DEPARTMENT of MEDICINE 2016 Annual Report DIVISIONS and INSTITUTES
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ASM Journals Eliminate Impact Factor Information from Journal Websites
ASM Journals Eliminate Impact Factor Information from Journal Websites The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Casadevall, A., S. Bertuzzi, M. J. Buchmeier, R. J. Davis, H. Drake, F. C. Fang, J. Gilbert, et al. 2016. “ASM Journals Eliminate Impact Factor Information from Journal Websites.” mSphere 1 (4): e00184-16. doi:10.1128/mSphere.00184-16. http:// dx.doi.org/10.1128/mSphere.00184-16. Published Version doi:10.1128/mSphere.00184-16 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:27822275 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA EDITORIAL crossmark ASM Journals Eliminate Impact Factor Information from Journal Websites Arturo Casadevall,a Editor in Chief, mBio®, Stefano Bertuzzi,b Chief Executive Officer, ASM, Michael J. Buchmeier,c Editor in Chief, Microbiology and Molecular Biology Reviews®, Roger J. Davis,d Editor in Chief, Molecular and Cellular Biology®, Harold Drake,e Editor in Chief, Applied and Environmental Microbiology®, Ferric C. Fang,f Editor in Chief, Infection and Immunity®, Jack Gilbert,g Editor in Chief, mSystems™, Barbara M. Goldman,b Director, Journals, ASM, Michael J. Imperiale,h Editor in Chief, mSphere™, Philip Matsumura,i Editor, Genome Announcements™, Alexander J. McAdam,j Editor in Chief, Journal of Clinical Microbiology®, Marcela F. Pasetti,k Editor in Chief, Clinical and Vaccine Immunology®, Rozanne M. -

ELEITORES DE EUA-MIAMI Nome Do Eleitor Seção Eleitoral AARON
ELEIÇÕES 2014 - ELEITORES DE EUA-MIAMI Nome do eleitor Seção Eleitoral AARON JOSHUA ODEN 214 AARON NIKOLAOS LALINDE 845 AARON PLUDWINSK 846 ABAS HASSAN HIJAZI 792 ABDIAS AVELINO DE AZEVÊDO NETO 822 ABEL COLOSSI NETO 842 ABEL EVARISTO BESSA ALVES 913 ABERALDO TEIXEIRA DE SOUZA 998 ABGAIL CAMPOY THIEME 845 ABIGAIL FRANCELINO LUCIANO GENÉZIO 826 ABIGAIL PATRICIA DE ARAUJO 791 ABIGAIL PIRES ROELLES 213 ABILIO DE AZEVEDO CERQUEIRA 229 ABILIO DE OLIVEIRA 226 ABILIO DE SOUZA NETO 212 ABILIO VIEIRA LOPES NETO 214 ABINOAM MODESTO DA SILVA 826 ABIQUEILA ALVES MARCELINO PAIVA 906 ABNEDER NACIFF DE CASTRO 846 ABNER ALVES DE ALMEIDA 214 ABNER DAVID WILDING 730 ABNER OLIVEIRA DE MOURA E SILVA 826 ABNNER GABRIEL SANTOS AGRA DE ARAUJO 809 ABRAAO DE OLIVEIRA VAZ 934 ABRAÃO MELO FERREIRA COSTA 809 ABRAHAM BENMERGUI 226 ABRAHAM COPERNIK BITTERMAN 229 ABRAHAM MICHAL FRYDMAN 214 ABRAHAO MECLER 210 ACACIO ALVES PEREIRA FILHO 232 ACACIO RAFAEL VILLANI 842 ACASSIA FERREIRA DA CUNHA 217 ACELINA MARIA COSTA MOREIRA 224 ACHZA SANTIAGO RODRIGUES 210 ACILCE TEREZINHA HORST 846 ACIZIO CORREA EVANGELISTA 934 ACYR BORGES JUNIOR 228 ADAILSON BORGES PERPETUO 846 ADAILSON PEREIRA MOURA 826 ADAILTON RODRIGUES 217 ADALBERTO BEDRAN 998 ADALBERTO BONALDO 845 ADALBERTO CANDIDO DE ALBUQUERQUE 601 ADALBERTO GONÇALVES SILVA 604 ADALBERTO JOSÉ DA SILVA 822 ADALBERTO ROMUALDO PEREIRA 847 ADALBERTO SCALIANTE 792 ADALBERTO SILVA FILHO 998 ADALBERTO TORRES 229 ADALGISA BARISON 213 ADALTO JOSE LOPES 227 ADALTO RODRIGUES PEREIRA 785 ADALTO SILVA CORREIA FILHO 934 ADALTON MARQUES DA SILVA -

Holmes Washington 0250E 22
©Copyright 2020 Daniel Holmes Identification of Targetable Vulnerabilities During Latent KSHV Infection Daniel Holmes A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2020 Reading Committee: Michael Lagunoff, Chair Adam Philip Geballe Jason G Smith Program Authorized to Offer Degree: Department of Microbiology University of Washington Abstract Identification of Targetable Vulnerabilities During Latent KSHV Infection Daniel Holmes Chair of the Supervisory Committee: Professor Michael Lagunoff Department of Microbiology Viruses are defined as obligate intracellular parasites that require host processes to repli- cate. Latent virus life cycles are no exception to this definition, as viruses are still reliant on host machinery for continued proliferation and maintenance of viral genomes, even in the absence of lytic replication. In this thesis, I used essentiality screening to identify host