The Pharmacology, Pharmacokinetics And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
WADA Technical Letter – TL07 ANDARINE
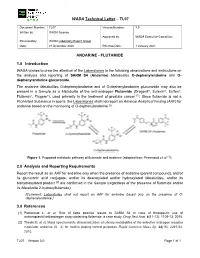
WADA Technical Letter – TL07 Document Number: TL07 Version Number: 3.0 Written by: WADA Science Approved by: WADA Executive Committee Reviewed by: WADA Laboratory Expert Group Date: 21 December 2020 Effective Date: 1 January 2021 ANDARINE - FLUTAMIDE 1.0 Introduction WADA wishes to draw the attention of the Laboratories to the following observations and instructions on the analysis and reporting of SARM S4 (Andarine) Metabolites O-dephenylandarine and O- dephenylandarine glucuronide. The andarine Metabolites O-dephenylandarine and of O-dephenylandarine glucuronide may also be present in a Sample as a Metabolite of the anti-androgen Flutamide (Drogenil®, Eulexin®, Euflex®, Flutamin®, Flugere®), used primarily in the treatment of prostate cancer [1]. Since flutamide is not a Prohibited Substance in sports, the Laboratories shall not report an Adverse Analytical Finding (AAF) for andarine based on the monitoring of O-dephenylandarine [2]. Figure 1. Proposed metabolic pathway of flutamide and andarine (adapted from Perrenoud et al. [1]). 2.0 Analysis and Reporting Requirements Report the result as an AAF for andarine only when the presence of andarine (parent compound), and/or its glucuronic acid conjugate, and/or its deacetylated and/or hydroxylated Metabolites, and/or its bishydroxylated product [2] are confirmed in the Sample (regardless of the presence of flutamide and/or its Metabolite 2-hydroxyflutamide); [Comment: Laboratories shall not report an AAF for andarine based only on the presence of O- dephenylandarine.] 3.0 References [1] Perrenoud L. et al. Risk of false positive results to SARM S4 in case of therapeutic use of antineoplastic/antiandrogen drug containing flutamide: a case study. -

Prnu-BICALUTAMIDE
PRODUCT MONOGRAPH PrNU-BICALUTAMIDE Bicalutamide Tablets, 50 mg Non-Steroidal Antiandrogen NU-PHARM INC. DATE OF PREPARATION: 50 Mural Street, Units 1 & 2 October 16, 2009 Richmond Hill, Ontario L4B 1E4 Control#: 133521 Page 1 of 27 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION....................................................... 3 SUMMARY PRODUCT INFORMATION ............................................................................. 3 INDICATIONS AND CLINICAL USE ................................................................................... 3 CONTRAINDICATIONS ........................................................................................................ 3 WARNINGS AND PRECAUTIONS....................................................................................... 4 ADVERSE REACTIONS......................................................................................................... 5 DRUG INTERACTIONS ......................................................................................................... 9 DOSAGE AND ADMINISTRATION ................................................................................... 10 OVERDOSAGE...................................................................................................................... 10 ACTION AND CLINICAL PHARMACOLOGY.................................................................. 10 STORAGE AND STABILITY............................................................................................... 11 DOSAGE FORMS, COMPOSITION AND PACKAGING -

Package Leaflet: Information for the Patient Desogestrel Rowex
Package leaflet: Information for the patient Desogestrel Rowex 75 microgram Film-coated tablets desogestrel Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Desogestrel Rowex is and what it is used for 2. What you need to know before you take Desogestrel Rowex 4. Possible side effects 5. How to store Desogestrel Rowex 6. Contents of the pack and other information 1. What Desogestrel Rowex is and what it is used for Desogestrel Rowex used to prevent pregnancy. There are 2 main kinds of hormone contraceptive. - The combined pill, "The Pill", which contains 2 types of female sex hormone an oestrogen and a progestogen, - The progestogen-only pill, POP, which doesn't contain an oestrogen. Desogestrel Rowex is a progestogen-only-pill (POP). Desogestrel Rowex contains a small amount of one type of female sex hormone, the progestogen desogestrel. Most POPs work primarily by preventing the sperm cells from entering the womb but do not always prevent the egg cell from ripening, which is the main way that combined pills work. -
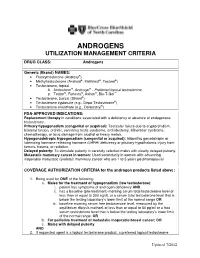
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

