Configuration of the Four Parasympathetic Ganglia of the Head
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Perioral Gustatory Sweating: Case Report
The Journal of Laryngology & Otology (2012), 126, 532–534. CLINICAL RECORD © JLO (1984) Limited, 2012 doi:10.1017/S0022215112000229 Perioral gustatory sweating: case report S C KÄYSER1, K J A O INGELS2, F J A VAN DEN HOOGEN2 1Department of Primary and Community Care, Radboud University Nijmegen Medical Centre, and 2Department of Otorhinolaryngology/Head and Neck Surgery, Radboud University Nijmegen Medical Centre, The Netherlands Abstract Objective: Presentation of a case of perioral Frey syndrome. Design: Case report. Subject: A 72-year-old woman with hyperhidrosis around the mouth and chin. Results: This patient suffered from bilateral perioral gustatory sweating following a mandibular osteotomy; such a case has not previously been described. Possible pathophysiological hypotheses are discussed in relation to the anatomy and innervation of the salivary glands. Conclusion: Perioral gustatory sweating is a rare complication of osteotomy. Key words: Gustatory sweating; Frey Syndrome; Perioral; Hyperhidrosis Introduction perioral excessive sweating and flushing which only Frey syndrome, also known as auriculotemporal syndrome, is a occurred during (and not preceding) eating. Her complaints well-known complication of parotid surgery. Approximately had begun following bilateral osteotomy of the mandible in 24 per cent of patients undergoing parotidectomy experience 1960, at the age of 25 years. The indication for this procedure gustatory sweating, although the reported incidence varies had been prognathism. Her recovery had been complicated greatly.1 Frey syndrome appears following a latency period by inadequate bone healing and loss of the right and left of one to 36 months (or longer) after surgery.2,3 inferior alveolar nerves (Figure 1). The aetiology of Frey syndrome is explained by ‘aberrant The diagnosis of hyperhidrosis was made using the nervous regeneration’. -
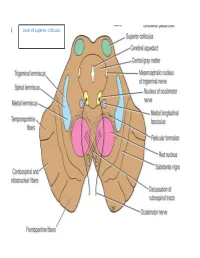
Level of Superior Colliculus ° Edinger- Westphal Nucleus ° Pretectal Nucleus: Close to the Lateral Part of the Superior Colliculus
Level of superior colliculus ° Edinger- Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. Red nucleus • Rounded mass of gray matter • Situated bt cerebral aqueduct and substantia nigra • Reddish blue(vascularity & iron containing pigment) • Afferents from: cerebral cortex,cerebellum,substa ntia nigra, thalamic nuclei, spinal cord • Efferent to: spinal cord, reticular formation. thalamus and substantia nigra • involved in motor coordination. Crus cerebri • Corticospinal & corticonuclear fibers (middle) • Frontopontine fibers (medial) • Temporopontine fibers (lateral) these descending tracts connect the cerebral cortex with spinal cord, cranial nerves nuclei, pons & cerebellum Level at superior colliculus ° Superior colliculus ° Occulomotor nucleus (posterior to MLF) ° Occulomotor n emerges through red nucleus ° Edinger-Westphal nucleus ° pretectal nucleus: close to the lateral part of the superior colliculus. ° MLF ° Medial , trigeminal, spinal leminiscus ( no lateral leminiscus) ° Red nucleus ° Substantia nigra ° Crus cerebri ° RF Substantia nigra ° Large motor nucleus ° is a brain structure located in the midbrain ° plays an important role in reward, addiction, and movement. ° Substantia nigra is Latin for "black substance" due to high levels of melanin ° has connections with basal ganglia ,cerebral cortex ° Concerned with muscle tone ° Parkinson's disease is caused by the death of neurons in the substantia nigra Oculomotor Nerve (III) • Main oculomotor nucleus • Accessory parasympathetic nucleus -

Cranial Nerves 9Th & 10Th