factors on which Kaposi's Sarcoma Associated Herpesvirus (KSHV) relies for the proliferation and survival of latently infected cells. KSHV is the etiological agent of Kaposi's Sarcoma (KS), an endothelial cell-based tumor where more than 90% of the endothelial cells in the tumor are latently infected with KSHV. While traditional therapies for herpesviruses target lytic replication, the prevalence of latency in KS necessitates exploration of options for intervening in this stage of the viral life cycle. I performed CRISPR/Cas9 screening using lentiviral vec- tors encoding a library of single guide RNAs (sgRNAs) targeting every protein coding gene in the human genome. I compared mock infected and KSHV infected endothelial cells eight days post infection to identify genes essential to latent KSHV infection. -
Help Make a Difference Every Day for Those We Serve
You help make a difference every day for those we serve. 2010 HONOR ROLL OF DONORS Philanthropic Facelift Benefits Patient, Family Experience Philanthropy was critically important to In addition, all of the Hospital’s public entrances transforming the face of Hartford Hospital in and its main cafeteria were renovated to provide 2010. The support of many generous donors a warm and welcoming décor for patients provided an essential boost to the first year of and families. Other major changes included HH2020, the Hospital’s 10-year modernization significant updates to the infrastructure of the plan. Their generosity helped: Conklin Building and the renovation of Heublein Add 8 ICU rooms and 9 step-down Hall in the Education and Resource Center (ERC). rooms on Bliss 9 and Bliss 11. A remarkably generous gift from a Farmington Expand the Emergency Department’s couple made possible the refurbishment of capacity by 10%, adding 5 front-end the entranceway and lobby of the ERC and an provider rooms, an additional exam adjacent conference room. (See story, page 23). room, 4 new triage desks and a new In all, with the help of charitable gifts, the discharge area – in the first phase Hospital renovated some 200,000 square feet of of the expansion plan for this vital area. space in the first year of HH2020. Create a new 26-bed inpatient unit for the Helen & Harry Gray Cancer Center on CB2. Establish the Center for Education, Simulation and Innovation for training tomorrow’s physicians today. We are pleased to have this opportunity to express the Our Honor Roll of Donors each year celebrates the appreciation of the Administration and the Board of tireless efforts of many dedicated volunteers and the Directors to our community of advocates, volunteers enormous generosity of our community. -

Editors' Statement on Considerations of Biodefence and Biosecurity
EDITORIAL Editors’ statement on considerations of biodefence and biosecurity The threat of bioterrorism requires active consideration by scientists. On 9 January 2003, the US National Academy of Sciences held a discussion on the balance between scientific openness and security. The next day, a group of editors met to discuss the issues with specific reference to the scientific publication process. The following statement has emerged from that meeting. The principles dis- cussed will be considered and followed through by Nature Medicine The process of scientific publication, is a view, shared by nearly all, that there is FOURTH: We recognize that on occasions through which new findings are reviewed information that, although we cannot an editor may conclude that the potential for quality and then presented to the rest now capture it with lists or definitions, harm of publication outweighs the poten- of the scientific community and the pub- presents enough risk of use by terrorists tial societal benefits. Under such circum- lic, is a vital element in our national life. that it should not be published. How and stances, the paper should be modified, or New discoveries reported in research pa- by what processes it might be identified not be published. Scientific information is pers have helped improve the human con- will continue to challenge us, because – as also communicated by other means: semi- dition in myriad ways: protecting public all present acknowledged — it is also true nars, meetings, electronic posting, etc. health, multiplying agricultural yields, that open publication brings benefits not Journals and scientific societies can play fostering technological development and only to public health but also in efforts to an important role in encouraging investi- economic growth, and enhancing global combat terrorism. -