The Effects of Androgens and Antiandrogens on Hormone Responsive Human Breast Cancer in Long-Term Tissue Culture1
[CANCER RESEARCH 36, 4610-4618, December 1976] The Effects of Androgens and Antiandrogens on Hormone responsive Human Breast Cancer in Long-Term Tissue Culture1 Marc Lippman, Gail Bolan, and Karen Huff MedicineBranch,NationalCancerInstitute,Bethesda,Maryland20014 SUMMARY Information characterizing the interaction between an drogens and breast cancer would be desirable for several We have examined five human breast cancer call lines in reasons. First, androgens can affect the growth of breast conhinuous tissue culture for andmogan responsiveness. cancer in animals. Pharmacological administration of an One of these cell lines shows a 2- ho 4-fold stimulation of drogens to rats bearing dimathylbenzanthracene-induced thymidina incorporation into DNA, apparent as early as 10 mammary carcinomas is associated wihh objective humor hr following androgen addition to cells incubated in serum regression (h9, 22). Shionogi h15 cells, from a mouse mam free medium. This stimulation is accompanied by an ac many cancer in conhinuous hissue culture, have bean shown celemation in cell replication. Antiandrogens [cyproterona to be shimulatedby physiological concentrations of andro acetate (6-chloro-17a-acelata-1,2a-methylena-4,6-pregna gen (21), thus suggesting that some breast cancer might be diene-3,20-dione) and R2956 (17f3-hydroxy-2,2,1 7a-tnima androgen responsive in addition to being estrogen respon thoxyastra-4,9,1 1-Inane-i -one)] inhibit both protein and siva. DNA synthesis below control levels and block androgen Evidence also indicates that tumor growth in humans may mediahed stimulation. Prolonged incubahion (greahenhhan be significantly altered by androgens. About 20% of pahianhs 72 hn) in antiandrogen is lethal. -

Risk of Breast Cancer After Stopping Menopausal Hormone Therapy In
Risk of breast cancer after stopping menopausal hormone therapy in the E3N cohort Agnès Fournier, Sylvie Mesrine, Laure Dossus, Marie-Christine Boutron-Ruault, Françoise Clavel-Chapelon, Nathalie Chabbert-Buffet To cite this version: Agnès Fournier, Sylvie Mesrine, Laure Dossus, Marie-Christine Boutron-Ruault, Françoise Clavel- Chapelon, et al.. Risk of breast cancer after stopping menopausal hormone therapy in the E3N cohort. Breast Cancer Research and Treatment, Springer Verlag, 2014, 145 (2), pp.535-43. 10.1007/s10549- 014-2934-6. inserm-01319982 HAL Id: inserm-01319982 https://www.hal.inserm.fr/inserm-01319982 Submitted on 23 May 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. TITLE PAGE Risk of breast cancer after stopping menopausal hormone therapy in the E3N cohort Authors : Agnès Fournier1,2,3, Sylvie Mesrine1,2,3, Laure Dossus1,2,3, Marie-Christine Boutron- Ruault1,2,3, Françoise Clavel-Chapelon1,2,3, Nathalie Chabbert-Buffet4 Affiliations: 1. Inserm, Center for research in Epidemiology and Population Health, U1018, Nutrition, Hormones and Women’s Health team, F-94807, Villejuif, France 2. Univ Paris-Sud, UMRS 1018, F-94807, Villejuif, France 3. Institut Gustave Roussy, F-94805, Villejuif, France 4. -

Download PDF File
Ginekologia Polska 2019, vol. 90, no. 9, 520–526 Copyright © 2019 Via Medica ORIGINAL PAPER / GYNECologY ISSN 0017–0011 DOI: 10.5603/GP.2019.0091 Anti-androgenic therapy in young patients and its impact on intensity of hirsutism, acne, menstrual pain intensity and sexuality — a preliminary study Anna Fuchs, Aleksandra Matonog, Paulina Sieradzka, Joanna Pilarska, Aleksandra Hauzer, Iwona Czech, Agnieszka Drosdzol-Cop Department of Pregnancy Pathology, Department of Woman’s Health, School of Health Sciences in Katowice, Medical University of Silesia, Katowice, Poland ABSTRACT Objectives: Using anti-androgenic contraception is one of the methods of birth control. It also has a significant, non-con- traceptive impact on women’s body. These drugs can be used in various endocrinological disorders, because of their ability to reduce the level of male hormones. The aim of our study is to establish a correlation between taking different types of anti-androgenic drugs and intensity of hirsutism, acne, menstrual pain intensity and sexuality . Material and methods: 570 women in childbearing age that had been using oral contraception for at least three months took part in our research. We examined women and asked them about quality of life, health, direct causes and effects of that treatment, intensity of acne and menstrual pain before and after. Our research group has been divided according to the type of gestagen contained in the contraceptive pill: dienogest, cyproterone, chlormadynone and drospirenone. Ad- ditionally, the control group consisted of women taking oral contraceptives without antiandrogenic component. Results: The mean age of the studied group was 23 years ± 3.23. 225 of 570 women complained of hirsutism. -

