The Urinary System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Female Urethra
OBJECTIVES: • By the end of this lecture, student should understand the anatomical structure of urinary system. General Information Waste products of metabolism are toxic (CO2, ammonia, etc.) Removal from tissues by blood and lymph Removal from blood by Respiratory system And Urinary system Functions of the Urinary System Elimination of waste products Nitrogenous wastes Toxins Drugs Functions of the Urinary System Regulate homeostasis Water balance Acid-base balance in the blood Electrolytes Blood pressure Organs of the Urinary system Kidneys Ureters Urinary bladder Urethra Kidneys Primary organs of the urinary system Located between the 12th thoracic and 3rd lumbar vertebrae. Right is usually lower due to liver. Held in place by connective tissue [renal fascia] and surrounded by thick layer of adipose [perirenal fat] Each kidney is approx. 3 cm thick, 6 cm wide and 12 cm long Regions of the Kidney Renal cortex: outer region Renal medulla: pyramids and columns Renal pelvis: collecting system Kidneys protected by three connective tissue layers Renal fascia -Attaches to abdominal wall Renal capsule: -Surrounds each kidney -Fibrous sac -Protects from trauma and infection Adipose capsule -Fat cushioning kidney Nephrons Each kidney contains over a million nephrons [functional structure] • Blood enters the nephron from a network that begins with the renal artery. • This artery branches into smaller and smaller vessels and enters each nephron as an afferent arteriole. • The afferent arteriole ends in a specialized capillary called the Glomerulus. • Each kidney has a glomerulus contained in Bowman’s Capsule. • Any cells that are too large to pass into the nephron are returned to the venous blood supply via the efferent arteriole. -

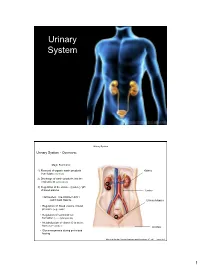
Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -

Kidney in an Effort to Aid Health Information Management Coding Professionals for ICD-10, the Following Anatomy Tip Is Provided with an Educational Intent
Anatomy Tip Kidney In an effort to aid Health Information Management Coding Professionals for ICD-10, the following anatomy tip is provided with an educational intent. The kidneys are the main part of the urinary system and are a pair of organs; right and left; located in the back of the abdomen. Each kidney is about 4 or 5 inches long. • The kidneys are surrounded by three layers of tissue: • The renal fascia is a thin, outer layer of fibrous connective tissue that surrounds each kidney (and the attached adrenal gland) and fastens it to surrounding structures. • The adipose capsule is a middle layer of adipose (fat) tissue that cushions the kidneys. • The renal capsule is an inner fibrous membrane that prevents the entrance of infections. • There are three major regions inside the kidney: • The renal cortex borders the convex side. • The renal medulla lies adjacent to the renal cortex. It consists of striated, cone-shaped regions called renal pyramids (medullary pyramids), whose peaks, called renal papillae, face inward. The unstriated regions between the renal pyramids are called renal columns. • The renal sinus is a cavity that lies adjacent to the renal medulla. The other side of the renal sinus, bordering the concave surface of the kidney, opens to the outside through the renal hilus. The ureter, nerves, and blood and lymphatic vessels enter the kidney on the concave surface through the renal hilus. The renal sinus houses the renal pelvis, a funnel-shaped structure that merges with the ureter. • All the blood in our bodies passes through the kidneys several times a day. -