Table of Contents (PDF)
December 30, 2014 u vol. 111 u no. 52 u 18401–18800 Cover image: Pictured are Konik horses, a semiferal breed, at a nature reserve in Oostvaar- dersplassen, Holland. Mikkel Schubert et al. sequenced the DNA from ancient horse bones and compared it to the genomes of five modern domesticated breeds and the only living wild horse species, Przewalski’s horse. Phylogenetic analysis revealed that domesticated breeds likely derived at least partially from the ancient populations. In addition, genes involved in muscle, limb, joint, and cardiac system development, and in social behavior, learning capa- bilities, fear response, and agreeableness were favored during domestication, indicating adaptations that may have resulted from human use and taming. See the article by Schubert et al. on pages E5661–E5669. Image courtesy of Ruben Smit (photographer). From the Cover E5661 Genetics of horse domestication 18460 Dating mastodon extinction 18524 Ethnic diversity and price bubbles 18530 Gulf of Mexico hypoxic zone 18709 Plague bacteria and flea hosts Contents REVIEWER ACKNOWLEDGMENT (ONLINE ONLY) E5724 Acknowledgment of Reviewers, 2014 THIS WEEK IN PNAS SCIENCE AND CULTURE—How science intersects with culture 18401 In This Issue 18403 Science and Culture: Q&A with Roger Malina Maggie McKee LETTERS (ONLINE ONLY) COMMENTARIES E5602 Incorrect representation of Barrier Canyon rock art site’s history and other factors invalidate reported dates Nancy Simon and Richard Reed 18405 The curious case of the Arctic mastodons Duane Froese E5604 Reply to Simon and Reed: Independent and converging See companion article on page 18460 results rule out historic disturbance and confirm age constraints for Barrier Canyon rock art 18407 Downsides of social capital Joel L. -

Uncensored Exchange of Scientific Results
Correction EDITORIAL Correction for “Uncensored exchange of scientific results,” by Journal Editors and Authors Group, which appeared in issue 4, February 18, 2003, of Proc Natl Acad Sci USA (100:1464; first published February 15, 2003; 10.1073/pnas.0630491100). Due to a printer’s error, the author name “Steven Salzburg” should instead appear as “Steven Salzberg.” Additionally, the affiliation for Steven Salzberg should instead appear as “The Institute for Genomic Research.” The corrected group author footnote appears below. The online version has been corrected. *Group members: Ronald Atlas, President, ASM, and Editor, CRC Critical Reviews in Mi- crobiology; Philip Campbell, Editor, Nature; Nicholas R. Cozzarelli, Editor, PNAS; Greg Curfman, Deputy Editor, New England Journal of Medicine; Lynn Enquist, Editor, Journal of Virology; Gerald Fink, Massachusetts Institute of Technology; Annette Flanagin, Man- aging Senior Editor, Journal of the American Medical Association, and President, Council of Science Editors; Jacqueline Fletcher, President, American Phytopathological Society; Elizabeth George, Program Manager, National Nuclear Security Administration, Depart- ment of Energy; Gordon Hammes, Editor, Biochemistry; David Heyman, Senior Fellow and Director of Science and Security Initiatives, Center for Strategic and International Studies; Thomas Inglesby, Editor, Biosecurity and Bioterrorism; Samuel Kaplan, Chair, ASM Pub- lications Board; Donald Kennedy, Editor, Science; Judith Krug, Director, Office for Intel- lectual Freedom, American Library -

20.2 Leader 771