Cranial Nerves 9th & 10th Neuroanatomy block-Anatomy-Lecture 8 Editing file Objectives At the end of the lecture, students should be able to: ● Define the deep origin of both Glossopharyngeal and Vagus Nerves. ● Locate the exit of each nerve from the brain stem. ● Describe the course and distribution of each nerve . ● List the branches of both nerves. Color guide ● Only in boys slides in Green ● Only in girls slides in Purple ● important in Red ● Notes in Grey Glossopharyngeal (IX) 9th Cranial Nerve ● it's mixed nerve, a Sensory nerve with preganglionic parasympathetic and few motor fibers ● It has no real nucleus to itself. Instead it shares nuclei with VII (facial) and X (vagus). Superficial attachment Course ● It arises from the ventral aspect of the 1. It Passes forwards between medulla by a linear series of small Internal jugular vein and rootlets, in groove between olive and External carotid artery. inferior cerebellar peduncle. ● It leaves the cranial cavity by passing 2. Lies Deep to Styloid process. through the jugular foramen in company with the Vagus , and the Accessory 3. Passes between external and nerves and the Internal jugular vein. internal carotid arteries at the posterior border of Stylopharyngeus then lateral to it. 4. It reaches the pharynx by passing between middle and inferior constrictors, deep to Hyoglossus, where it breaks into terminal branches. 3 Glossopharyngeal (IX) 9th Cranial Nerve Ganglia & Communications ● Small with no branches. Superior Ganglion ● It is connected to the Superior Cervical sympathetic ganglion. ● Large and carries general sensations from pharynx, soft palate and tonsil. Inferior ● ganglion It is connected to Auricular Branch of Vagus. -

Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: a Case Report
E CASE REPORT Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: A Case Report Shikha Sharma, MD, PhD,* Wilson Ly, MD, PharmD,* and Xiaobing Yu, MD*† Endoscopic nasal septoplasty is a commonly performed otolaryngology procedure, not known to cause persistent postsurgical pain or hypersensitivity. Here, we discuss a unique case of persis- tent nasal pain that developed after a primary endoscopic septoplasty, which then progressed to marked mechanical and thermal allodynia following a revision septoplasty. Pain symptoms were found to be mediated by the maxillary division of the trigeminal nerve and resolved after percuta- neous radiofrequency ablation (RFA) of bilateral maxillary nerves. To the best of our knowledge, this is the first report of maxillary nerve–mediated nasal allodynia after septoplasty. (A&A Practice. 2020;14:e01356.) GLOSSARY CT = computed tomography; FR = foramen rotundum; HIPAA = Health Insurance Portability and Accountability Act; ION = infraorbital nerve; LPP = lateral pterygoid plate; MRI = magnetic reso- nance imaging; RFA = radiofrequency ablation; SPG = sphenopalatine ganglion; US = ultrasound ndoscopic nasal septoplasty is a common otolaryn- septoplasty for chronic nasal obstruction with resection of gology procedure with rare incidence of postsurgical the cartilage inferiorly and posteriorly in 2010. Before this Ecomplications. Minor complications include epistaxis, surgery, the patient only occasionally experienced mild septal hematoma, septal perforation, cerebrospinal fluid leak, headaches. However, his postoperative course was compli- and persistent obstruction.1 Numbness or hypoesthesia of the cated by significant pain requiring high-dose opioids. After anterior palate, secondary to injury to the nasopalatine nerve, discharge, patient continued to have persistent deep, “ach- has been reported, but is usually rare and temporary, resolv- ing” nasal pain which radiated toward bilateral forehead ing over weeks to months.2 Acute postoperative pain is also and incisors. -

Endocrine Block اللهم ال سهل اال ما جعلته سهل و أنت جتعل احلزن اذا شئت سهل
