Respiratory Function CHAPTER Whenyouseethisicon,Usethecodeatfrontofbooktoaccessonlinestudentresources
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

X-Ray Interpretation
Objectives Describe a systematic method for interpretation of chest and abdomen x-rays List findings to accurately identify common X-ray Interpretation pathology in chest & abdomen x-rays Describe a systematic method to approach the Denise Ramponi, DNP, FNP-C, ENP-BC, FAANP, FAEN important components in interpretation of upper & lower extremity x-rays Chest X-ray: Standard Views Lateral Film Postero-anterior (PA): (LAT) view can determine th On inspiration – diaphragm descends to 10 rib the anterior-posterior posteriorly structures along the axis of the body Normal LAT film Counting Ribs AP View - Portable http://www.lumen.luc.edu/lumen/MedEd/medicine/pulmonar/cxr/cxr_f.htm When the patient is unable to tolerate routine views with pts sitting or supine No participation from the patient Film is against the patient's back (supine) 1 Consolidation, Atelectasis, Chest radiograph Interstitial involvement Consolidation - any pathologic process that fills the alveoli with Left and right heart fluid, pus, blood, cells or other borders well defined substances Interstitial - involvement of the Both hemidiaphragms supporting tissue of the lung visible to midline parenchyma resulting in fine or coarse reticular opacities Right - higher Atelectasis - collapse of a part of Heart less than 50% of the lung due to a decrease in the amount of air resulting in volume diameter of the chest loss and increased density. Infiltrate, Consolidation vs. Congestive Heart Failure Atelectasis Fluid leaking into interstitium Kerley B 2 Kerley B lines Prominent interstitial markings Kerley lines Magnified CXR Cardiomyopathy & interstitial pulmonary edema Short 1-2 cm white lines at lung periphery horizontal to pleural surface Distended interlobular septa - secondary to interstitial edema. -

Infections of the Respiratory Tract
F70954-07.qxd 12/10/02 7:36 AM Page 71 Infections of the respiratory 7 tract the nasal hairs and by inertial impaction with mucus- 7.1 Pathogenesis 71 covered surfaces in the posterior nasopharynx (Fig. 11). 7.2 Diagnosis 72 The epiglottis, its closure reflex and the cough reflex all reduce the risk of microorganisms reaching the lower 7.3 Management 72 respiratory tract. Particles small enough to reach the tra- 7.4 Diseases and syndromes 73 chea and bronchi stick to the respiratory mucus lining their walls and are propelled towards the oropharynx 7.5 Organisms 79 by the action of cilia (the ‘mucociliary escalator’). Self-assessment: questions 80 Antimicrobial factors present in respiratory secretions further disable inhaled microorganisms. They include Self-assessment: answers 83 lysozyme, lactoferrin and secretory IgA. Particles in the size range 5–10 µm may penetrate further into the lungs and even reach the alveolar air Overview spaces. Here, alveolar macrophages are available to phagocytose potential pathogens, and if these are overwhelmed neutrophils can be recruited via the This chapter deals with infections of structures that constitute inflammatory response. The defences of the respira- the upper and lower respiratory tract. The general population tory tract are a reflection of its vulnerability to micro- commonly experiences upper respiratory tract infections, bial attack. Acquisition of microbial pathogens is which are often seen in general practice. Lower respiratory tract infections are less common but are more likely to cause serious illness and death. Diagnosis and specific chemotherapy of respiratory tract infections present a particular challenge to both the clinician and the laboratory staff. -