editorials Statement on the consideration of biodefence and biosecurity As discussed in a Commentary by Tony Fauci on page 787, the threat of bioterrorism requires active consideration by scientists. On 9 January 2003, the US National Academy of Sciences held a discussion meeting on the balance between scientific openness and security (see Nature 421, 197; 2003). The next day, a group of editors met to discuss the issues with specific reference to the scientific publication process. The following statement has emerged from that meeting. The statement was conceived in a US context, but the principles discussed will be considered and followed through by Nature and its related journals in their international arenas. he process of scientific publication, through which new find- information, but also recognize that research in the very same ings are reviewed for quality and then presented to the rest fields will be critical to society in meeting the challenges of Tof the scientific community and the public, is a vital element defence. We are committed to dealing responsibly and effectively in our national life. New discoveries reported in research papers with safety and security issues that may be raised by papers have helped improve the human condition in myriad ways: protect- submitted for publication, and to increasing our capacity to ing public health, multiplying agricultural yields, fostering techno- identify such issues as they arise. logical development and economic growth, and enhancing global Third: Scientists and their journals should consider the appropriate stability and security. level and design of processes to accomplish effective review of But new science, as we know, may sometimes have costs as well as papers that raise such security issues. -
2020 Convention Program.Pdf
aseees Association for Slavic, East European, & Eurasian Studies 2020 ASEEES VIRTUAL CONVENTION Nov. 5-8 • Nov. 14-15 ASSOCIATION FOR SLAVIC, EAST EUROPEAN, & EURASIAN STUDIES 52nd Annual ASEEES Convention November 5-8 and 14-15, 2020 Convention Theme: Anxiety & Rebellion The 2020 ASEEES Annual Convention will examine the social, cultural, and economic sources of the rising anxiety, examine the concept’s strengths and limitations, reconstruct the politics driving anti- cosmopolitan rebellions and counter-rebellions, and provide a deeper understanding of the discourses and forms of artistic expression that reflect, amplify or stoke sentiments and motivate actions of the people involved. Jan Kubik, President; Rutgers, The State U of New Jersey / U College London 2020 ASEEES Board President 3 CONVENTION SPONSORS ASEEES thanks all of our sponsors whose generous contributions and support help to promote the continued growth and visibility of the Association during our Annual Convention and throughout the year. PLATINUM SPONSORS: Cambridge University Press GOLD SPONSOR: East View information Services SILVER SPONSOR: Indiana University, Robert F. Byrnes Russian and East European Institute BRONZE SPONSORS: Baylor University, Modern Languages and Cultures | Communist and Post-Communist Studies by University of California Press | Open Water RUSSIAN SCHOLAR REGISTRATION SPONSOR: The Carnegie Corporation of New York FILM SCREENING SPONSOR: Arizona State University, The Melikian Center: Russian, Eurasian and East European Studies FRIENDS OF ASEEES: -
2010 Annual Report
Annual Report July 1, 2009 to June 30, 2010 Judge Baker Children’s Center Inspiring Possibilities NEACWCD Manville School JBCC The Baker Clinical Care Mission Statement Judge Baker Children’s Center promotes the best possible mental health of children through the integration of research, intervention, training and advocacy. BOARD OF TRUSTEES MEMBERS OF THE PROGRAM & Kathryn E. Cade CORPORATION DEPARTMENT DIRECTORS Chair Joseph D. Alviani Todd Anderson Edward E. Mullen Walter Angoff Information Technology First Vice Chairman Reginald I. Barron William R. Beardslee, MD Family Preventative Jay L. Webber Ellen R. Cohen Intervention Project Second Vice Chairman & Treasurer Lawrence B. Cohen John S. Driscoll Anthony M. Bono Verne W. Vance, Jr. Finance Clerk Edward A. Dubilo Deborah S. First Elizabeth A. Fitzsimons Deborah L. Anderson Henry Louis Gates, Jr., Ph.D. Development Carol E. Bonner Samuel G. King Janina R. Galler, MD Lisa Dabney Burrows Richard Lewis Legacy of Childhood Malnutrition Thomas