CASODEX (Bicalutamide)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Gynecomastia and breast pain have been reported during treatment with These highlights do not include all the information needed to use CASODEX 150 mg when used as a single agent. (5.3) CASODEX® safely and effectively. See full prescribing information for • CASODEX is used in combination with an LHRH agonist. LHRH CASODEX. agonists have been shown to cause a reduction in glucose tolerance in CASODEX® (bicalutamide) tablet, for oral use males. Consideration should be given to monitoring blood glucose in Initial U.S. Approval: 1995 patients receiving CASODEX in combination with LHRH agonists. (5.4) -------------------------- RECENT MAJOR CHANGES -------------------------- • Monitoring Prostate Specific Antigen (PSA) is recommended. Evaluate Warnings and Precautions (5.2) 10/2017 for clinical progression if PSA increases. (5.5) --------------------------- INDICATIONS AND USAGE -------------------------- ------------------------------ ADVERSE REACTIONS ----------------------------- • CASODEX 50 mg is an androgen receptor inhibitor indicated for use in Adverse reactions that occurred in more than 10% of patients receiving combination therapy with a luteinizing hormone-releasing hormone CASODEX plus an LHRH-A were: hot flashes, pain (including general, back, (LHRH) analog for the treatment of Stage D2 metastatic carcinoma of pelvic and abdominal), asthenia, constipation, infection, nausea, peripheral the prostate. (1) edema, dyspnea, diarrhea, hematuria, nocturia, and anemia. (6.1) • CASODEX 150 mg daily is not approved for use alone or with other treatments. (1) To report SUSPECTED ADVERSE REACTIONS, contact AstraZeneca Pharmaceuticals LP at 1-800-236-9933 or FDA at 1-800-FDA-1088 or ---------------------- DOSAGE AND ADMINISTRATION ---------------------- www.fda.gov/medwatch The recommended dose for CASODEX therapy in combination with an LHRH analog is one 50 mg tablet once daily (morning or evening). -

Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer
Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer Michael Danquah, Charles B. Duke, Renukadevi Patil, Duane D. Miller & Ram I. Mahato Pharmaceutical Research An Official Journal of the American Association of Pharmaceutical Scientists ISSN 0724-8741 Volume 29 Number 8 Pharm Res (2012) 29:2079-2091 DOI 10.1007/s11095-012-0737-1 1 23 Your article is protected by copyright and all rights are held exclusively by Springer Science+Business Media, LLC. This e-offprint is for personal use only and shall not be self- archived in electronic repositories. If you wish to self-archive your work, please use the accepted author’s version for posting to your own website or your institution’s repository. You may further deposit the accepted author’s version on a funder’s repository at a funder’s request, provided it is not made publicly available until 12 months after publication. 1 23 Author's personal copy Pharm Res (2012) 29:2079–2091 DOI 10.1007/s11095-012-0737-1 RESEARCH PAPER Combination Therapy of Antiandrogen and XIAP Inhibitor for Treating Advanced Prostate Cancer Michael Danquah & Charles B. Duke III & Renukadevi Patil & Duane D. Miller & Ram I. Mahato Received: 4 February 2012 /Accepted: 9 March 2012 /Published online: 27 March 2012 # Springer Science+Business Media, LLC 2012 ABSTRACT Results CBDIV17 was more potent than bicalutamide and Purpose Overexpression of the androgen receptor (AR) and inhibited proliferation of C4-2 and LNCaP cells, IC50 for CBDIV17 anti-apoptotic genes including X-linked inhibitor of apoptosis was ∼12 μMand∼21 μM in LNCaP and C4-2 cells, respectively, protein (XIAP) provide tumors with a proliferative advantage. -