Laparoscopic Colectomy for a Patient with Congenital Renal Agenesis
[Downloaded free from http://www.jstcr.org on Monday, October 07, 2013, IP: 41.135.175.93] || Click here to download free Android application for this journal cASE REPORt Laparoscopic Colectomy for a Patient with Congenital Renal Agenesis Hiroyuki Tanishima, Tetsuya Horiuchi, Yoshiharu Shono, Masamichi Kimura Department of Surgery, National Hospital Organization, ABSTRACT Osaka Minami Medical Center, Osaka, Japan We present a very rare case of laparoscopic colectomy for a patient with ascending colon cancer and an agenetic INTRODUCTION right kidney. A 57-year-old man visited our institute for further evaluation for a positive fecal occult blood test. ongenital unilateral renal agenesis is a rare Approximately, 20 years earlier, the right kidney of the patient condition. In patients with the congenital absence was found to be congenitally absent. A physical examination indicated no anatomical anomalies in his genitourinary [1] Cof the kidney, the renal fascia is also absent. Here, system, and the renal function was within the normal range. for the first time, we report the case of a patient with Total colonoscopy revealed a cancer of the ascending cancer of the ascending colon and right renal agenesis who colon and laparoscopic colectomy was performed. The was treated by laparoscopic colectomy, and discussed the right colon was mobilized by lateral-to-medial extension of a retroperitoneal dissection between the fusion fascia and presence of the anterior renal fascia in such cases based on the anterior renal fascia. The right testicular vessels were our experience and from a review of the literature. preserved without injury to the anterior renal fascia; however, the right ureter could not be detected. -
Urinary System
Urinary System Urinary System Urinary System - Overview: Major Functions: 1) Removal of organic waste products Kidney from fluids (excretion) 2) Discharge of waste products into the environment (elimination) 1 3) Regulation of the volume / [solute] / pH 3 of blood plasma Ureter HOWEVER, THE KIDNEY AIN’T JUST FOR PEE’IN… Urinary bladder • Regulation of blood volume / blood pressure (e.g., renin) • Regulation of red blood cell formation (i.e., erythropoietin) 2 • Metabolization of vitamin D to active form (Ca++ uptake) Urethra • Gluconeogenesis during prolonged fasting Marieb & Hoehn (Human Anatomy and Physiology, 8th ed.) – Figure 25.1 1 Urinary System Renal ptosis: Kidneys drop to lower position due Functional Anatomy - Kidney: to loss of perirenal fat Located in the superior lumbar “Bar of soap” region 12 cm x 6 cm x 3 cm 150 g / kidney Layers of Supportive Tissue: Renal fascia: Peritoneal cavity Outer layer of dense fibrous connective tissue; anchors kidney in place Perirenal fat capsule: Fatty mass surrounding kidney; cushions kidney against blows Fibrous capsule: Transparent capsule on kidney; prevents infection of kidney from local tissues Kidneys are located retroperitoneal Marieb & Hoehn (Human Anatomy and Physiology, 8th ed.) – Figure 25.2 Urinary System Functional Anatomy - Kidney: Pyelonephritis: Inflammation of the kidney Pyramids appear striped due to parallel arrangement of capillaries / collecting tubes Renal cortex Renal medulla Renal pyramids Renal papilla Renal columns Renal hilum Renal pelvis • Entrance for blood vessels -

Gross Anatomy of the Lungs
GROSS ANATOMY OF KIDNEY, URETER AND SUPRA RENAL GLAND Professor Dr. Mario Edgar Fernández. Kidneys: Gross Anatomy Lie in retroperitoneal, superior lumbar region Extend from T11 or T12 to L3 Laterally convex, medially concave Hilus Where blood vessels, ureters, and nerves enter and leave kidney Adrenal gland On superior portion Kidney: Gross Anatomy Lateral margin. Convex. Medial margin. Concave at the hilum. Renal hilum. Site of entry and exit of blood vessels & ureter. Renal sinus. Cavity at the medial border for the renal hilum. Anterior surface. Facies anterior. Curved. Posterior surface. Facies posterior. Nearly flat. Upper pole. Extremitas superior Lower pole. Extre,itas inferior Projections Kidneys: Gross and Sectional Anatomy Right kidney ~ 2cm lower than left Adrenal gland on superior pole KIDNEYS Its main function is to excrete most of the waste products of metabolism It control the water and electrolyte balance of the body It maintain acid-base balance of the blood The waste products leave the kidneys as urine, which passes down the ureters to the urinary bladder The urine leaves the body through the urethra KIDNEYS Kidneys are reddish brown in color Lie behind the peritoneum of the posterior abdominal wall It lie high up on either side of the vertebral column Are largely under cover of the costal margin The right kidney lies slightly lower than the left due to the large size of right lobe of the liver With contraction of the diaphragm during respiration, KIDNEYS both kidneys move downward in a vertical direction -

Anatomy of the Kidney
Anatomy of the kidney Renal block-Anatomy-Lecture 1 Editing file Color guide : Only in boys slides in Green Objectives Only in girls slides in Purple important in Red Notes in Grey By the end of this course you should be able to discuss : ● Components of the urinary system ● Kidney : 1. Shape & Position 2. Surface anatomy 3. External features 4. Hilum & its contents 5. Relation 6. Internal features 7. Blood supply 8. Lymph drainage 9. Nerve supply Introduction 3 ● Every day, each kidney filters liters (around 150 L per day ) of fluid from the bloodstream. ● Although the lungs and the skin also play roles in excretion, The kidneys bear the major responsibility for eliminating nitrogenous (nitrogen-containing) wastes, toxins, and drugs from the body. Excretes most of the Maintain acid-base waste products of balance of the blood. metabolism. By Erythropoietin Controls hormone stimulates Function of water & electrolyte bone marrow for RBCs kidney balance of the body. formation. Converts By Rennin vitamin D to its enzyme regulates active form. the blood pressure. The kidney : ● Kidneys are reddish brown in color. 4 ● Lie behind the peritoneum (retroperitoneal) on the posterior abdominal wall on either side of the vertebral column. ● They are largely under cover of the costal margin. kidney lies between T12-L3 ● With contraction of the diaphragm (during inspiration) the kidney moves downward as much as 2.5 cm. T12 Comparison between : L3 Right kidney Left kidney Anterior view lies slightly lower than the left due Location to the large size of the right lobe of Upper than the right the liver. -

