Complete Mesocolic Excision with Central Vascular Ligation in Comparison with Conventional Surgery for the Right Colon Cancer: an Italian Randomized Trial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Allegati Al Comunicato Ufficiale N. 37 Del 13/02/2020
ALLEGATI AL COMUNICATO UFFICIALE N. 37 DEL 13/02/2020 CAMPIONATO 38 TERZA CATEGORIA ------------------------------------------------------------------------------------------------------------------------------------------------------------------- GIRONE A GIORNATA 4 RITORNO ------------------------------------------------------------------------------------------------------------------------------------------------------------------- 1) AVIGLIANA CALCIO TETTI FRANCESI RIVALTA 486 GUIDO BERTINI SANT'AMBROGIO DI TORINO 23/02/20 14:30 VIA BERTASSI 11 2) CIRCOLO DA GIAU DT ALMESE CALCIO 93 COMUNALE BRUINO 23/02/20 14:30 VIA PIOSSASCO 35 3) LENCI POIRINO O.N.L.U.S. TORRE PELLICE 425 COMUNALE POIRINO 23/02/20 14:30 VIA FONTE ANTICO 16 4) REAL 909 SPORTINSIEME PIOBESI T.SE 4328 CERTEZZA GRUGLIASCO 23/02/20 14:30 C.SO ALLAMANO 79 5) RUBIANA CALCIO A.S.D. PINEROLESE A.P. 1553 COMUNALE RUBIANA 23/02/20 14:30 BORGATA RATTA 15 6) SAN REMO 72 SRL SAN LUIGI SANTENA 931 SINTETICO RAPID TORINO 23/02/20 14:30 VIA OSOPPO 3 7) SCALENGHE ROLETTO VAL NOCE 516 COMUNALE SCALENGHE 23/02/20 14:30 VIA VERDI 1 ------------------------------------------------------------------------------------------------------------------------------------------------------------------- CAMPIONATO P8 UNDER 19 PROV. ------------------------------------------------------------------------------------------------------------------------------------------------------------------- GIRONE A GIORNATA 4 RITORNO ------------------------------------------------------------------------------------------------------------------------------------------------------------------- -

ALFIERO GISELLA Via G. Falcone, 4 – 10060 Candiolo
F ORMATO EUROPEO PER IL CURRICULUM VITAE INFORMAZIONI PERSONALI Nome ALFIERO GISELLA Indirizzo Via G. Falcone, 4 – 10060 Candiolo (TO) Telefono 348/6068670 Fax 011-2404235 E-mail [email protected] Nazionalità Italiana Data di nascita 04/05/1974 ESPERIENZA LAVORATIVA • Date (da – a) Da 01/2002 a OGGI • Nome e indirizzo del datore di Dasein S.r.l. - Lungo Dora Colletta, 81 Torino lavoro • Tipo di azienda o settore Consulenza, Ricerca, Formazione nel campo della Pubblica Amministrazione • Tipo di impiego Coordinatrice regione Piemonte, consulente e formatrice • Principali mansioni e responsabilità Da gennaio a giugno 2002 ho collaborato con la Dasein S.r.l. occupandomi di organizzazione e tutoraggio nell’ambito di corsi formativi. Da luglio 2002 sono stata assunta a tempo indeterminato per occuparmi di valutazione del personale, consulenza e formazione per diversi Enti Locali e dal 2013 sono stata nominata responsabile della sede piemontese della Dasein S.r.l. e componente del