Challenges Facing Rural and Remote PD Patients in Manitoba
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

May 6–15, 2011 Festival Guide Vancouver Canada
DOCUMENTARY FILM FESTIVAL MAY 6–15, 2011 FESTIVAL GUIDE VANCOUVER CANADA www.doxafestival.ca facebook.com/DOXAfestival @doxafestival PRESENTING PARTNER ORDER TICKETS TODAY [PAGE 5] GET SERIOUSLY CREATIVE Considering a career in Art, Design or Media? At Emily Carr, our degree programs (BFA, BDes, MAA) merge critical theory with studio practice and link you to industry. You’ll gain the knowledge, tools and hands-on experience you need for a dynamic career in the creative sector. Already have a degree, looking to develop your skills or just want to experiment? Join us this summer for short courses and workshops for the public in visual art, design, media and professional development. Between May and August, Continuing Studies will off er over 180 skills-based courses, inspiring exhibits and special events for artists and designers at all levels. Registration opens March 31. SUMMER DESIGN INSTITUTE | June 18-25 SUMMER INSTITUTE FOR TEENS | July 4-29 Table of Contents Tickets and General Festival Info . 5 Special Programs . .15 The Documentary Media Society . 7 Festival Schedule . .42 Acknowledgements . 8 Don’t just stand there — get on the bus! Greetings from our Funders . .10 Essay by John Vaillant . 68. Welcome from DOXA . 11 NO! A Film of Sexual Politics — and Art Essay by Robin Morgan . 78 Awards . 13 Youth Programs . 14 SCREENINGS OPEning NigHT: Louder Than a Bomb . .17 Maria and I . 63. Closing NigHT: Cave of Forgotten Dreams . .21 The Market . .59 A Good Man . 33. My Perestroika . 73 Ahead of Time . 65. The National Parks Project . 31 Amnesty! When They Are All Free . -

Physician Directory
Physician Directory, Currently Practicing in the Province Information is accurate as of: 9/24/2021 8:00:12 AM Page 1 of 97 Name Office Address City Prov Postal Code CCFP Specialty Abara, Chukwuma Solomon Thompson Clinic, 50 Selkirk Avenue Thompson MB R8N 0M7 CCFP Abazid, Nizar Rizk Health Sciences Centre, Section of Neonatology, 665 William Avenue Winnipeg MB R3E 0L8 Abbott, Burton Bjorn Seven Oaks General Hospital, 2300 McPhillips Street Winnipeg MB R2V 3M3 CCFP Abbu, Ganesan Palani C.W. Wiebe Medical Centre, 385 Main Street Winkler MB R6W 1J2 CCFP Abbu, Kavithan Ganesan C.W. Wiebe Medical Centre, 385 Main Street Winkler MB R6W 1J2 CCFP Abdallateef, Yossra Virden Health Centre, 480 King Street, Box 400 Virden MB R0M 2C0 Abdelgadir, Ibrahim Mohamed Ali Manitoba Clinic, 790 Sherbrook Street Winnipeg MB R3A 1M3 Internal Medicine, Gastroenterology Abdelmalek, Abeer Kamal Ghobrial The Pas Clinic, Box 240 The Pas MB R9A 1K4 Abdulrahman, Suleiman Yinka St. Boniface Hospital, Room M5038, 409 Tache Avenue Winnipeg MB R2H 2A6 Psychiatry Abdulrehman, Abdulhamid Suleman 200 Ste. Anne's Road Winnipeg MB R2M 3A1 Abej, Esmail Ahmad Abdullah Winnipeg Clinic, 425 St. Mary Ave Winnipeg MB R3C 0N2 CCFP Gastroenterology, Internal Medicine Abell, Margaret Elaine 134 First Street, Box 70 Wawanesa MB R0K 2G0 Abell, William Robert Rosser Avenue Medical Clinic, 841 Rosser Avenue Brandon MB R7A 0L1 Abidullah, Mohammad Westman Regional Laboratory, Rm 146 L, 150 McTavish Avenue Brandon MB R7A 7H8 Anatomical Pathology Abisheva, Gulniyaz Nurlanbekovna Pine Falls Health Complex, 37 Maple Street, Box 1500 Pine Falls MB R0E 1M0 CCFP Abo Alhayjaa, Sahar C W Wiebe Medical Centre, 385 Main Street Winkler MB R6W 1J2 Obstetrics & Gynecology Abou-Khamis, Rami Ahmad Northern Regional Health, 867 Thompson Drive South Thompson MB R8N 1Z4 Internal Medicine Aboulhoda, Alaa Samir The Pas Clinic, Box 240 The Pas MB R9A 1K4 General Surgery Abrams, Elissa Michele Meadowwood Medical Centre, 1555 St. -