OSPE ENDOCRINE BLOCK اللهم ﻻ سهل اﻻ ما جعلته سهل و أنت جتعل احلزن اذا شئت سهل Important Points 1. Don’t forget to mention right and left. 2. Read the questions carefully. 3. Make sure your write the FULL name of the structures with the correct spelling. Example: IVC ✕ Inferior Vena Cava ✓ Aorta ✕ Abdominal aorta ✓ 4. There is NO guarantee whether or not the exam will go out of this file. ممكن يأشرون على أجزاء مو معلمه فراح نحط بيانات إضافية حاولوا تمرون عليها كلها Good luck! Pituitary gland Identify: 1. Anterior and posterior clinoidal process of sella turcica. 2. Hypophyseal fossa (sella turcica) Theory • The pituitary gland is located in middle cranial fossa and protected in sella turcica (hypophyseal fossa) of body of sphenoid. Relations Of Pituitary Gland hypothalamus Identify: 1. Mamillary body (posteriorly) 2. Optic chiasma (anteriorly) 3. Sphenoidal air sinuses (inferior) 4. Body of sphenoid 5. Pituitary gland Theory • If pituitary gland became enlarged (e.g adenoma) it will cause pressure on optic chiasma and lead to bilateral temporal eye field blindness (bilateral hemianopia) Relations Of Pituitary Gland Important! Identify: 1. Pituitary gland. 2. Diaphragma sellae (superior) 3. Sphenoidal air sinuses (inferior) 4. Cavernous sinuses (lateral) 5. Abducent nerve 6. Oculomotor nerve 7. Trochlear nerve 8. Ophthalmic nerve 9. Trigeminal (Maxillary) nerve Structures of lateral wall 10. Internal carotid artery Note: Ophthalmic and maxillary are both branches of the trigeminal nerve Divisions of Pituitary Gland Identify: 1. Anterior lobe (Adenohypophysis) 2. Optic chiasma 3. Infundibulum 4. Posterior lobe (Neurohypophysis) Theory Anterior Lobe Posterior Lobe • Adenohypophysis • Neurohypophysis • Secretes hormones • Stores hormones • Vascular connection to • Neural connection to hypothalamus by hypothalamus by Subdivisions hypophyseal portal hypothalamo-hypophyseal system (from superior tract from supraoptic and hypophyseal artery) paraventricular nuclei. -

Gross and Micro-Anatomical Study of the Cavernous Segment of the Abducens Nerve and Its Relationships to Internal Carotid Plexus: Application to Skull Base Surgery
brain sciences Article Gross and Micro-Anatomical Study of the Cavernous Segment of the Abducens Nerve and Its Relationships to Internal Carotid Plexus: Application to Skull Base Surgery Grzegorz Wysiadecki 1,* , Maciej Radek 2 , R. Shane Tubbs 3,4,5,6,7 , Joe Iwanaga 3,5,8 , Jerzy Walocha 9 , Piotr Brzezi ´nski 10 and Michał Polguj 1 1 Department of Normal and Clinical Anatomy, Chair of Anatomy and Histology, Medical University of Lodz, ul. Zeligowskiego˙ 7/9, 90-752 Łód´z,Poland; [email protected] 2 Department of Neurosurgery, Spine and Peripheral Nerve Surgery, Medical University of Lodz, University Hospital WAM-CSW, 90-549 Łód´z,Poland; [email protected] 3 Department of Neurosurgery, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA 70112, USA; [email protected] (R.S.T.); [email protected] (J.I.) 4 Department of Neurosurgery and Ochsner Neuroscience Institute, Ochsner Health System, New Orleans, LA 70433, USA 5 Department of Neurology, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA 70112, USA 6 Department of Anatomical Sciences, St. George’s University, Grenada FZ 818, West Indies 7 Department of Surgery, Tulane University School of Medicine, New Orleans, LA 70112, USA 8 Department of Anatomy, Kurume University School of Medicine, 67 Asahi-machi, Kurume, Fukuoka 830-0011, Japan Citation: Wysiadecki, G.; Radek, M.; 9 Department of Anatomy, Jagiellonian University Medical College, 33-332 Kraków, Poland; Tubbs, R.S.; Iwanaga, J.; Walocha, J.; [email protected] Brzezi´nski,P.; Polguj, M. -

The Sympathetic and the Parasympathetic Nervous System