Upper Airway Obstruction in Children: Imaging Essentials
Acute upper airway obstruction in children: Imaging essentials Carlos J. Sivit MD Rainbow Babies and Children’s Hospital Case Western Reserve School of Medicine ►Clinical perspective ►Infections ►Foreign body ►Masses 1 Clinical Clinical ► Common cause of respiratory failure in children ► Potentially life-threatening in younger children because of smaller airway diameter ► Narrowing of upper airway has exponential effect on airflow 2 Clinical ► Majority of children are otherwise healthy ► Appropriate management results in good outcomes ► Improper management has dire consequences ► Imaging plays critical role in diagnosis Clinical ► Signs and symptoms § Respiratory distress § Dysphagia § Odynophagia § Stridor § Absence of air entry § Tachycardia 3 Stridor ► Harsh respiratory noise caused by turbulent air flow through narrowed airway ► Specific for severe upper airway obstruction ► Intensifies in inspiration ► Does not help specify nature or location Infections 4 Infections ► Acute laryngotracheobronchitis ► Acute epiglottitis ► Acute bacterial tracheitis ► Retropharyngeal abscess ► Infectious mononucleosis Croup ► Heterogenous group of acute infections characterized by brassy “croupy” cough ► May or may not be accompanied by stridor, hoarseness and respiratory distress ► Typically seen in younger children § 6 months – 5 years 5 Croup ► Parainfluenza viruses account for 75% ► Adenoviruses, RSV, influenza and measles cause most remaining cases ► Secondary bacterial infection is rare Imaging ►Imaging § Performed to exclude other conditions -
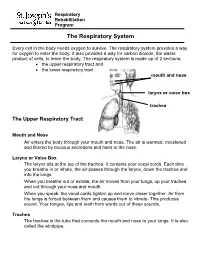
The Respiratory System
Respiratory Rehabilitation Program The Respiratory System Every cell in the body needs oxygen to survive. The respiratory system provides a way for oxygen to enter the body. It also provides a way for carbon dioxide, the waste product of cells, to leave the body. The respiratory system is made up of 2 sections: the upper respiratory tract and the lower respiratory tract mouth and nose larynx or voice box trachea The Upper Respiratory Tract Mouth and Nose Air enters the body through your mouth and nose. The air is warmed, moistened and filtered by mucous secretions and hairs in the nose. Larynx or Voice Box The larynx sits at the top of the trachea. It contains your vocal cords. Each time you breathe in or inhale, the air passes through the larynx, down the trachea and into the lungs. When you breathe out or exhale, the air moves from your lungs, up your trachea and out through your nose and mouth. When you speak, the vocal cords tighten up and move closer together. Air from the lungs is forced between them and causes them to vibrate. This produces sound. Your tongue, lips and teeth form words out of these sounds. Trachea The trachea is the tube that connects the mouth and nose to your lungs. It is also called the windpipe. The Lower Respiratory Tract Inside Lungs Outside Lungs bronchial tubes alveoli diaphragm (muscle) Bronchial Tubes The trachea splits into 2 bronchial tubes in your lungs. These are called the left bronchus and right bronchus. The bronchus tubes keep branching off into smaller and smaller tubes called bronchi. -

Since January 2020 Elsevier Has Created a COVID-19 Resource Centre with Free Information in English and Mandarin on the Novel Coronavirus COVID- 19
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IUPUIScholarWorks Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information website. Elsevier hereby grants permission to make all its COVID-19-related research that is available on the COVID-19 resource centre - including this research content - immediately available in PubMed Central and other publicly funded repositories, such as the WHO COVID database with rights for unrestricted research re-use and analyses in any form or by any means with acknowledgement of the original source. These permissions are granted for free by Elsevier for as long as the COVID-19 resource centre remains active. A02842_052 4/11/06 3:59 PM Page 813 Chapter 52 Otolaryngologic Disorders William P. Potsic and Ralph F. Wetmore EAR vibrating tympanic membrane to the stapes footplate. Anatomy Stapes movement creates a fluid wave in the inner ear that travels to the round window membrane and is dissi- The ear is divided into three anatomic and functional pated by reciprocal motion to the stapes. areas: the external ear, the middle ear, and the inner ear. There are two striated muscles in the middle ear. The The external ear consists of the auricle, external auditory tensor tympani muscle lies along the side of the eustachian canal, and the lateral surface of the tympanic membrane. tube, and its tendon attaches to the medial surface of the The auricle is a complex fibroelastic skeleton that is cov- malleus. -

RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J
OFP PATIENT EDUCATION HANDOUT RESPIRATORY TRACT INFECTIONS Peter Zajac, DO, FACOFP, Author Amy J. Keenum, DO, PharmD, Editor • Ronald Januchowski, DO, FACOFP, Health Literacy Editor HOME MANAGEMENT INCLUDES: • Drinking plenty of clear fuids and rest. Vitamin-C may help boost your immune system. Over-the-counter pain relievers such as acetaminophen and ibuprofen can be helpful for fevers and to ease any aches. Saline (salt) nose drops, lozenges, and vapor rubs can also help symptoms when used as directed by your physician. • A cool mist humidifer can make breathing easier by thinning mucus. • If you smoke, you should try to stop smoking for good! Avoid second-hand smoking also. • In most cases, antibiotics are not recommended because they are only effective if bacteria caused the infection. • Other treatments, that your Osteopathic Family Physician may prescribe, include Osteopathic Manipulative Therapy (OMT). OMT can help clear mucus, Respiratory tract infections are any relieve congestion, improve breathing and enhance comfort, relaxation, and infection that affect the nose, sinuses, immune function. and throat (i.e. the upper respiratory tract) or airways and lungs (i.e. the • Generally, the symptoms of a respiratory tract infection usually pass within lower respiratory tract). Viruses are one to two weeks. the main cause of the infections, but • To prevent spreading infections, sneeze into the arm of your shirt or in a tissue. bacteria can cause some. You can Also, practice good hygiene such as regularly washing your hands with soap and spread the infection to others through warm water. Wipe down common surfaces, such as door knobs and faucet handles, the air when you sneeze or cough. -

Respiratory Tract Infections in the Tropics
9.1 CHAPTER 9 Respiratory Tract Infections in the Tropics Tim J.J. Inglis 9.1 INTRODUCTION Acute respiratory infections are the single most common infective cause of death worldwide. This is also the case in the tropics, where they are a major cause of death in children under five. Bacterial pneumonia is particularly common in children in the tropics, and is more often lethal. Pulmonary tuberculosis is the single most common fatal infection and is more prevalent in many parts of the tropics due to a combination of endemic HIV infection and widespread poverty. A lack of diagnostic tests, limited access to effective treatment and some traditional healing practices exacerbate the impact of respiratory infection in tropical communities. The rapid urbanisation of populations in the tropics has increased the risk of transmitting respiratory pathogens. A combination of poverty and overcrowding in the peri- urban zones of rapidly expanding tropical cities promotes the epidemic spread of acute respiratory infection. PART A. INFECTIONS OF THE LOWER RESPIRATORY TRACT 9.2 PNEUMONIA 9.2.1 Frequency Over four million people die from acute respiratory infection per annum, mostly in developing countries. There is considerable overlap between these respiratory deaths and deaths due to tuberculosis, the single commonest fatal infection. The frequency of acute respiratory infection differs with location due to host, pathogen and environmental factors. Detailed figures are difficult to find and often need to be interpreted carefully, even for tuberculosis where data collection is more consistent. But in urban settings the enormity of respiratory infection is clearly evident. Up to half the patients attending hospital outpatient departments in developing countries have an acute respiratory infection. -