Errata Since Publication in June 2010, We Have Discovered an Number of Items That Needed Either Clarity Or Correction
Metis Health Status and Healthcare Use in Manitoba Errata Since publication in June 2010, we have discovered an number of items that needed either clarity or correction. Updated pages are # 10-11, 56, 141-142, 234-235, 254, 272, 286, 299-301, 456, 460, 480 &582. All the updated pages are attached. Manitoba Centre for Health Policy Errata_Nov_2012.indd 1 28/11/2012 2:04:52 PM Chapter 1: Introduction and Methods This page edited September 23, 2010. Figure 1.4: Villages, Towns, Cities, or Unorganized Territories Where Metis Live in Manitoba, 2009 Where Metis Live in Manitoba, 2009 Villages, towns, cities, or unorganized territories See next page for Metis 1 community locations code key 2 3 6 14 5 4 7 8 11 10 19 15 20 9 21 22 12 16 18 23 24 13 17 2825 27 26 29 30 31 37 32 3433 35 38 36 39 119 42 40 41 43 44 4950 65 51 45 66 58 67 52 68 72 4647 53 69 55 70 54 71 48 73 120 56 57 75 121 62 74 59 76 77 80 60 64 78 79 104 61 63 81 123122 105 82 83 109 124 126 106 84 85 86 108 125 107 89 88 94 90 93 127 110 116 91 87 11792 103 95 98 102 111 96 100 101 115 118 99 97 139 128 112 129 130 132 133 134 113 136 131 135 114 137 138 Source: MCHP/MMF, 2010 10 | University of Manitoba Metis Health Status and Healthcare Use in Manitoba This page edited September 23, 2010. -

Gods Lake Narrows
Gods Lake Narrows Community Overview Statistics Census Year Population History 1985 112 Two communities share the name Gods Lake, 1991 105 the community and the adjacent God’s Lake 1996 101 First Nation reserve. Information relates to the 2001 113 non-reserve side, unless otherwise noted. 2006 88 2011 85 Access 2016 89 The community is located along the lakeshore of *information is from Statistics Canada the narrow portion of Gods Lake 224 kilometres (km) by air southeast of Thompson and 547 km Households by air northeast of Winnipeg. There are 46 housing units. Governance Boundary The community is represented by a mayor and Manitoba Regulation 67/2009 refers to Director council under The Northern Affairs Act. of Surveys at Winnipeg as No. 18658. See map. Economic Overview Property Assessment and Taxes Gods Lake lies within the Precambrian Shield Information is from the 2020 assessment roll region, heavily forested with many small lakes. and Tax Rates and Levy Regulation (2020) of Whitefish in Gods Lake have been downgraded Manitoba Indigenous and Northern Relations. to cutters and not economical to harvest, so there is no commercial fishing. Relatively small Value of Assessment amounts of fish are taken from outlying lakes. Business $91,400 Trapping occurs in the Gods Lake Registered Real Property $854,000 Trapline Zone. Local lodges are providing Grants-in-lieu $424,740 residents with seasonal guiding jobs. Exempt $255,080 Total $1,625,220 Contacts Rate of Taxation Gods Lake Narrows Community Council General Municipal 5.7 mills General Delivery Gods Lake Narrows, MB R0B 0M0 Business Tax 3.75% School Levies Phone: 204-335-2596 Education Support 8.828 mills Fax: 204-335-2662 Frontier School Division #48 13.202 mills Phone: 204-335-2392 WTP Email: [email protected] Emergency Services Office hours: Monday to Friday 8 a.m. -

Programa Do Workshop Etal