Consiglio di Amministrazione della società. Principali attività svolte: Nuclei di Valutazione Nell’ambito di tali progetti collaboro nella realizzazione di sistemi di valutazione ai sensi del Contratto Collettivo Nazionale di Lavoro Enti Locali, in particolare riferiti ai dirigenti e alle posizioni organizzative (valutazione della posizione e del risultato) ed ai sistemi permanenti di valutazione ex art.6 del CCNL 31/3/99, relativi alle prestazioni e alle progressioni del personale dell'Ente. Sono componente di nuclei di Valutazione nei Comuni di: Candiolo, None, Banchette, Buttigliera Alta, Coazze, Pecetto Torinese, Chiaverano, Burolo, Villanova C.se, Locana, Lombardore, Villarbasse, Montalto Dora, Rivarolo C.se, Alagna(VC), Serravalle Sesia, Varallo Sesia, Romagnano Sesia, S. -

Nome ALFIERO GISELLA Indirizzo Via G. Falcone, 4 – 10060 Candiolo (TO) Telefono 348/6068670 Fax 011-2404235 E-Mail [email protected]
F ORMATO EUROPEO PER IL CURRICULUM V I T A E INFORMAZIONI PERSONALI Nome ALFIERO GISELLA Indirizzo Via G. Falcone, 4 – 10060 Candiolo (TO) Telefono 348/6068670 Fax 011-2404235 E-mail [email protected] Nazionalità Italiana Data di nascita 04/05/1974 ESPERIENZA LAVORATIVA • Date (da – a) Da 01/2002 a OGGI • Nome e indirizzo del datore di Dasein S.r.l. - Lungo Dora Colletta, 81 Torino lavoro • Tipo di azienda o settore Consulenza, Ricerca, Formazione nel campo della Pubblica Amministrazione • Tipo di impiego Coordinatrice regione Piemonte, consulente e formatrice • Principali mansioni e responsabilità Da gennaio a gi ugno 2002 ho collaborato con la Dasein S.r.l. occupandomi di organizzazione e tutoraggio nell’ambito di corsi formativi. Da luglio 2002 sono stata assunta a tempo indeterminato per occuparmi di valutazione del personale, consulenza e formazione per diversi Enti Locali e dal 2013 sono stata nominata coordinatrice della sede piemontese della Dasein S.r.l. Principali attività svolte: • Nuclei di Valutazione Nell’ambito di tali progetti collaboro nella realizzazione di sistemi di valutazione ai sensi del Contratto Collettivo Nazionale di Lavoro Enti Locali, in particolare riferiti ai dirigenti e alle posizioni organizzative (valutazione della posizione e del risultato) ed ai sistemi permanenti di valutazione ex art.6 del CCNL 31/3/99, relativi alle prestazioni e alle progressioni del personale dell'Ente. Sono componente di nuclei di Valutazione nei Comuni di: Candiolo, None, Banchette, Buttigliera Alta, Coazze, Pecetto Torinese, Chiaverano, Burolo, Villanova C.se, Lombardore, Villarbasse, Montalto Dora, Comunità Montana Valli Orco e Soana, Rivarolo C.se, Buccinasco, Alagna(VC), Serravalle Sesia, Varallo Sesia, Romagnano Sesia, S. -

Nome / Cognome Luciana MELLANO