Control of Breathing in Mechanically Ventilated Patients
Eur Respir J, 1996, 9, 2151–2160 Copyright ERS Journals Ltd 1996 DOI: 10.1183/09031936.96.09102151 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 SERIES "CLINICAL PHYSIOLOGY IN RESPIRATORY INTENSIVE CARE" Edited by A. Rossi and C. Roussos Control of breathing in mechanically ventilated patients D. Georgopoulos, C. Roussos Control of breathing in mechanically ventilated patients. D. Georgopoulos, C. Roussos. Pulmonary and Critical Care Dept, General ©ERS Journals Ltd 1996. Hospital "G. Papanicolaou", University of ABSTRACT: During mechanical ventilation, the respiratory system is under the Thessaloniki, Thessaloniki, Greece and influence of two pumps, the ventilator pump and the patient's own respiratory Critical Care Dept, "Evangelismos" Hospital, muscles. Depending on the mode of mechanical ventilatory support, ventilation University of Athens, Athens, Greece. may be totally controlled by the ventilator or may be determined by the interac- Correspondence: D. Georgopoulos tion between patient respiratory effort and ventilator function. In either case, com- General Hospital "G. Papanicolaou" pared to spontaneous breathing, the breathing pattern is altered and this may Pulmonary Dept influence: 1) force-length and force-velocity relationships of respiratory muscles Respiratory Failure Unit (mechanical feedback); 2) chemical stimuli (chemical feedback); 3) the activity of Exochi 57010 various receptors located in the respiratory tract, lung and chest wall (reflex feed- Thessaloniki back); and 4) behavioural response (behavioural feedback). Changes in these feed- Greece back systems may modify the function of the ventilator, in a way that is dependent Keywords: Behavioural feedback on the mode of mechanical ventilatory support, ventilator settings, mechanics of chemical feedback the respiratory system and the sleep/awake stage. -

Large Airway Obstruction in Children Reprinted with Revisions from Update in Anaesthesia, (2004)18:44-49
Large airway obstruction in children Reprinted with revisions from Update in Anaesthesia, (2004)18:44-49. Originally Royal College of Anaesthetists Newsletter 1999; Issue 47: 159-162, reused with permission. N S Morton Correspondence Email: [email protected] PART 1: CAUSES AND ASSESSMENT The larynx is funnel shaped and is narrowest at the Opening and maintaining the airway is fundamental level of the cricoid ring compared with the cylindrical ommon emergencies to the treatment of all emergency situations in adult conformation, which is narrowest at the level of C paediatrics, as in adults. All resuscitation algorithms the vocal cords. The airway is more compressible as start with ABC (Airway, Breathing, Circulation) and cartilage support components are less well developed. must be qualified in trauma to include cervical spine Thus, extrinsic pressure from haematomas, neoplasms, Summary control. The commonest cause of paediatric airway vessels or enlarged heart chambers may more readily obstruction is still the child with depressed conscious compress the airway. The collapse of the laryngeal There are anatomical, level who is not positioned properly or whose airway inlet during inspiration is a feature of laryngomalacia physiological and is not opened adequately by Basic Life Support and the collapse of the trachea and/or bronchi during developmental reasons for manoeuvres. Airway foreign bodies are also common expiration occurs in tracheo-bronchomalacia. If the children to be particularly and may need rapid intervention. The pattern of intrathoracic airways are narrowed from whatever susceptible to airway obstruction. infective causes of airway obstruction has changed cause, the extra work of inspiration and of expiration since the introduction of vaccination programmes leads to large swings in intrathoracic pressure and the Rapid clinical assessment, against Haemophilus influenzae type B. -
Introduction to the Respiratory System
C h a p t e r 15 The Respiratory System PowerPoint® Lecture Slides prepared by Jason LaPres Lone Star College - North Harris Copyright © 2010 Pearson Education, Inc. Copyright © 2010 Pearson Education, Inc. Introduction to the Respiratory System • The Respiratory System – Cells produce energy: • For maintenance, growth, defense, and division • Through mechanisms that use oxygen and produce carbon dioxide Copyright © 2010 Pearson Education, Inc. Introduction to the Respiratory System • Oxygen – Is obtained from the air by diffusion across delicate exchange surfaces of the lungs – Is carried to cells by the cardiovascular system, which also returns carbon dioxide to the lungs Copyright © 2010 Pearson Education, Inc. 15-1 The respiratory system, composed of conducting and respiratory portions, has several basic functions Copyright © 2010 Pearson Education, Inc. Functions of the Respiratory System • Provides extensive gas exchange surface area between air and circulating blood • Moves air to and from exchange surfaces of lungs • Protects respiratory surfaces from outside environment • Produces sounds • Participates in olfactory sense Copyright © 2010 Pearson Education, Inc. Components of the Respiratory System • The Respiratory Tract – Consists of a conducting portion • From nasal cavity to terminal bronchioles – Consists of a respiratory portion • The respiratory bronchioles and alveoli The Respiratory Tract Copyright © 2010 Pearson Education, Inc. Components of the Respiratory System • Alveoli – Are air-filled pockets within the lungs: -