O workshop eTAL é voltado para programadores e ProGrAmA Do WorKShoP etAl à programação, por meio de antenas parabólicas, diretores de canais de televisão pública de países TVs por assinatura, TVs Universitárias parceiras, Iberoamericanos. O curso pretende beneficiar 20 UHF e VHF. O Canal Futura é resultado da parceria DiA 1 – DomiNGo, 21 De julho entre organizações da iniciativa privada, unidas pelo profissionais dessas televisões. Esse espaço tem como compromisso de investir socialmente e líderes em objetivo apresentar os desafios da produção interativa para tv e moBiliZAção SoCiAl seus segmentos. Os parceiros mantenedores são: multiplataformas e novas possibilidades de construção O workshop “TV e Mobilização Social” tem o Confederação Nacional da Indústria (CNI), CNN, de diálogo com a audiência. Além de apresentar objetivo de apresentar como, para além da tela da FIESP, FIRJAN, Fundação Bradesco; Fundação Itaú oportunidades inventivas e eficientes de promover a TV, o Canal Futura: atua em diferentes estratégias Social; Fundação Vale; Gerdau; Grupo Votorantim, Rede Globo e SEBRAE. produção dos canais para além da tela da televisão. nos territórios; os principais projetos de educação, De 21 A 26 de julho de 2013, direitos humanos junto a educadores e jovens em que está envolvido; além de uma experimentação da MONTEVIDEU, URUGUAI DiA 2 – SeGuNDA-feirA, 22 De julho PArA Quem? metodologia de trabalho com conteúdos do canal. DeSeNvolvimeNto De ProjetoS iNterAtivoS INSCRIÇÕES: As atividades são destinadas a diretores dos canais, O Futura estende seu compromisso com a 10 de maio a diretores de programas, gerentes de produção transformação social brasileira, atuando nos territórios Recorreremos o processo criativo da produção de 10 de junho de 2013 e coprodução de conteúdo, áreas de aquisição de forma presencial através de uma equipe de projetos interativos e aprofundaremos as estruturas das televisões públicas e culturais de países mobilizadores. -

CIUR-FM Winnipeg – Licence Renewals
Broadcasting Decision CRTC 2015-261 PDF version Reference: 2015-52 Ottawa, 18 June 2015 Native Communication Inc. Thompson and Winnipeg, Manitoba Applications 2014-0923-5 and 2014-0928-5, received 10 and 11 September 2014 CINC-FM Thompson and its transmitters; CIUR-FM Winnipeg – Licence renewals The Commission renews the broadcasting licences for the Type B Native radio stations CINC-FM Thompson and its transmitters, and CIUR-FM Winnipeg, from 1 September 2015 to 31 August 2022. Introduction 1. Native Communication Inc. filed applications to renew the broadcasting licences for the following Type B Native radio stations, which expire 31 August 2015. Application Call sign and location number 2014-0923-5 CINC-FM Thompson, Manitoba, and its transmitters CICP-FM Cranberry Portage CIFF-FM Flin Flon CINR-FM Norway House CISI-FM South Indian Lake CIST-FM St. Theresa Point CISV-FM Swan River CITP-FM The Pas Indian Reserve CIWM-FM Brandon CIWR-FM Waterhen VF2106 Lac Brochet VF2107 Poplar River VF2108 Red Sucker Lake VF2109 Tadoule Lake VF2167 Pukatawagan VF2168 Wabowden VF2174 Gods Lake Narrows VF2175 God’s River VF2195 Cross Lake VF2196 Berens River VF2198 Garden Hill VF2199 Shamattawa VF2220 Brochet VF2222 Nelson House VF2261 Cormorant VF2262 Duck Bay VF2263 Grand Rapids VF2264 Pikwitonei VF2265 Split Lake VF2312 Churchill VF2313 Moose Lake VF2314 Oxford House VF2333 Gillam VF2334 Fox Lake, Alberta VF2335 Lake Manitoba VF2336 Griswold VF2337 Easterville VF2338 Thicket Portage VF2339 Bloodvein VF2340 Hollow Water First Nations VF2342 Sherridon VF2382 Long Plain VF2404 Jackhead VF2405 Pauingassi First Nation VF2406 Leaf Rapids VF2407 Little Grand Rapids VF2420 Camperville VF2421 Dauphin River VF2422 Ilford VF2423 Lynn Lake VF2462 Snow Lake VF2503 Fisher River VF2504 Paint Lake 2014-0928-5 CIUR-FM Winnipeg, Manitoba 2. -