The sympathetic and the parasympathetic nervous system Zsuzsanna Tóth, PhD Institute of Anatomy, Histology and Embryology Semmelweis University The role of the autonomic nervous system Claude Bernard • „milieu intérieur” concept; every organism lives in its internal environment that is constant and independent form the external environment Walter Bradford Cannon homeostasis; • an extension of the “milieu interieur” concept • consistence in an open system requires mechanisms that act to maintain that consistency • steady-state conditions require that any tendency toward change automatically meets with factors that resist that change • regulating systems that determine the homeostatic state : o autonomic nervous system ( sympathetic, parasympathetic, enteral) o endocrine system General structure of the autonomic nervous system craniosacral thoracolumbar Anatomy Neurotransmittersof the gut autonomic nervous system. symp. gangl pregangl. fiber pregangl. postgangl. fiber fiber (PoR) PoR enteral ganglion PoR PoR smooth muscle smooth muscle Kuratani S Development 2009;136:1585-1589 Sympathetic activation: Fight or flight reaction • energy mobilization • preparation for escape, or fight vasoconstriction • generalized Parasympathetic activation: adrenal • energy saving and restoring • „rest and digest” system • more localized vasoconstriction Paravertebral ganglia and the sympathetic chains pars cervicalis superius ganglion medium cervicale stellatum pars vertebrae • from the base of the skull to the caudal end thoracalis thoracalis of the sacrum • paravertebral ganglia (ganglia trunci sympathici) • rami interganglionares pars vertebrae • the two chains fuses at the ganglion impar abdominalis lumbalis sacrum pars pelvina foramen sacralia anteriora ganglion impar Anatomy of the cervical part of the sympathetic trunk superior cervical ganglion • behind the seath of the carotid, fusiform ggl. cervicale superius • IML T1-3 vegetative motoneurons- preganglionic fibers truncus symp. -

Neurophysiological Aspects of the Trigeminal Sensory System: an Update
Rev. Neurosci. 2018; 29(2): 115–123 Frederic Van der Cruyssen* and Constantinus Politis Neurophysiological aspects of the trigeminal sensory system: an update https://doi.org/10.1515/revneuro-2017-0044 Keywords: infraorbital; mandibular; neurophysiology; Received June 21, 2017; accepted July 20, 2017; previously published ophthalmic nerve; oral somatosensory functioning; online November 8, 2017 trigeminal sensory system. Abstract: The trigeminal system is one of the most complex cranial nerve systems of the human body. Research on it has vastly grown in recent years and concentrated more and more on molecular mechanisms and pathophysiology, Introduction but thorough reviews on this topic are lacking, certainly Knowledge about physiological aspects of the trigeminal on the normal physiology of the trigeminal sensory system. system today is largely based on animal models (Akerman Here we review the current literature on neurophysiology and Goadsby, 2015; Herta et al., 2017), cadaver studies of the trigeminal nerve from peripheral receptors up to its (Ezure et al., 2001; Williams et al., 2003) or extrapola- central projections toward the somatosensory cortex. We tions from peripheral nerve functioning. Human studies focus on the most recent scientific discoveries and describe are frequently limited to pathophysiology and lack proper historical relevant research to substantiate further. One study designs (Tanaka and Zhao, 2016; Goadsby et al., chapter on new insights of the pathophysiology of pain 2017). Neurophysiological research in this area is difficult at the level of the trigeminal system is added. A database due to the invasive character of most neurophysiological search of Medline, Embase and Cochrane was conducted tests, the small caliber of fibers, high density of receptors, with the search terms ‘animal study’, ‘neurophysiology’, cross-connections between different cranial nerves, dif- ‘trigeminal’, ‘oral’ and ‘sensory’. -

Simple Ways to Dissect Ciliary Ganglion for Orbital Anatomical Education