URINARY SYSTEM Components
Human Anatomy Unit 3 URINARY SYSTEM Components • Kidneys • Ureters • Urinary bladder • Urethra Funcons • Storage of urine – Bladder stores up to 1 L of urine • Excreon of urine – Transport of urine out of body • Regulaon: – Plasma pH – Blood volume/pressure – Plasma ion concentraons (Ca2+, Na+, K+, CL-) – Assist liver in detoxificaon, amino acid metabolism Kidney Gross Anatomy • Retroperitoneal – Anterior surface covered with peritoneum – Posterior surface directly against posterior abdominal wall • Superior surface at about T12 • Inferior surface at about L3 • Ureters enter urinary bladder posteriorly • LeT kidney 2cm superior to right – Size of liver Structure of the Kidney • Hilum = the depression along the medial border through which several structures pass – renal artery – renal vein – ureter – renal nerves Surrounding Tissue • Fibrous capsule – Innermost layer of dense irregular CT – Maintains shape, protec:on • Adipose capsule – Adipose ct of varying thickness – Cushioning and insulaon • Renal fascia – Dense irregular CT – Anchors kidney to peritoneum & abdominal wall • Paranephric fat – Outermost, adipose CT between renal fascia and peritoneum Frontal Sec:on of the Kidney • Cortex – Layer of renal :ssue in contact with capsule – Renal columns – parts of cortex that extend into the medulla between pyramids • Medulla – Striped due to renal tubules • Renal pyramids – 8-15 present in medulla of adult – Conical shape – Wide base at cor:comedullary juncon Flow of Filtrate/Urine • Collec:ng ducts – Collect from mul:ple nephrons • Minor calyx – Collect from each pyramid • Major calyx – Collect from minor calyx • Renal pelvis – Collects from calyces, passes onto • Ureter – Collects from pelvis • Urinary Bladder – Collects from ureters Histology Renal Cortex Renal Medulla Renal Tubules • Nephron – func:onal unit of the kidney. -
Introduction to the Urinary System
Tips for Success 1. Show up 2. Participate in lab 3. Show up 4. Turn in assignments (completed, refer to #6) 5. Show up 6. Communicate with me, e-mail is best 7. Show up Every point counts! Business Homework due in lab Label the handout provided today Front and back Use your book! There should be at least 18 items labeled Part 1 Urinary System Wastes Gases versus fluids Urinary system Dispose of water soluble wastes Electrolyte regulation Acid-base regulation Urinary System Other functions Kidneys Renin Erythropoietin Vitamin D activation Nitrogenous Wastes Urine is about 95% water Second largest component is urea Urea derived from breakdown of amino acids Nitrogenous Wastes TOXIC! + 1. Dietary amino acids → NH2 removed → NH2 + H → NH3 500 ml of urine removes only 1 gram of nitrogen as ammonia 2. Ammonia can be converted to urea Requires energy 50 ml of urine removes 1 gram of nitrogen as urea 3. Ammonia can be converted to uric acid Requires lots of energy 10 ml of urine removes 1 gram of nitrogen as uric acid Urinary System Organs Kidneys Major excretory organs Urinary bladder Temporary storage reservoir for urine Ureters Transport urine from the kidneys to the bladder Urethra Transports urine out of the body Hepatic veins (cut) Esophagus (cut) Inferior vena cava Renal artery Adrenal gland Renal hilum Aorta Renal vein Kidney Iliac crest Ureter Rectum (cut) Uterus (part of female reproductive Urinary system) bladder Urethra Figure 25.1 Kidney: Urinary System page 6 Anterior Inferior vena cava Peritoneal -
Lecture (1) Urinary System
UrinaryUrinaryUrinary systemsystemsystem Dr. Carmen E. Rexach Anatomy 35 Mt. San Antonio College Functions •Storage of urine – Bladder stores up to 1 L of urine • Excretion of urine – Transport of urine out of body • Blood volume regulation – Effects of hormones on kidneys • Regulation of erythrocyte production –Kidneys • Monitor oxygen content of blood • Produce EPO = erthrocyte production Components •Kidneys • Ureters • Urinary Bladder • Urethra Kidneys Gross Anatomy • Kidneys approx weight = 125- 150g each • Retroperitoneal – Anterior surface covered with peritoneum – Posterior surface directly against posterior abdominal wall • Superior surface at about T12 • Inferior surface at about L3 • ureters enter urinary bladder posteriorly • Left kidney 2cm superior to right –Size of liver Transverse section at L1 surface features of kidney • Hilum = the depression along the medial border through which several structures pass –renal artery –renal vein –ureter – renal nerves Surrounding structures • Fibrous capsule – Innermost layer of dense irregular CT – Maintains shape, protection • Adipose capsule (perinephric fat) – Adipose ct of varying thickness – Cushioning and insulation • Renal fascia – Dense irregular CT – Anchors kidney to peritoneum & abdominal wall • Paranephric fat – Outermost, adipose CT between renal fascia and peritoneum Coronal section •Cortex – layer of renal tissue in contact with capsule –Lighter shade –Renal columns= parts of cortex that extend into the medulla between pyramids •Medulla –Innermost – striped due to renal tubules •renal pyramids – 8-15 present in medulla of adult – conical shape – Wide base at corticomedullary junction Coronal section • Renal pelvis – collects from calyces, passes onto ureter •Calyces (pl) – funnel shaped regions – collect urine into pelvis •Minor calyx (s) – in contact with each pyramid •Major calyx (s) – collect from minor Microscopic Anatomy Microscopic anatomy Renal tubules • Nephron – functional unit of the kidney. -