W. Cornu Peter C. Nordblom James F. Prince, LICSW Robert P. Gittens Charles Ogletree, Jr. The Manville School Robert G. Holdway Marcia A. Polese Nina Rodriguez Andrew R. Knowland, Jr. Manuel Rosenberg Facilities George Macomber Richard A. Soden Phyllis Rothberg Katie Nicholson Jeffrey S. Stern Teens Achieving Mastery Over John R.A. Pears, RIBA Stress (TEAMS) Richard Weissbourd, Ph.D. Claire S. Stern Colonel Ralph Zimmerman Julie S. Springwater Dorothy A. Weber, Ed.D. New England Association of Child Grace Zimmerman John R. Weisz, Ph.D., ABPP Welfare Commissioners and Directors Rhonda Zinner Lucie E. White Rachel E. Sudikoff George C. Wilson Human Resources EXECUTIVE TEAM Claudio O. -
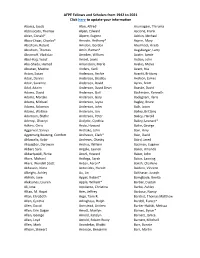
AFPE Fellows and Scholars from 1942 to 2021 Click Here to Update Your
AFPE Fellows and Scholars from 1942 to 2021 Click here to update your information Abarca, Jacob Alon, Alfred Arumugam, Thiruma Abbruscato, Thomas Alpen, Edward Ascione, Frank Abler, Conald* Alpern, Eugene Ashkin, Michael Abou-Chaar, Charles* Amadio, Anthony* Asprin, Mary Abraham, Robert Amidon, Gordon Ateshkadi, Arasb Abraham, Thomas Amin, Raman* Augsburger, Larry Abramoff, Vladislav Amsden, William Austin, Jamie Abul-Hajj, Yusuf Amsel, Lewis Autian, John Abu-Shady, Hamed Amundson, Merle Avalos, Melva Abustan, Maxine Anders, Karli Avant, Nia Acton, Susan Anderson, Archie Avaritt, Brittany Adair, Dennis Anderson, Bradley Axelson, James Adair, Suzanne Anderson, David Ayres, Scott Adal, Adaim Anderson, David Dean Baaske, David Adams, David Anderson, Gail Bachmann, Kenneth Adams, Marijke Anderson, Gary Badagnani, Ilaria Adams, Michael Anderson, Jayna Bagley, Bruce Adams, Solomon Anderson, John Baik, Jason Adams, Wallace Anderson, Jon Bailey, Brittany Adamson, Blythe Anderson, Peter Bailey, Harold Adeniyi, Oluseyi Andjelic, Cynthia Bailey, Leonard* Adkins, Chris Ando, Howard Bailie, George Aggarwal, Saniya Andrako, John Bain, Amy Agyemang Boateng, Comfort Andreson, Clark* Bain, David Ahluwalia, Kabir Andrews, Chasity Baird, Jared Akajagbor, Darowan Andrus, William Baizman, Eugene Akbari, Sara Angelo, Lauren Baker, Amanda Akbariyazidi, Rizita Ansel, Howard Baker, John Akers, Michael Antloga, Sarah Baker, Lanning Akers, Wendell Scott Anton, Aaron* Baksh, Charlene Akhavein, Nima Antonides, Harold Baldino, Vincent Albright, Ashley Ao, Lin Balthasar, -

Maryland Historical Magazine, 1985, Volume 80, Issue No. 3
Maryland Historical Magazine * r. "^ EDMONDSON " -'ir-':-'"- f f iBlMtfiVriiJnBi Published Quarterly by The Museum and Library of Maryland History The Maryland Historical Society Fall 1985 THE MARYLAND HISTORICAL SOCIETY OFFICERS, 1984-1985 J. Fife Symington, Jr., Chairman* Robert G. Merrick, ST., Honorary Chairman Brian B. Topping, President* Mrs. Charles W. Cole, Jr., Vice President* William C. Whitridge, Vice President* E. Phillips Hathaway, Vice President* Richard P. Moran, Secretary* Samuel Hopkins, Vice President* Mrs. Frederick W. Lafferty, Treasurer* Walter D. Pinkard, Sr., Vice President* Leonard C. Crewe, Jr., Past President* Truman T. Semans, Vice President* Bryson L. Cook, Counsel* Frank H. Weller, Jr., Vice President* * The officers listed above constitute the Society's Executive Committee. BOARD OF TRUSTEES, 1984-1985 H. Furlong Baldwin William S. James, Harford Co. Mrs. Emory J. Barber, St. Mary's Co. H. Irvine Keyser II (Honorary) Gary Black, Jr. Richard R. Kline, Frederick Co. John E. Boulais, Caroline Co. Robert G. Merrick, Jr. J. Henry Butta Michael Middleton, Charles Co. Mrs. James Frederick Colwill (Honorary) Jack Moseley Owen Daly II Thomas S. Nichols (Honorary) Donald L. DeVries James L. Olfson, Anne Arundel Co. Leslie B. Disharoon Eleanor A. Owen Deborah B. English Mrs. Brice Phillips, Worcester Co. Jerome Geckle J. Hurst Purnell, Jr., Kent Co. William Gilchrist, Allegany Co. George M. Radcliffe Louis L. Goldstein, Calvert Co. Adrian P. Reed, Queen Anne's Co. Kingdon Gould, Jr., Howard Co. G. Donald Riley, Jr., Carroll Co. William Grant, Garrett Co. Mrs. Timothy Rodgers Benjamin H. Griswold III David Rogers, Wicomico Co. Willard Hackerman John D. Schapiro R.