CURRICULUM VITAE Informazioni personali Nome / Cognome Luciana MELLANO Responsabile Area Tecnica e Tecnico Manutentiva del Comune di Lombardore (posizione D2) Tel. Ufficio: 011 9956101 int. 2 Fax Ufficio: 011 9956036 E-mail istituzionale: [email protected] [email protected] [email protected] Sito Web: www.comune.lombardore.to.it Link : Centrale Unica di Committenza (interno sito del comune di Lombardore) Sito Web: www.anfiteatromorenico.it Link : Centrale Unica di Committenza (interno sito del anfiteatromorenico) Pagina 1/5 - Curriculum vitae di MELLANO Luciana Istruzione e formazione Istruzione : 1989 Maturità tecnica – Diploma di Geometra conseguito presso l’Istituto XX Aprile di Cuorgnè (TO) 1992 Abilitazione all’esercizio della professione di Geometra Corsi e Formazione : 1997 Enea – Dipartimento Energia : Organizzazione e gestione del controllo delle relazioni presentate ai sensi della L. 10/91. 2002 Distretto Tecnologico per operatore di Sportello Unico Per le attività produttive . 2003 Provincia di Torino: Attività contrattuale della P.A. procedimenti amministrativi. Provincia di Torino : Sicurezza e Prevenzione. 2004 CIAC s.c.rl : La gestione degli appalti. 2005 Distretto Tecnologico del Canavese : Direttiva CEE in materia di aggiudicazione degli appalti pubblici , forniture e servizi. Regione Piemonte – Corep : Corso di Formazione specialistica nel settore della conoscenza e dell’intervento sul paesaggio. 2006 Città di Ciriè – Incontro di formazione sul Codice degli Appalti. ARPA – Corso di formazione per gestione esposti (ambientali) 2007 Provincia di Torino – Corso avanzato per utilizzo PC. Provincia di Torino – Forum “nuove procedure per le varianti ai piani regolatori”. 2008 Provincia di Torino : Il nuovo codice dei Contratti pubblici relativi a lavori, servizi e forniture. -
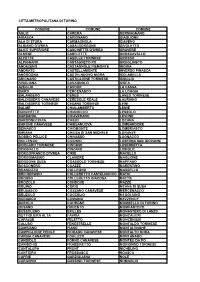
Città Metropolitana Di Torino Comune Comune Comune
CITTÀ METROPOLITANA DI TORINO COMUNE COMUNE COMUNE AGLIÈ CAREMA GERMAGNANO AIRASCA CARIGNANO GIAGLIONE ALA DI STURA CARMAGNOLA GIAVENO ALBIANO D'IVREA CASALBORGONE GIVOLETTO ALICE SUPERIORE CASCINETTE D'IVREA GRAVERE ALMESE CASELETTE GROSCAVALLO ALPETTE CASELLE TORINESE GROSSO ALPIGNANO CASTAGNETO PO GRUGLIASCO ANDEZENO CASTAGNOLE PIEMONTE INGRIA ANDRATE CASTELLAMONTE INVERSO PINASCA ANGROGNA CASTELNUOVO NIGRA ISOLABELLA ARIGNANO CASTIGLIONE TORINESE ISSIGLIO AVIGLIANA CAVAGNOLO IVREA AZEGLIO CAVOUR LA CASSA BAIRO CERCENASCO LA LOGGIA BALANGERO CERES LANZO TORINESE BALDISSERO CANAVESE CERESOLE REALE LAURIANO BALDISSERO TORINESE CESANA TORINESE LEINÌ BALME CHIALAMBERTO LEMIE BANCHETTE CHIANOCCO LESSOLO BARBANIA CHIAVERANO LEVONE BARDONECCHIA CHIERI LOCANA BARONE CANAVESE CHIESANUOVA LOMBARDORE BEINASCO CHIOMONTE LOMBRIASCO BIBIANA CHIUSA DI SAN MICHELE LORANZÈ BOBBIO PELLICE CHIVASSO LUGNACCO BOLLENGO CICONIO LUSERNA SAN GIOVANNI BORGARO TORINESE CINTANO LUSERNETTA BORGIALLO CINZANO LUSIGLIÈ BORGOFRANCO D'IVREA CIRIÈ MACELLO BORGOMASINO CLAVIERE MAGLIONE BORGONE SUSA COASSOLO TORINESE MAPPANO BOSCONERO COAZZE MARENTINO BRANDIZZO COLLEGNO MASSELLO BRICHERASIO COLLERETTO CASTELNUOVO MATHI BROSSO COLLERETTO GIACOSA MATTIE BROZOLO CONDOVE MAZZÈ BRUINO CORIO MEANA DI SUSA BRUSASCO COSSANO CANAVESE MERCENASCO BRUZOLO CUCEGLIO MEUGLIANO BURIASCO CUMIANA MEZZENILE BUROLO CUORGNÈ MOMBELLO DI TORINO BUSANO DRUENTO MOMPANTERO BUSSOLENO EXILLES MONASTERO DI LANZO BUTTIGLIERA ALTA FAVRIA MONCALIERI CAFASSE FELETTO MONCENISIO CALUSO FENESTRELLE MONTALDO -

