In Mauritania
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
FEWS Country Report BURKINA, CHAD, MALI, MAURITANIA, and NIGER
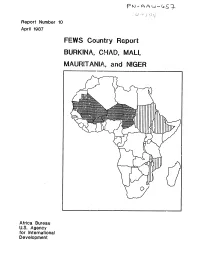
Report Number 10 April 1987 FEWS Country Report BURKINA, CHAD, MALI, MAURITANIA, and NIGER Africa Bureau U.S. Agency for International Development Summary Map __ Chad lMurltanl fL People displaced by fighting High percentage of population have bothL.J in B.E.T. un~tfood needsa nd no source of income - High crop oss cobied with WESTERN Definite increases in retes of malnutrition at CRS centers :rom scarce mrket and low SAHARA .ct 1985 through Nov 196 ,cash income Areas with high percentage MA RTAI of vulnerable LIBYA MAU~lAN~A/populations / ,,NIGER SENEGAL %.t'"S-"X UIDA Areas at-risk I/TGI IEI BurkinaCAMEROON Areas where grasshoppers r Less than 50z of food needs met combined / CENTRAL AFRICAN would have worst impact Fi with absence of government stocks REPLTL IC if expected irdestat ions occur W Less than r59 of food needs met combined ith absence of government stocks FEYIS/PWA. April 1987 Famine Early Warning System Country Report BURKINA CHAD MALI MAURITANIA NIGER Populations Under Duress Prepared for the Africa Bureau of the U.S. Agency for International Development Prepared by Price, Williams & Associates, Inc. April 1987 Contents Page i Introduction 1 Summary 2 Burkina 6 Chad 9 Mali 12 Mauritania 18 Niger 2f FiAures 3 Map 2 Burkina, Grain Supply and OFNACER Stocks 4 Table I Burkina, Production and OFNACER Stocks 6 Figure I Chad, Prices of Staple Grains in N'Djamcna 7 Map 3 Chad, Populations At-Risk 10 Table 2 Mali, Free Food Distribution Plan for 1987 II Map 4 Mali, Population to Receive Food Aid 12 Figure 2 Mauritania, Decreasing -

The World Bank
Document of The World Bank Public Disclosure Authorized Report No: ICR00002788 IMPLEMENTATION COMPLETION AND RESULTS REPORT (IDA-38100, IDA-38101, IDA-3810A and IDA-49330) ON A Public Disclosure Authorized CREDIT IN THE AMOUNT OF SDR21.1 MILLION (US$32.15 MILLION EQUIVALENT) TO THE ISLAMIC REPUBLIC OF MAURITANIA FOR A Public Disclosure Authorized SECOND MINING SECTOR CAPACITY BUILDING PROJECT June 13, 2014 Public Disclosure Authorized Sustainable Energy, Oil, Gas, and Mining Unit Sustainable Development Network AFCF1 Africa Region CURRENCY EQUIVALENTS (Exchange Rate Effective May 15, 2014) Currency Unit = Mauritania Ouguiya (MRO) MRO 1.00 = US$ 0.0034 US$ 1.00 = MRO 298 FISCAL YEAR July 1 – June 30 ABBREVIATIONS AND ACRONYMS Bpd Barrels per day CAS Country Assistance Strategy CNITIE Comité National de l’Initiative pour la Transparence dans les Industries Extractives CNRE Centre National des Ressources en Eau CPPR Country Portfolio Performance Review DMG Direction des Mines et de la Géologie EI Extractive Industries EITI Extractive Industries Transparency Initiative GIRM Government of the Islamic Republic of Mauritania GIZ Gesellschaft fur Internationale Zusammenarbeit ICR Implementation Completion Report IDA International Development Association IDB Islamic Development Bank LED Local Economic Development IMF International Monetary Fund M&E Monitoring and evaluation MMI Ministère des Mines et de l’Industrie MPEM Ministère du Pétrole, de l’Energie et des Mines NORAD Norwegian Agency for development Cooperation PAD Project Appraisal Document -

Chapter 5 Formulation of Action Plan and Model for Gorgol Region
The Development Study for the Project on Revitalization of Irrigated Agriculture in the Irrigated Zone of Foum Gleita in the Islamic Republic of Mauritania Main Report CHAPTER 5 FORMULATION OF ACTION PLAN AND MODEL FOR GORGOL REGION 5.1 Issues of the Foum Gleita Project Area 5.1.1 Analysis of the History of the Foum Gleita Project The important events in Foum Gleita are reviewed to define the background of problems. However, the operation for the entire area has started about 20 years ago in 1990, and hence SONADER no longer possessed the documents of this period, and neither did the farmers. The information was fragmentary, and often the time of the events was not well defined and the description given by the farmers was different from each other. These issues were complicated, and it was difficult to ascertain the veracity of the facts. Based on these conditions, the Fig. 5.1.1 was prepared, and the chronological table on the left shows important events related to Foum Gleita and the figure on the right shows an image between necessary inputs for irrigated agriculture and cropping areas as its results. Actually, the problems of Foum Gleita were attributed to the fact that the scope of management and maintenance for mid and long term was not sufficient, and the farmers and the government did not play their roles. Then the problems were accumulated, while both of them do nothing. The figure 5.1.1 shows the real situation of Foum Gleita (left in red) and the idealistic responsibility and results (right in blue). -