Community Liaison Program: Bridging Land-Use Perspectives of First Nation Communities and the Minerals Resource Sector in Manitoba by L.A
GS-19 Community liaison program: bridging land-use perspectives of First Nation communities and the minerals resource sector in Manitoba by L.A. Murphy Murphy, L.A. 2011: Community liaison program: bridging land-use perspectives of First Nation communities and the minerals resource sector in Manitoba; in Report of Activities 2011, Manitoba Innovation, Energy and Mines, Manitoba Geological Survey, p. 180–181. Summary Model Forest Junior Rangers The Manitoba Geological Survey (MGS) community program, Nopiming Provincial liaison program provides a geological contact person Park on the east side of Lake for Manitoba First Nation communities and the Winnipeg (Figure GS-19-1) minerals resource sector. The mandate for this program Red Sucker Lake First Nation in the Island Lake acknowledges and respects the First Nation land-use traditional land-use area perspective, allows for an open exchange of mineral Bunibonibee Cree Nation in the Oxford House information, and encourages the integration of geology traditional land-use area and mineral-resource potential into the land-use planning Sapotaweyak First Nation Community Interest Zone process. Timely information exchange is critical to all Gods Lake First Nation in Gods Lake Narrows stakeholders, and open communication of all concerns Tataskweyak Cree Nation in Split Lake regarding multiple land-use issues reduces timelines and mitigates potential impacts to Aboriginal and Treaty rights. Manitoba Keewatinowi Okimakanak Inc. (MKO) Schools, communities and mineral industry stakeholders representing Manitoba’s northern First Nations and throughout Manitoba access the program during land-use Tribal councils planning processes, encouraging a balanced approach to College Pierre-Elliot-Trudeau, Transcona School economic development in traditional land-use areas. -

Pdfs GST-HST Municipal Rebates 2018 E.Xlsx
GST/HST Incremental Federal Rebate for Municipalities Report - January 1 to December 31, 2018 Manitoba PAYMENT LEGAL NAME CITY NAME FSA AMOUNT 2625360 MANITOBA ASSOCIATION INC. NEEPAWA R0J $1,112.09 285 PEMBINA INC WINNIPEG R2K $11,916.31 4508841 MANITOBA ASSOCIATION INC WINNIPEG R2K $1,519.18 474 HARGRAVE CORPORATION WINNIPEG R3A $2,653.46 6869166 MANITOBA LTD. SANFORD R0G $6,712.69 7049651 MANITOBA ASSOCIATION INC. WINNIPEG R3B $330,332.94 ACADEMY ROAD BUSINESS IMPROVMENT ZONE WINNIPEG R3N $6,535.53 AGASSIZ WEED CONTROL DISTRICT BEAUSEJOUR R0E $244.81 ALTONA RURAL WATER SERVICES CO-OP LTD ALTONA R0G $2,145.25 ARBORG BI-FROST PARKS & RECREATION COMMISSION ARBORG R0C $4,415.00 ARGYLE-LORNE-SOMERSET WEED CONTROL DISTRICT BALDUR R0K $322.95 ARLINGTONHAUS INC. WINNIPEG R2K $6,353.08 ARTEMIS HOUSING CO-OP LTD WINNIPEG R3A $1,573.30 ASTRA NON-PROFIT HOUSING CORPORATION WINNIPEG R2K $2,548.64 AUTUMN HOUSE INC. WINNIPEG R3E $7,366.31 BAPTIST MISSION APARTMENTS INC. WINNIPEG R3E $3,828.08 BARROWS COMMUNITY COUNCIL BARROWS R0L $2,713.78 BEAUSEJOUR BROKENHEAD DEVELOPMENT CORP BEAUSEJOUR R0E $4,669.11 BETELSTADUR HOUSING COOPERATIVE LTD WINNIPEG R3A $669.10 BETHANIAHAUS INC. WINNIPEG R2K $6,160.12 BIBLIOTHÉQUE MONTCALM LIBRARY SAINT-JEAN-BAPTISTE R0G $177.01 BIBLIOTHÉQUE REGIONALE JOLYS REGIONAL LIBRARY SAINT-PIERRE-JOLYS R0A $761.21 BIBLIOTHÉQUE TACHÉ LIBRARY LORETTE R0A $729.46 BISSETT COMMUNITY COUNCIL BISSETT R0E $4,346.40 BLUMENFELD HOCHFELD WATER CO-OP LTD WINKLER R6W $540.72 BLUMENORT SENIOR CITIZENS HOUSING INC. STEINBACH R5G $834.10 BOISSEVAIN -