Uffici Locali Dell'agenzia Delle Entrate E Competenza
TORINO Le funzioni operative dell'Agenzia delle Entrate sono svolte dalle: Direzione Provinciale I di TORINO articolata in un Ufficio Controlli, un Ufficio Legale e negli uffici territoriali di MONCALIERI , PINEROLO , TORINO - Atti pubblici, successioni e rimborsi Iva , TORINO 1 , TORINO 3 Direzione Provinciale II di TORINO articolata in un Ufficio Controlli, un Ufficio Legale e negli uffici territoriali di CHIVASSO , CIRIE' , CUORGNE' , IVREA , RIVOLI , SUSA , TORINO - Atti pubblici, successioni e rimborsi Iva , TORINO 2 , TORINO 4 La visualizzazione della mappa dell'ufficio richiede il supporto del linguaggio Javascript. Direzione Provinciale I di TORINO Comune: TORINO Indirizzo: CORSO BOLZANO, 30 CAP: 10121 Telefono: 01119469111 Fax: 01119469272 E-mail: [email protected] PEC: [email protected] Codice Ufficio: T7D Competenza territoriale: Circoscrizioni di Torino: 1, 2, 3, 8, 9, 10. Comuni: Airasca, Andezeno, Angrogna, Arignano, Baldissero Torinese, Bibiana, Bobbio Pellice, Bricherasio, Buriasco, Cambiano, Campiglione Fenile, Cantalupa, Carignano, Carmagnola, Castagnole Piemonte, Cavour, Cercenasco, Chieri, Cumiana, Fenestrelle, Frossasco, Garzigliana, Inverso Pinasca, Isolabella, La Loggia, Lombriasco, Luserna San Giovanni, Lusernetta, Macello, Marentino, Massello, Mombello di Torino, Moncalieri, Montaldo Torinese, Moriondo Torinese, Nichelino, None, Osasco, Osasio, Pancalieri, Pavarolo, Pecetto Torinese, Perosa Argentina, Perrero, Pinasca, Pinerolo, Pino Torinese, Piobesi Torinese, Piscina, Poirino, Pomaretto, -

Linea 299V Saluzzo - Villafranca Piemonte Tpl Extraurbano Linea 299T Villafranca Piemonte - Torino Citta' Metropolitana Di Torino
LINEA 299V SALUZZO - VILLAFRANCA PIEMONTE TPL EXTRAURBANO LINEA 299T VILLAFRANCA PIEMONTE - TORINO CITTA' METROPOLITANA DI TORINO IN VIGORE DAL 13 SETTEMBRE 2021 299V SALUZZO > VILLAFRANCA PIEMONTE CORSA 1 19 37 55 73 85 97 109 121 139 151 163 169 181 193 205 217 229 DOMENICA E FESTIVI INFRASETTIMANALI ■ ■ ■ ■ SABATO ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A DA LUNEDÌ A VENERDÌ ❏ -2A ❏ -2A ■ ❏ -4A ❏ -2A ❏ -4A ❏ -2A ■ ❏ -2A ❏ -2A ■ x ❏ -2A ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A N. fer NOTA 1 6 6 6160 SALUZZO / Stazione FS 13.55 1 SALUZZO / Autostazione 05.40 06.15 06.55 07.25 07.55 08.25 09.25 11.25 12.35 13.05 14.03 14.00 15.05 16.25 17.25 18.25 20.15 6163 SALUZZO / S. Agostino 13.06 14.04 14.01 16.26 17.26 6062 CARDE' / Corso Vittorio Emanuele II 04.25 05.50 06.25 07.05 07.35 08.05 08.35 09.35 11.35 12.45 13.18 14.16 14.13 15.15 16.38 17.38 18.35 20.25 6064 VILLAFRANCA / Scuole (arrivo) 04.33 05.59 