OkajimasDetection Folia Anat. of ciliary Jpn., ganglion94(3): 119–124, for orbit November, anatomy 2017119 Simple ways to dissect ciliary ganglion for orbital anatomical education By Ming ZHOU, Ryoji SUZUKI, Hideo AKASHI, Akimitsu ISHIZAWA, Yoshinori KANATSU, Kodai FUNAKOSHI, Hiroshi ABE Department of Anatomy, Akita University Graduate School of Medicine, Akita, 010-8543 Japan –Received for Publication, September 21, 2017– Key Words: ciliary ganglion, orbit, human anatomy, anatomical education Summary: In the case of anatomical dissection as part of medical education, it is difficult for medical students to find the ciliary ganglion (CG) since it is small and located deeply in the orbit between the optic nerve and the lateral rectus muscle and embedded in the orbital fat. Here, we would like to introduce simple ways to find the CG by 1): tracing the sensory and parasympathetic roots to find the CG from the superior direction above the orbit, 2): transecting and retracting the lateral rectus muscle to visualize the CG from the lateral direction of the orbit, and 3): taking out whole orbital structures first and dissecting to observe the CG. The advantages and disadvantages of these methods are discussed from the standpoint of decreased laboratory time and students as beginners at orbital anatomy. Introduction dissection course for the first time and with limited time. In addition, there are few clear pictures in anatomical The ciliary ganglion (CG) is one of the four para- textbooks showing the morphology of the CG. There are sympathetic ganglia in the head and neck region located some scientific articles concerning how to visualize the behind the eyeball between the optic nerve and the lateral CG, but they are mostly based on the clinical approaches rectus muscle in the apex of the orbit (Siessere et al., rather than based on the anatomical procedure for medical 2008). -

The Mandibular Nerve - Vc Or VIII by Prof
The Mandibular Nerve - Vc or VIII by Prof. Dr. Imran Qureshi The Mandibular nerve is the third and largest division of the trigeminal nerve. It is a mixed nerve. Its sensory root emerges from the posterior region of the semilunar ganglion and is joined by the motor root of the trigeminal nerve. These two nerve bundles leave the cranial cavity through the foramen ovale and unite immediately to form the trunk of the mixed mandibular nerve that passes into the infratemporal fossa. Here, it runs anterior to the middle meningeal artery and is sandwiched between the superior head of the lateral pterygoid and tensor veli palatini muscles. After a short course during which a meningeal branch to the dura mater, and the nerve to part of the medial pterygoid muscle (and the tensor tympani and tensor veli palatini muscles) are given off, the mandibular trunk divides into a smaller anterior and a larger posterior division. The anterior division receives most of the fibres from the motor root and distributes them to the other muscles of mastication i.e. the lateral pterygoid, medial pterygoid, temporalis and masseter muscles. The nerve to masseter and two deep temporal nerves (anterior and posterior) pass laterally above the medial pterygoid. The nerve to the masseter continues outward through the mandibular notch, while the deep temporal nerves turn upward deep to temporalis for its supply. The sensory fibres that it receives are distributed as the buccal nerve. The 1 | P a g e buccal nerve passes between the medial and lateral pterygoids and passes downward and forward to emerge from under cover of the masseter with the buccal artery. -

An Unusual Finding of the Auriculotemporal Nerve: Possible Risk Factor During Preauricular Skin Incisions