Campro Catalog Stable Isotope
Introduction & Welcome Dear Valued Customer, We are pleased to present to you our Stable Isotopes Catalog which contains more than three thousand (3000) high quality labeled compounds. You will find new additions that are beneficial for your research. Campro Scientific is proud to work together with Isotec, Inc. for the distribution and marketing of their stable isotopes. We have been working with Isotec for more than twenty years and know that their products meet the highest standard. Campro Scientific was founded in 1981 and we provide services to some of the most prestigious universities, research institutes and laboratories throughout Europe. We are a research-oriented company specialized in supporting the requirements of the scientific community. We are the exclusive distributor of some of the world’s leading producers of research chemicals, radioisotopes, stable isotopes and environmental standards. We understand the requirements of our customers, and work every day to fulfill them. In working with us you are guaranteed to receive: - Excellent customer service - High quality products - Dependable service - Efficient distribution The highly educated staff at Campro’s headquarters and sales office is ready to assist you with your questions and product requirements. Feel free to call us at any time. Sincerely, Dr. Ahmad Rajabi General Manager 180/280 = unlabeled 185/285 = 15N labeled 181/281 = double labeled (13C+15N, 13C+D, 15N+18O etc.) 186/286 = 12C labeled 182/282 = d labeled 187/287 = 17O labeled 183/283 = 13C labeleld 188/288 = 18O labeled 184/284 = 16O labeled, 14N labeled 189/289 = Noble Gases Table of Contents Ordering Information.................................................................................................. page 4 - 5 Packaging Information .............................................................................................. -

COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone During SARS-Cov-2 Infection
pharmaceuticals Review COVID-19—The Potential Beneficial Therapeutic Effects of Spironolactone during SARS-CoV-2 Infection Katarzyna Kotfis 1,* , Kacper Lechowicz 1 , Sylwester Drozd˙ zal˙ 2 , Paulina Nied´zwiedzka-Rystwej 3 , Tomasz K. Wojdacz 4, Ewelina Grywalska 5 , Jowita Biernawska 6, Magda Wi´sniewska 7 and Miłosz Parczewski 8 1 Department of Anesthesiology, Intensive Therapy and Acute Intoxications, Pomeranian Medical University in Szczecin, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacokinetics and Monitored Therapy, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 3 Institute of Biology, University of Szczecin, 71-412 Szczecin, Poland; [email protected] 4 Independent Clinical Epigenetics Laboratory, Pomeranian Medical University, 71-252 Szczecin, Poland; [email protected] 5 Department of Clinical Immunology and Immunotherapy, Medical University of Lublin, 20-093 Lublin, Poland; [email protected] 6 Department of Anesthesiology and Intensive Therapy, Pomeranian Medical University in Szczecin, 71-252 Szczecin, Poland; [email protected] 7 Clinical Department of Nephrology, Transplantology and Internal Medicine, Pomeranian Medical University, 70-111 Szczecin, Poland; [email protected] 8 Department of Infectious, Tropical Diseases and Immune Deficiency, Pomeranian Medical University in Szczecin, 71-455 Szczecin, Poland; [email protected] * Correspondence: katarzyna.kotfi[email protected]; Tel.: +48-91-466-11-44 Abstract: In March 2020, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2 was declared Citation: Kotfis, K.; Lechowicz, K.; a global pandemic by the World Health Organization (WHO). The clinical course of the disease is Drozd˙ zal,˙ S.; Nied´zwiedzka-Rystwej, unpredictable but may lead to severe acute respiratory infection (SARI) and pneumonia leading to P.; Wojdacz, T.K.; Grywalska, E.; acute respiratory distress syndrome (ARDS). -

Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals
Journal of Clinical Medicine Review Hormonal Treatment Strategies Tailored to Non-Binary Transgender Individuals Carlotta Cocchetti 1, Jiska Ristori 1, Alessia Romani 1, Mario Maggi 2 and Alessandra Daphne Fisher 1,* 1 Andrology, Women’s Endocrinology and Gender Incongruence Unit, Florence University Hospital, 50139 Florence, Italy; [email protected] (C.C); jiska.ristori@unifi.it (J.R.); [email protected] (A.R.) 2 Department of Experimental, Clinical and Biomedical Sciences, Careggi University Hospital, 50139 Florence, Italy; [email protected]fi.it * Correspondence: fi[email protected] Received: 16 April 2020; Accepted: 18 May 2020; Published: 26 May 2020 Abstract: Introduction: To date no standardized hormonal treatment protocols for non-binary transgender individuals have been described in the literature and there is a lack of data regarding their efficacy and safety. Objectives: To suggest possible treatment strategies for non-binary transgender individuals with non-standardized requests and to emphasize the importance of a personalized clinical approach. Methods: A narrative review of pertinent literature on gender-affirming hormonal treatment in transgender persons was performed using PubMed. Results: New hormonal treatment regimens outside those reported in current guidelines should be considered for non-binary transgender individuals, in order to improve psychological well-being and quality of life. In the present review we suggested the use of hormonal and non-hormonal compounds, which—based on their mechanism of action—could be used in these cases depending on clients’ requests. Conclusion: Requests for an individualized hormonal treatment in non-binary transgender individuals represent a future challenge for professionals managing transgender health care. For each case, clinicians should balance the benefits and risks of a personalized non-standardized treatment, actively involving the person in decisions regarding hormonal treatment.