06.34 07.14 07.44 08.14 08.44 09.44 11.45 12.54 13.27 14.24 14.22 15.24 16.47 17.47 18.44 20.33 299T VILLAFRANCA PIEMONTE > TORINO CORSA 7 9 13 260103 25 31 43 49 61 67 79 91 103 115 127 133 145 157 163 175 187 199 211 223 235 229 DOMENICA E FESTIVI INFRASETTIMANALI ■ ■ ■ ■ SABATO ❏ -2A ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A ■ ❏ -4A ❏ -2A ■ ❏ -2A ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A DA LUNEDÌ A VENERDÌ ❏ -2A ❏ -4A ❏ -4A ❏ -2A ❏ -2A ❏ -4A ■ ❏ -4A ❏ -4A ❏ -2A ❏ -2A ❏ -4A ❏ -2A ■ ❏ -4A ❏ -4A ❏ -2A ■ x ❏ -2A ❏ -2A ❏ -2A ■ ❏ -2A ❏ -2A ❏ -2A N. -

Tariffe Trasporti Sanitari in Vigore Dal 15/09/2020 Vettura / Doblo'/ Pullmino Con Un Solo Volontario C.R.I
TARIFFE TRASPORTI SANITARI IN VIGORE DAL 15/09/2020 VETTURA / DOBLO'/ PULLMINO CON UN SOLO VOLONTARIO C.R.I. LUOGO DI DESTINAZIONE ANDATA E SOLO SOSTA PRESA RITORNO ANDATA GIAVENO, ENTRO I COAZZE, H GIAVENO 20 KM €23,00 €23,00 €7,00/ora VALGIOIE TRANA, AVIGLIANA, H GIAVENO ENTRO I €30,00 €30,00 SANGANO, 30 KM €7,00/ora REANO GIAVENO, COAZZE, VALGIOIE, H AVIGLIANA ENTRO I €30,00 €30,00 €7,00/ora TRANA, 30KM SANGANO, REANO, AVIGLIANA H RIVOLI/ ALTRE COAZZE, DESTINAZIONI ENTRO I 65 €60,00 €50,00 €7,00/ora VALGIOIE NEL COMUNE DI KM RIVOLI GIAVENO, TRANA, AVIGLIANA, H RIVOLI/ ALTRE SANGANO, DESTINAZIONI ENTRO I 45 €7,00/ora €40,00 €40,00 REANO, NEL COMUNE DI KM VILLARBASSE, RIVOLI RIVOLI RIVALTA BRUINO H RIVOLI/ ALTRE ALPIGNANO DESTINAZIONI ENTRO I 52 €50,00 €43,00 €7,00/ora SELVAGGIO NEL COMUNE DI KM RIVOLI H RIVOLI/ ALTRE RUBIANA DESTINAZIONI ENTRO 80 KM € 75,00 € 60,00 €7,00/ora NEL COMUNE DI RIVOLI LUOGO DI DESTINAZIONE ANDATA E SOLO SOSTA PRESA RITORNO ANDATA H CANDIOLO/ H SAN LUIGI/ COAZZE, ALTRE ENTRO I 75 €70,00 €60,00 €7,00/ora VALGIOIE DESTINAZIONI KM NEL COMUNE DI ORBASSANO GIAVENO, H CANDIOLO/ TRANA, H SAN LUIGI/ AVIGLIANA, ALTRE ENTRO I 50 €50,00 €50,00 SANGANO, DESTINAZIONI KM €7,00/ora REANO, NEL COMUNE DI VILLARBASSE, ORBASSANO BRUINO RIVALTA H CANDIOLO/ H SAN LUIGI/ SELVAGGIO ALTRE ENTRO I 63 €60,00 €53,00 €7,00/ora DESTINAZIONI KM NEL COMUNE DI ORBASSANO TUTTE LE COAZZE DESTINAZIONI ENTRO I 90 € 80,00 € 70,00 €7,00/ora VALGIOIE NEL COMUNE DI KM PIANEZZA GIAVENO AVIGLIANA TRANA TUTTE LE ROSTA DESTINAZIONI ENTRO I 65 € 60,00 -

Vaccinazioni
VACCINAZIONI Il Servizio di Igiene e Sanità Pubblica del Dipartimento di Prevenzione si occupa della prevenzione e controllo delle malattie infettive e diffusive ed effettua vaccinazioni nazionali e internazionali, pediatriche e per adulti. VACCINAZIONI DEI BAMBINI E DEGLI ADOLESCENTI A partire dal 2010 è stata introdotta in Piemonte l’offerta gratuita di nuovi vaccini sia per i bambini che per gli adolescenti. I vaccini prioritari per i quali è prevista l’offerta gratuita con invito sono: vaccino anti polio, tetano, difterite, pertosse, epatite B, haemophilus influenzae B, morbillo, rosolia, parotite, peumococco per i nuovi nati, meningococco nel 2° anno di vita e per gli adolescenti