S Approximately 17 percent (36 million) of American adults report some degree of hearing loss. S About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. S Nine out of every 10 children who are born deaf are born to parents who can hear. Hearing Loss Facts S The NIDCD estimates that approximately 15 percent (26 million) of Americans between the ages of 20 and 69 have high frequency hearing loss due to exposure to loud sounds or noise at work or in leisure activities. S Only 1 out of 5 people who could benefit from a hearing aid actually wears one. S Three out of 4 children experience ear infection (otitis media) by the time they are 3 years old. Hearing Loss Facts S There is a strong relationship between age and reported hearing loss: 18 percent of American adults 45-64 years old, 30 percent of adults 65-74 years old, and 47 percent of adults 75 years old or older have a hearing impairment. S Roughly 25 million Americans have experienced tinnitus. S Approximately 4,000 new cases of sudden deafness occur each year in the United States. Hearing Loss Facts S Approximately 615,000 individuals have been diagnosed with Ménière's disease in the United States. Another 45,500 are newly diagnosed each year. S One out of every 100,000 individuals per year develops an acoustic neurinoma (vestibular schwannoma). -

Tinnitus & Hyperacusis
REFERENCE Tinnitus & Hyperacusis GlossarY The American Tinnitus Association (ATA) is pleased to provide our readers with a glossary of terms pertaining to tinnitus and hyperacusis. It has been adapted with permission from a document published with the Progressive Tinnitus Management program developed by researchers and clinicians at the Veterans Health Administration. The ATA Tinnitus & Hyperacusis Glossary was edited by members of the Tinnitus Today Editorial Advisory Panel. The terminology used to describe any condition is of vital importance to diagnosis and treatment of the condition. Without a commonly understood set of terms, we could not effectively communicate a diagnosis, direct treatment for conditions, or expect patients to understand and follow those treatments accurately. www.ATA.org TINNITUS TODay WIntER 2017 33 REFERENCE Acceptance and Commitment aminoglycoside antibiotics: Any by neural networks that respond to Therapy (ACT): A psychotherapeutic of a group of antibiotics derived from different levels of sound. approach similar to Cognitive Behav- various species of Streptomyces that auditory hallucinations: Usually ioral Therapy (CBT), and sometimes is inhibit bacterial protein synthesis and perceived as voices or music (and referenced as part of the third wave of are active against gram-negative bac- sometimes as environmental sounds, CBT approaches. ACT involves mind- teria, in particular. Aminoglycosides e.g., a barking dog), and have been fulness, which is aimed at reducing include streptomycin, gentamicin, studied primarily in the context of psychological distress, depressive amikacin, kanamycin, tobramycin, and mental health. Some individuals who symptoms, and anxiety by focusing on neomycin, among others. All can be experience auditory hallucinations do the present moment. -
Secondary Endolymphatic Hydrops
PO BOX 13305 · PORTLAND, OR 97213 · FAX: (503) 229-8064 · (800) 837-8428 · [email protected] · WWW.VESTIBULAR.ORG Secondary Endolymphatic Hydrops By Susan Pesznecker, RN; Legacy Clinical Research & Technology Center, Portland, Oregon with the Vestibular Disorders Association Endolymphatic hydrops is a disorder of controls are believed to be lost or the vestibular system. Although its damaged. This may cause the volume and underlying cause and natural history are concentration of the endolymph to unknown, it is believed to result from fluctuate in response to changes in the abnormalities in the quantity, body’s circulatory fluids and electrolytes. composition, and/or pressure of the endolymph (the fluid within the Symptoms endolymphatic sac, a compartment of the Symptoms typical of hydrops include inner ear). pressure or fullness in the ears (aural fullness), tinnitus (ringing or other noise Causes in the ears), hearing loss, dizziness, and Endolymphatic hydrops may be either imbalance. primary or secondary. Primary idiopathic endolymphatic hydrops (known as Diagnosis and testing Ménière’s disease) occurs for no known There is no vestibular or auditory test reason. Secondary endolymphatic that is diagnostic of endolymphatic hydrops appears to occur in response to hydrops. Diagnosis is clinical—based on an event or underlying condition. For the physician’s observations and on the example, it can follow head trauma or ear patient’s history, symptoms, and surgery, and it can occur with other inner symptom pattern. The clinical diagnosis ear disorders, allergies, or systemic may be strengthened by the results of disorders (such as diabetes or certain tests. For example, certain autoimmune disorders). -

Counseling for Patients with Hyperacusis Mary Maraist
Augustana College Augustana Digital Commons Communication Sciences and Disorders: Student Communication Sciences and Disorders Scholarship & Creative Works 5-2019 Counseling for Patients with Hyperacusis Mary Maraist Follow this and additional works at: https://digitalcommons.augustana.edu/csdstudent Part of the Cognitive Behavioral Therapy Commons, Sense Organs Commons, Speech and Hearing Science Commons, and the Speech Pathology and Audiology Commons HYPERACUSIS COUNSELING MATERIALS 1 Counseling for Patients with Hyperacusis Mary Maraist CSD490: Senior Inquiry, Spring 2019 Ann Perreau, Ph.D., Thesis Advisor Augustana College HYPERACUSIS COUNSELING MATERIALS 2 Acknowledgements Firstly I would to thank Dr. Ann Perreau for introducing me to the topic of hyperacusis and for being an integral part of this project. I'm very thankful for all all of the support and expertise she has lent me throughout my time at Augustana and this project. She also contacted the participants for this project, which was incredibly helpful. On that note, I would like to thank the individuals who participated in this project. Their participation and flexibility was a crucial part of this process, and I'm very appreciative of the time they took to be a part of this project. My friends and family also deserve thanks as they have helped me work through challenges and and have supported me throughout my education. Thank you to all who have made an impression on my time at Augustana and who will continue to motivate me in the future. HYPERACUSIS COUNSELING MATERIALS 3 Abstract Hyperacusis is the phenomenon of experiencing moderately loud sounds as overly loud and/or intensely annoying.