4 Lower Respiratory Disease
d:/postscript/04-CHAP4_4.3D – 27/1/4 – 9:27 [This page: 245] 4 Lower Respiratory Disease S Walters and DJ Ward 1 Executive summary Statement of the problem Respiratory disease has a substantial impact on the health of populations at all ages and every level of morbidity. Acute upper respiratory infections are the commonest illnesses experienced by individuals throughout life, accounting for over 27% of all GP consultations. Asthma and chronic obstructive pulmonary disease are the cause of almost 5% of all admissions and bed-days, and lower respiratory infections are responsible for almost 11% of deaths. While still uncommon, TB rates appear to be rising and it remains an important problem in some communities. Cystic fibrosis is the commonest inherited disorder in the UK and is an important cause of death in young adults. Improvements in survival mean increasing use of expensive medications and medical technologies. Sub-categories The principal sub-categories of lower respiratory disease considered in this review were chosen on the basis of their public health or health service impact, and are: 1 lower respiratory infections in children 2 lower respiratory infections in adults, including pneumonia 3 asthma 4 chronic obstructive pulmonary disease (COPD) 5 tuberculosis 6 cystic fibrosis. Upper respiratory conditions (including allergic rhinitis), influenza, lung cancer, neonatal respiratory problems, occupational diseases, sleep-disordered breathing, diffuse parenchymal lung disease (a wide range of conditions that include fibrosing alveolitis and sarcoidosis) and other respiratory disorders are not specifically reviewed in detail in this revision. Together, these conditions account for 7% of deaths and 2.5% of hospital admissions, and form a substantial part of the workload of respiratory physicians. -

Common Pediatric Pulmonary Issues
Common Pediatric Pulmonary Issues Chris Woleben MD, FAAP Associate Dean, Student Affairs VCU School of Medicine Assistant Professor, Emergency Medicine and Pediatrics Objectives • Learn common causes of upper and lower airway disease in the pediatric population • Learn basic management skills for common pediatric pulmonary problems Upper Airway Disease • Extrathoracic structures • Pharynx, larynx, trachea • Stridor • Externally audible sound produced by turbulent flow through narrowed airway • Signifies partial airway obstruction • May be acute or chronic Remember Physics? Poiseuille’s Law Acute Stridor • Febrile • Laryngotracheitis (croup) • Retropharyngeal abscess • Epiglottitis • Bacterial tracheitis • Afebrile • Foreign body • Caustic or thermal airway injury • Angioedema Croup - Epidemiology • Usually 6 to 36 months old • Males > Females (3:2) • Fall / Winter predilection • Common causes: • Parainfluenza • RSV • Adenovirus • Influenza Croup - Pathophysiology • Begins with URI symptoms and fever • Infection spreads from nasopharynx to larynx and trachea • Subglottic mucosal swelling and secretions lead to narrowed airway • Development of barky, “seal-like” cough with inspiratory stridor • Symptoms worse at night Croup - Management • Keep child as calm as possible, usually sitting in parent’s lap • Humidified saline via nebulizer • Steroids (Dexamethasone 0.6 mg/kg) • Oral and IM route both acceptable • Racemic Epinephrine • <10kg: 0.25 mg via nebulizer • >10kg: 0.5 mg via nebulizer Croup – Management • Must observe for 4 hours after