nel 16° anno di età, papilloma virus per le adolescenti nel 12° e 16° anno di età. Per i bambini affetti da particolari patologie che li espongono a rischio di complicanze, sono raccomandate vaccinazioni particolari. E’ compito del pediatra di famiglia consigliare e segnalare le vaccinazioni più opportune. Sono inoltre offerti gratuitamente i vaccini per i bambini e gli adolescenti che si recano in zone del mondo dove particolari malattie, scomparse in Piemonte, sono ancora presenti. COME Per i vaccini la famiglia di ogni nuovo nato riceve una lettera dell’ASL con l’invito a recarsi presso i Servizi vaccinali per la somministrazione. Al momento della prima dose viene rilasciato un certificato, aggiornato in tempo reale, con le indicazioni per i successivi richiami. Per gli altri vaccini è opportuno rivolgersi al pediatra di libera scelta, per avere informazioni -
D.T3.1.3. Fua-Level Self- Assessments on Background Conditions Related To
D.T3.1.3. FUA-LEVEL SELF- ASSESSMENTS ON BACKGROUND CONDITIONS RELATED TO CIRCULAR WATER USE Version 1 Turin FUA 02/2020 Sommario A.CLIMATE,ENVIRONMENT AND POPULATION ............................................... 3 A1) POPULATION ........................................................................................ 3 A2) CLIMATE ............................................................................................. 4 A3) SEALING SOIL ...................................................................................... 6 A4) GREEN SPACES IN URBANIZED AREAS ...................................................... 9 B. WATER RESOURCES ............................................................................ 11 B1) ANNUAL PRECIPITATION ...................................................................... 11 B2) RIVER, CHANNELS AND LAKES ............................................................... 13 B3) GROUND WATER .................................................................................. 15 C. INFRASTRUCTURES ............................................................................. 17 C1) WATER DISTRIBUTION SYSTEM - POPULATION WITH ACCESS TO FRESH WATER .................................................................................................... 17 C2) WATER DISTRIBUTION SYSTEM LOSS ..................................................... 18 C3) DUAL WATER DISTRIBUTION SYSTEM ..................................................... 18 C4) FIRST FLUSH RAINWATER COLLECTION ................................................ -

Convenzione Croce Rossa