Pdf | 94.29 Kb
ALERT LEVEL: MAURITANIA NO ALERT Monthly Food Security Update WATCH WARNING December 2006 EMERGENCY Conditions are normal, with pockets of food insecurity CONTENT Summary and implications Summary and implications ....1 As the last late-planted rain fed sorghum crops are harvested, cereal yield estimates indicate a Current hazards summary.....1 decrease from last year due to this year’s shorter than usual rainy season and damages from grain- Status of crops ......................1 eating birds during the heading stage of their growing cycle. Rice harvests are still in progress and Conditions in stock-raising most flood-recession crops have been planted. However, farmers did not plant flood recession crops areas .....................................2 in many areas of Gorgol region, due to fear of infestations of pink stalk borers, straying animals and Locust situation .....................2 pressure from grain-eating birds. While the locust situation remains calm, heavy pressure on off- season crops from grain-eating birds continue, despite large-scale control programs. Food security.........................2 Recommendations ................2 Conditions in the pastoral areas of central Mauritania (northern Brakna, northern Gorgol, central Trarza and Assaba) are beginning to deteriorate as a result of overgrazing and wind erosion. The pace of seasonal migration has picked up as herders and their animals search for better grazing lands and move closer to buyers in anticipation of the approaching Tabaski holiday (the Muslim Feast of Sacrifice). Supplies of sorghum and millet on grain markets remain limited, due largely to the shortfall in local production and the small volume of grain trade with Senegal. Transfers of Malian grain (from the 2004 and 2005 harvests) are picking up in border areas in the Southeast and in Nouakchott, keeping sorghum prices relatively stable, though prices on rural markets are trending upwards. -

Looters Vs. Traitors: the Muqawama (“Resistance”) Narrative, and Its Detractors, in Contemporary Mauritania Elemine Ould Mohamed Baba and Francisco Freire
Looters vs. Traitors: The Muqawama (“Resistance”) Narrative, and its Detractors, in Contemporary Mauritania Elemine Ould Mohamed Baba and Francisco Freire Abstract: Since 2012, when broadcasting licenses were granted to various private television and radio stations in Mauritania, the controversy around the Battle of Um Tounsi (and Mauritania’s colonial past more generally) has grown substantially. One of the results of this unprecedented level of media freedom has been the prop- agation of views defending the Mauritanian resistance (muqawama in Arabic) to French colonization. On the one hand, verbal and written accounts have emerged which paint certain groups and actors as French colonial power sympathizers. At the same time, various online publications have responded by seriously questioning the very existence of a structured resistance to colonization. This article, drawing pre- dominantly on local sources, highlights the importance of this controversy in study- ing the western Saharan region social model and its contemporary uses. African Studies Review, Volume 63, Number 2 (June 2020), pp. 258– 280 Elemine Ould Mohamed Baba is Professor of History and Sociolinguistics at the University of Nouakchott, Mauritania (Ph.D. University of Provence (Aix- Marseille I); Fulbright Scholar resident at Northwestern University 2012–2013), and a Senior Research Consultant at the CAPSAHARA project (ERC-2016- StG-716467). E-mail: [email protected] Francisco Freire is an Anthropologist (Ph.D. Universidade Nova de Lisboa 2009) at CRIA–NOVA FCSH (Lisbon, Portugal). He is the Principal Investigator of the European Research Council funded project CAPSAHARA: Critical Approaches to Politics, Social Activism and Islamic Militancy in the Western Saharan Region (ERC-2016-StG-716467). -