The Urinary System Consists of Kidneys, Ureters, Urinary Bladder
Anatomy Lecture Notes Chapter 23 the urinary system consists of kidneys, ureters, urinary bladder, and urethra the function of the kidneys is NOT "to make urine" the kidneys: 1) regulate water balance 2) regular ECF electrolyte levels (Na, K, Ca) 3) eliminate some metabolic wastes urine is a by-product of these functions A. kidneys 1. located against posterior abdominal wall (retroperitoneal) T11 or T12 to L3 right kidney lower than left kidney 2. surrounded by a. pararenal fat (posterior only) b. renal fascia c. adipose capsule - perirenal fat d. renal capsule - dense c.t. covering surface of kidney e. parietal peritoneum Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 3. layers a. cortex - contains renal corpuscles and extends inwards as renal columns b. medulla - consists of renal pyramids which consist mostly of collecting ducts papilla - apex of renal pyramid; where collecting ducts drain into calyx 4. cavities and associated structures a. renal sinus - space in medial part of kidney; contains renal pelvis b. renal pelvis - expanded superior part of ureter minor calyx collects urine from one renal papilla major calyx formed by junction of 2 or more minor calyces renal pelvis formed by junction of all major calyces Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 5. renal hilum - medial indentation; where ureter leaves kidney 6. blood flow through the kidney - renal fraction = 20% of cardiac output aorta renal artery segmental arteries lobar arteries interlobar arteries arcuate arteries cortical radiate (interlobular) arteries afferent arterioles glomerular capillaries (glomerulus) efferent arteriole peritubular capillaries and vasa recta cortical radiate (interlobular) veins arcuate veins interlobar veins renal vein inferior vena cava Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 7. -

ANATOMY Urinary System
ANATOMY Urinary system 1st Prof Pharm.D Urinary system Composition of urinary system: The urinary system consists of ❑ two kidneys, ❑two ureters, ❑the urinary bladder, ❑the urethra. Kidneys Kidneys are paired, reddish, bean–shaped organs responsible for formation of urine by blood filtration Location Kidneys are positioned against the posterior wall of the abdominal cavity (retroperitoneal) between the levels of the twelfth thoracic and the third lumbar vertebrae The right kidney is usually 1.5 to 2.0 cm lower than the left because of the large area occupied by the liver on the right side. External anatomy of kidneys Each adult kidney is a bean-shaped organ about 11.25 cm (4 in.) long, 5.5 to 7.7 cm (2–3 in.) wide, and 2.5 cm (1 in.) thick. Each kidney is embedded in a fatty fibrous pouch consisting of three layers: ❑ The renal capsule - layer of dense fibrous connective tissue surrounding each kidney, protects kidney from trauma and infection and maintain its shape ❑ Renal adipose capsule – layer of adipose tissue surrounding the renal capsule functions as a shock absorber, cushioning the kidneys against mechanical shock. ❑ Renal fascia - thin layer of connective tissue surrounding the adipose tissue, anchors the kidney to the posterior abdominal wall * The lateral border of each kidney is convex, whereas the medial border is strongly concave * On the medial border is hilum, a depression through which renal artery, vein and nerves enter and leave kidney * The superior border of each kidney is capped by the adrenal gland Internal anatomy of kidneys The coronal section of the kidney show two distinct regions and a cavity.