PROVINCIA DI TORINO COMUNE DI VILLAR FOCCHIARDO Via Conte Carroccio, 30 Tel. 0119645025 – 0119646547 - Fax 011/9646283 e-mail: [email protected] [email protected] Partita I.V.A. : 01375740014 CONVENZIONE TRA IL COMUNE DI VILLAR FOCCHIARDO E LA CROCE ROSSA ITALIANA – UNITA’ LOCALE DI VILLAR DORA PER IL SERVIZIO DI ACCOMPAGNAMENTO E TRASPORTO SANITARIO DI UTENTI RESIDENTI ED INSERITI NELLA CATEGORIA AGEVOLATA. TRA Il Comune di Villar Focchiardo, P.I. 01375740014 rappresentato dal Sindaco FRANCO Luigi, domiciliato ai fini della presente Convenzione in Via Conte Carroccio n. 30 – Villar Focchiardo E La Croce Rossa Italiana – Unità Locale di Villar Dora, rappresentata dal Responsabile del Comitato Locale di Villar Dora Sig. FAVARIO Mauro; SI CONVIENE E SI STIPULA QUANTO SEGUE Il Comune di Villar Focchiardo intende offrire un servizio di accompagnamento e trasporto “sanitario” ai propri cittadini bisognosi di cure e/o visite mediche, disciplinato come segue: 1) Possono beneficiare del servizio coloro che, trovandosi in una delle categorie sotto elencate, abbiano i requisiti previsti dall’art. 16 del vigente regolamento comunale per la disciplina della concessione di sovvenzioni, contributi, sussidi ed ausili finanziari (ISEE): - pazienti che sono in possesso di esenzione ticket per indigenza; - pazienti che sono in possesso di esenzione ticket per patologia, per i trasporti per cure e/o visite mediche inerenti la patologia; - invalidi di guerra, invalidi del lavoro, invalidi per servizio, ciechi civili e sordomuti; - invalidi civili totali con diritto all’indennità di accompagnamento (100% di invalidità) e portatori di handicap certificato ai sensi dell’art. 4 della Legge n.104/1992. -

Dipartimenti Di Prevenzione Delle ASL Della Regione Piemonte Ambito Territoriale (Comuni)
Dipartimenti di prevenzione delle ASL della Regione Piemonte Ambito territoriale (comuni) 1 ASL Ambito territoriale ASL Città di Torino Torino Almese, Avigliana, Bardonecchia, Beinasco, Borgone Susa, Bruino, Bruzolo, Bussoleno, Buttigliera Alta, Caprie, Caselette, Cesana Torinese, Chianocco, Chiomonte, Chiusa di San Michele, Claviere, Coazze, Collegno, Condove, Exilles, Giaglione, Giaveno, Gravere, Grugliasco, Mattie, Meana di Susa, Mompantero, Moncenisio, Novalesa, Orbassano, Oulx, Piossasco, Reano, Rivalta di Torino, Rivoli, Rosta, Rubiana, Salbertrand, San Didero, San Giorio di Susa, Sangano, Sant’ambrogio di Torino, Sant’Antonino di Susa, Sauze di Cesana, Sauze d’Oulx, Susa, Trana, Vaie, Valgioie, Venaus, Villar Dora, Villar Focchiardo, Villarbasse, Volvera, Alpignano, Druento, ASL TO3 Givoletto, La Cassa, Pianezza, San Gillio, Val della Torre, Venaria Reale, Airasca, Angrogna, Bibiana, Bobbio Pellice, Bricherasio, Buriasco, Campiglione Fenile, Cantalupa, Cavour, Cercenasco, Cumiana, Fenestrelle, Frossasco, Garzigliana, Inverso Pinasca, Luserna San Giovanni, Lusernetta, Macello, Massello, Osasco, Perosa Argentina, Perrero, Pinasca, Pinerolo, Piscina, Pomaretto, Porte, Pragelato, Prali, Pramollo, Prarostino, Roletto, Rorà, Roure, Salza di Pinerolo, San Germano Chisone, San Pietro Val Lemina, San Secondo di Pinerolo, Scalenghe, Sestriere, Torre Pellice, Usseaux, Vigone, Villafranca Piemonte, Villar Pellice, Villar Perosa, Virle Piemonte. Ala di Stura, Balangero, Balme, Barbania, Borgaro Torinese, Cafasse, Cantoira, Caselle Torinese,