Case Report An unusual finding of the auriculotemporal nerve: possible risk factor during preauricular skin incisions Joe Iwanaga1,2,3, Samuel L. Bobek4, Christian Fisahn1,5, Ken Nakamura3, Yoshihiro Miyazono3, R. Shane Tubbs1 1Seattle Science Foundation, Seattle, WA 98122, USA; 2Department of Anatomy, 3Dental and Oral Medical Center, Kurume University School of Medicine, Kurume, Fukuoka 830-0011, Japan; 4Swedish Maxillofacial Surgery, 5Swedish Neuroscience Institute, Swedish Medical Center, Seattle, WA 98122, USA Correspondence to: Joe Iwanaga. Seattle Science Foundation, 550 17th Ave, James Tower, Suite 600, Seattle, WA 98122, USA. Email: [email protected]. Abstract: The auriculotemporal nerve (ATN) is a branch of the mandibular nerve and has been implicated for some migraines and its role in Frey’s syndrome is well known. An adult cadaver was found to have a duplicated ATN. The anterior trunk ascended as the superficial temporal artery and gave off the branches to the temporomandibular joint, parotid gland, external acoustic meatus and temporal region and communicated with a posterior trunk of the ATN. The posterior trunk ascended via the subcutaneous tissues 1 mm anterior to the auricle and gave off the branches to the anterior auricular region, temporal region and communicated with the anterior trunk. Such a duplicated ATN might be injured with preauricular skin incisions. Knowledge of such an anatomical variation might assist surgeons in iatrogenic injury of the ATN. Keywords: Auriculotemporal nerve (ATN); infratemporal fossa; Frey’s syndrome; mandibular nerve Submitted Aug 09, 2016. Accepted for publication Aug 17, 2016. doi: 10.21037/gs.2016.09.02 View this article at: http://dx.doi.org/10.21037/gs.2016.09.02 Introduction Case presentation The auriculotemporal nerve (ATN) is one of the branches During the dissection of a cadaver that was 87-year-old at of the mandibular division (V3) of the trigeminal nerve. -

Neuronal Types and Their Specification Dynamics in the Autonomic Nervous System
From the Department of Medical Biochemistry and Biophysics Karolinska Institutet, Stockholm, Sweden NEURONAL TYPES AND THEIR SPECIFICATION DYNAMICS IN THE AUTONOMIC NERVOUS SYSTEM Alessandro Furlan Stockholm 2016 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. Printed by E-Print AB © Alessandro Furlan, 2016 ISBN 978-91-7676-419-0 On the cover: abstract illustration of sympathetic neurons extending their axons Credits: Gioele La Manno NEURONAL TYPES AND THEIR SPECIFICATION DYNAMICS IN THE AUTONOMIC NERVOUS SYSTEM THESIS FOR DOCTORAL DEGREE (Ph.D.) By Alessandro Furlan Principal Supervisor: Opponent: Prof. Patrik Ernfors Prof. Hermann Rohrer Karolinska Institutet Max Planck Institute for Brain Research Department of Medical Biochemistry and Research Group Developmental Neurobiology Biophysics Division of Molecular Neurobiology Examination Board: Prof. Jonas Muhr Co-supervisor(s): Karolinska Institutet Prof. Ola Hermansson Department of Cell and Molecular Biology Karolinska Institutet Department of Neuroscience Prof. Tomas Hökfelt Karolinska Institutet Assistant Prof. Francois Lallemend Department of Neuroscience Karolinska Institutet Division of Chemical Neurotransmission Department of Neuroscience Prof. Ted Ebedal Uppsala University Department of Neuroscience Division of Developmental Neuroscience To my parents ABSTRACT The autonomic nervous system is formed by a sympathetic and a parasympathetic division that have complementary roles in the maintenance of body homeostasis. Autonomic neurons, also known as visceral motor neurons, are tonically active and innervate virtually every organ in our body. For instance, cardiac outflow, thermoregulation and even the focusing of our eyes are just some of the plethora of physiological functions under the control of this system. Consequently, perturbation of autonomic nervous system activity can lead to a broad spectrum of disorders collectively known as dysautonomia and other diseases such as hypertension.