Pastoralism and Security in West Africa and the Sahel
Pastoralism and Security in West Africa and the Sahel Towards Peaceful Coexistence UNOWAS STUDY 1 2 Pastoralism and Security in West Africa and the Sahel Towards Peaceful Coexistence UNOWAS STUDY August 2018 3 4 TABLE OF CONTENTS Abbreviations p.8 Chapter 3: THE REPUBLIC OF MALI p.39-48 Acknowledgements p.9 Introduction Foreword p.10 a. Pastoralism and transhumance UNOWAS Mandate p.11 Pastoral Transhumance Methodology and Unit of Analysis of the b. Challenges facing pastoralists Study p.11 A weak state with institutional constraints Executive Summary p.12 Reduced access to pasture and water Introductionp.19 c. Security challenges and the causes and Pastoralism and Transhumance p.21 drivers of conflict Rebellion, terrorism, and the Malian state Chapter 1: BURKINA FASO p.23-30 Communal violence and farmer-herder Introduction conflicts a. Pastoralism, transhumance and d. Conflict prevention and resolution migration Recommendations b. Challenges facing pastoralists Loss of pasture land and blockage of Chapter 4: THE ISLAMIC REPUBLIC OF transhumance routes MAURITANIA p.49-57 Political (under-)representation and Introduction passivity a. Pastoralism and transhumance in Climate change and adaptation Mauritania Veterinary services b. Challenges facing pastoralists Education Water scarcity c. Security challenges and the causes and Shortages of pasture and animal feed in the drivers of conflict dry season Farmer-herder relations Challenges relating to cross-border Cattle rustling transhumance: The spread of terrorism to Burkina Faso Mauritania-Mali d. Conflict prevention and resolution Pastoralists and forest guards in Mali Recommendations Mauritania-Senegal c. Security challenges and the causes and Chapter 2: THE REPUBLIC OF GUINEA p.31- drivers of conflict 38 The terrorist threat Introduction Armed robbery a. -

2. Arrêté N°R2089/06/MIPT/DGCL/ Du 24 Août 2006 Fixant Le Nombre De Conseillers Au Niveau De Chaque Commune
2. Arrêté n°R2089/06/MIPT/DGCL/ du 24 août 2006 fixant le nombre de conseillers au niveau de chaque commune Article Premier: Le nombre de conseillers municipaux des deux cent seize (216) Communes de Mauritanie est fixé conformément aux indications du tableau en annexe. Article 2 : Sont abrogées toutes dispositions antérieures contraires, notamment celles relatives à l’arrêté n° 1011 du 06 Septembre 1990 fixant le nombre des conseillers des communes. Article 3 : Les Walis et les Hakems sont chargés, chacun en ce qui le concerne, de l’exécution du présent arrêté qui sera publié au Journal Officiel. Annexe N° dénomination nombre de conseillers H.Chargui 101 Nema 10101 Nema 19 10102 Achemim 15 10103 Jreif 15 10104 Bangou 17 10105 Hassi Atile 17 10106 Oum Avnadech 19 10107 Mabrouk 15 10108 Beribavat 15 10109 Noual 11 10110 Agoueinit 17 102 Amourj 10201 Amourj 17 10202 Adel Bagrou 21 10203 Bougadoum 21 103 Bassiknou 10301 Bassiknou 17 10302 El Megve 17 10303 Fassala - Nere 19 10304 Dhar 17 104 Djigueni 10401 Djiguenni 19 10402 MBROUK 2 17 10403 Feireni 17 10404 Beneamane 15 10405 Aoueinat Zbel 17 10406 Ghlig Ehel Boye 15 Recueil des Textes 2017/DGCT avec l’appui de la Coopération française 81 10407 Ksar El Barka 17 105 Timbedra 10501 Timbedra 19 10502 Twil 19 10503 Koumbi Saleh 17 10504 Bousteila 19 10505 Hassi M'Hadi 19 106 Oualata 10601 Oualata 19 2 H.Gharbi 201 Aioun 20101 Aioun 19 20102 Oum Lahyadh 17 20103 Doueirare 17 20104 Ten Hemad 11 20105 N'saveni 17 20106 Beneamane 15 20107 Egjert 17 202 Tamchekett 20201 Tamchekett 11 20202 Radhi -

Senegal River Basin Health Master Plan Study
SENEGAL RIVER BASIN HEALTH MAETER PLAN STUDY WASH Field Report No. 453 December 1994 SANITATION fbr --- ~.rea+r.rr~fi PROJECT -- Sponsored by the U.S. Agency for International Development Operated by CDM and Associates WASH Field Report No. 453 Senegal River Basin Health Master Plan Study Prepared for the USAlD Mission to Senegal U. S. Agency for International Development under WASH Task No. 5 12 Mbarack Diop William R. Jobin with Nicolas G. Adrien Fereydoun Arfaa Judith Auk1 Sax& Bertoli-Minor Ralph W~~PP Jan Rozendaal December 1994 Water and Slnimtion for Hdth Project C-t No. DPJi-5973-Z4WO81-00, Project No. 936-5973 is sponsod by Me Bumu for Glow Programs, Field Suppoh and Resurch Offh of Hdth rad Nuaitibn U.S. Agency for IntennW Development Wdingmn, DC 20523 Senegal River Basin Health Master Plan Shady ERRATA P. xix, paragraph 6, line 1 : "The Senegal River rises in Guinea.." P. 21, paragraph 4, lines 4-5: "Giventhe decrease in midalls in the Lawer€.,c~..." P. 35, Current Findings/Epiderniological Survey, paragraph 2, line 1: "Inthe Delta, three schools on the Mauritanian bank of the river (Finuresand 14)..." - P. 57, Figure 20: Green line = St. Louis, red line = Dagana P. 68, fourth full paragraph, line 3: "...toallow fanners to harvest a normal crop and Figure 25)." !~ENEGALRIVHIBASMHEALTHMASLPZPLANST~Y CONTENTS ... Acknowledgements ............................................... xu1 Acronyms ...................................................... xv Preface ........................................................ xix ExecutiveSummary -