Broadcasting Decision CRTC 2021-266
Broadcasting Decision CRTC 2021-266 PDF version Ottawa, 5 August 2021 Canadian Broadcasting Corporation Across Canada Various television and radio programming undertakings – Administrative renewals 1. The Commission renews the broadcasting licences for the television and radio programming undertakings set out in the appendix to this decision from 1 September 2021 to 31 March 2022, subject to the terms and conditions in effect under the current licences. The Commission also extends the distribution orders for the television programming undertakings CBC News Network, ICI RDI and ICI ARTV until 31 March 2022.1 2. In Broadcasting Decision 2020-201, the Commission renewed these licences administratively from 1 September 2020 to 31 August 2021, and extended the distribution orders for CBC News Network, ICI RDI and ICI ARTV until 31 August 2021. 3. This decision does not dispose of any issue that may arise with respect to the renewal of these licences. Secretary General Related documents Various television and radio programming undertakings – Administrative Renewals, Broadcasting Decision CRTC 2020-201, 22 June 2020 Distribution of the programming service of ARTV inc. by licensed terrestrial broadcasting distribution undertakings, Broadcasting Order CRTC 2013-375, 8 August 2013 Canadian Broadcasting Corporation – Licence renewals, Broadcasting Decision CRTC 2013-263 and Broadcasting Orders CRTC 2013-264 and 2013-265, 28 May 2013 This decision is to be appended to each licence. 1 For ICI RDI and CBC News Network, see Appendices 9 and 10, respectively, -
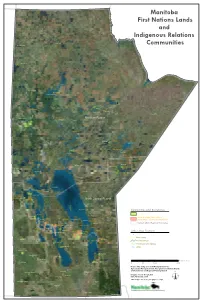
Manitoba First Nations Lands and Indigenous Relations Communities
60N Manitoba First Nations Lands and 59N Indigenous Relations Sayisi Dene Northlands Dene Communities 89W 58N Barren Lands Brochet 57N Marcel Colomb South Indian Lake O-Pipon-Na-Piwin 90W Gillam Tataskweyak Granville Lake Ilford War Lake York Factory 56N Fox Lake Shamattawa Nelson House Mathias Colomb Northern Region Nisichawayasihk !Thompson Pikwitonei Thicket Portage Sherridon 55N Oxford House Wabowden Bunibonibee Manto Sipi Flin !Flon 102W Herb Lake Landing Gods Lake Narrows 93W 92W 91W Cross Lake 96W 95W 94W 97W 99W 98W 101W 100W God's Lake Cross Lake Red Sucker Lake Cormorant Red Sucker Lake Garden Hill Norway House 54N Wasagamack Opaskwayak Norway House Island Lake The Pas Mosakahiken St. Theresa Point Moose Lake Misipawistik Easterville Chemawawin 53N Dawson Bay Poplar River Red Deer Lake Barrows Sapotaweyak Powell National Mills Baden Pelican Rapids North Central Region Wuskwi Sipihk Berens River Berens River Communities and Boundaries Pauingassi Duck Bay First Nations Lands Pine Creek Little Grand Rapids 52N Little Grand Rapids Northern Affairs Communities Skownan Mallard Camperville Dauphin River Dauphin River Jackhead (Indigenous Relations Communities) Rock Ridge Princess Harbour Waterhen Bloodvein Northern Affairs Regional Boundaries Salt Point Homebrook - Peonan Point Lake St. Martin Matheson Island Little Saskatchewan Pine Dock Meadow Portage Spence Lake Pinaymootang Loon Straits Dallas / Red Rose Fisher Bay Crane River O-Chi-Chak-Ko-Sipi Other Map Features Fisher River ! Harwill Cities Peguis Aghaming Expressway Valley -

Gods Lake Narrows
Gods Lake Narrows Community Overview Trapping occurs in the Gods Lake Registered Trapline Zone. Local lodges are providing Two communities share the name Gods Lake, residents with seasonal guiding jobs. the community and the adjacent God’s Lake First Nation reserve. Information in this profile Community Statistics relates to the non-reserve side, unless otherwise noted. Population 1985 112 Access 1991 105 The community is located along the lakeshore of 1996 101 the narrow portion of Gods Lake 224 kilometres 2001 113 (km) by air southeast of Thompson and 547 km 2006 88 by air northeast of Winnipeg. 2011 85 *Information is from Statistics Canada. Governance The community is represented by a mayor and Households council under The Northern Affairs Act. There are 46 housing units. Community Contacts Boundary Manitoba Regulation 67/2009 refers to Director Gods Lake Narrows Community Council of Surveys at Winnipeg as No. 18658. See map. General Delivery Gods Lake Narrows, MB R0B 0M0 Property Assessment and Taxes Information is from the 2015 assessment roll Phone: 204-335-2596 and Manitoba Regulation 117/2015 tax rates Fax: 204-335-2662 and levy of Manitoba Indigenous and Municipal Email: [email protected] Relations. Office Hours and Staff Value of Assessment Monday to Friday: 8 a.m. – 4 p.m. Business $77,700 Real Property $675,440 The community employs a community Grants-in-lieu $379,150 administrative officer, public works employee, Exempt $71,390 volunteer fire chief with several trained volunteer Total $1,203,680 firefighters, custodian and back-up operator. Rate of Taxation General Municipal mills 5.7 Economic Overview Business Tax 3.75% School Levies Gods Lake lies within the Precambrian Shield Foundation mills 11.61 region which is heavily forested and dotted with Frontier School Division #48 mills 15.399 many small lakes. -
Local and Regional Identity Action Plan
LLOCALOCAL AANDND RREGIONALEGIONAL IIDENTITYDENTITY AACTIONCTION PPLANLAN TTHEHE TTHOMPSONHOMPSON EECONOMICCONOMIC DDIVERSIFICATIONIVERSIFICATION WWORKINGORKING GGROUPROUP CCONSULTATIONONSULTATION SUMMARYSUMMARY REPORTREPORT JanuaryJanuary 20132013 THE THOMPSON ECONOMIC DIVERSIFICATION WORKING GROUP 2 | The City of Thompson | Keewatin Tribal Council | The Manitoba Metis Federation | Manitoba Keewatinowi Okimakanak | Thompson Unlimited ACTION PLAN #4: LOCAL AND REGIONAL IDENTITY - CONSULTATION SUMMARY REPORT LLOCALOCAL AANDND RREGIONALEGIONAL IIDENTITYDENTITY AACTIONCTION PPLANLAN | 3 TTHEHE TTHOMPSONHOMPSON EECONOMICCONOMIC DDIVERSIFICATIONIVERSIFICATION WWORKINGORKING GGROUPROUP CCONSULTATIONONSULTATION SUMMARYSUMMARY REPORTREPORT JanuaryJanuary 20132013 AActionProvincection of ManitobaPPlanlan ##4: |4 Northern: LLocaloc aAssociationl aandnd RRegionalof eCommunitygional Councils IIdentityden t| i tNisichawayasihky - CConsultationonsu Creelta tNationion |SSummary Thompsonumma Chamberry RReporte ofp oCommerrt ce | Vale Supported by: CITY THOMPSON (CHAIR) UNLIMITED PROVINCE of MANITOBA THOMPSON CHAMBER OF COMMERCE FEDERAL THOMPSON GOVERNMENT VALE ECONOMIC MKO UNITED DIVERSIFICATION STEEL WORKERS LOCAL 6166 WORKING GROUP KTC rePLAN MMF NCN Working Group Members NACC Invited Stakeholders THE THOMPSON ECONOMIC DIVERSIFICATION WORKING GROUP The City of Thompson | Keewatin Tribal Council | The Manitoba Metis Federation | Manitoba Keewatinowi Okimakanak | Thompson Unlimited ACTION PLAN #4: LOCAL AND REGIONAL IDENTITY - CONSULTATION SUMMARY REPORT