Distribution, Host Preference and Infection Rates of Malaria Vectors in Mauritania
Parasites & Vectors BioMed Central Short report Open Access Distribution, host preference and infection rates of malaria vectors in Mauritania Ibrahima Dia*1, Hampate Ba2, Sid Ahmed Ould Mohamed2, Diawo Diallo1, Baidy Lo2 and Mawlouth Diallo1 Address: 1Unité d'Entomologie Médicale, Institut Pasteur de Dakar, BP 220, Dakar, Senegal and 2Institut National de Recherches en Santé Publique, Nouakchott, Mauritania Email: Ibrahima Dia* - [email protected]; Hampate Ba - [email protected]; Sid Ahmed Ould Mohamed - [email protected]; Diawo Diallo - [email protected]; Baidy Lo - [email protected]; Mawlouth Diallo - [email protected] * Corresponding author Published: 4 December 2009 Received: 7 October 2009 Accepted: 4 December 2009 Parasites & Vectors 2009, 2:61 doi:10.1186/1756-3305-2-61 This article is available from: http://www.parasitesandvectors.com/content/2/1/61 © 2009 Dia et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract This study reports for the first time on the distribution, host preference and infection rates of malaria vectors in Mauritania. It was conducted during an outbreak of Rift valley fever. Three anopheline species were reported. An. arabiensis was the predominant species observed in all regions whereas An. pharoensis and An. funestus were observed along the south border in the Senegal River valley where extensive irrigation schemes are present. The distribution limits of anopheline species were observed from the Senegal River basin in the Trarza region up to the south limit of the Saharan desert in Tidjikja city. -

PIF) Entry – Full Sized Project – GEF - 7 Development of an Integrated System to Promote the Natural Capital in the Drylands of Mauritania
5/5/2020 WbgGefportal Project Identification Form (PIF) entry – Full Sized Project – GEF - 7 Development of an integrated system to promote the natural capital in the drylands of Mauritania Part I: Project Information GEF ID 10444 Project Type FSP Type of Trust Fund GET CBIT/NGI CBIT NGI Project Title Development of an integrated system to promote the natural capital in the drylands of Mauritania Countries Mauritania Agency(ies) IUCN Other Executing Partner(s) Executing Partner Type CNEOZA, Ministère de l'Environnement et du Développement Durable Government https://gefportal2.worldbank.org 1/51 5/5/2020 WbgGefportal GEF Focal Area Land Degradation Taxonomy Climate Change Adaptation, Climate Change, Focal Areas, Climate resilience, Livelihoods, Disaster risk management, Land Degradation, Sustainable Land Management, Drought Mitigation, Integrated and Cross-sectoral approach, Improved Soil and Water Management Techniques, Sustainable Livelihoods, Sustainable Pasture Management, Ecosystem Approach, Restoration and Rehabilitation of Degraded Lands, Community-Based Natural Resource Management, Sustainable Agriculture, Income Generating Activities, Food Security, Land Degradation Neutrality, Land Productivity, Influencing models, Transform policy and regulatory environments, Strengthen institutional capacity and decision-making, Convene multi-stakeholder alliances, Private Sector, Stakeholders, Individuals/Entrepreneurs, Large corporations, SMEs, Beneficiaries, Non-Governmental Organization, Civil Society, Community Based Organization, Participation, -

Poverty and the Struggle to Survive in the Fuuta Tooro Region Of
What Development? Poverty and the Struggle to Survive in the Fuuta Tooro Region of Southern Mauritania Dissertation Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Christopher Hemmig, M.A. Graduate Program in Near Eastern Languages and Cultures. The Ohio State University 2015 Dissertation Committee: Sabra Webber, Advisor Morgan Liu Katey Borland Copyright by Christopher T. Hemmig 2015 Abstract Like much of Subsaharan Africa, development has been an ever-present aspect to postcolonial life for the Halpulaar populations of the Fuuta Tooro region of southern Mauritania. With the collapse of locally historical modes of production by which the population formerly sustained itself, Fuuta communities recognize the need for change and adaptation to the different political, economic, social, and ecological circumstances in which they find themselves. Development has taken on a particular urgency as people look for effective strategies to adjust to new realities while maintaining their sense of cultural identity. Unfortunately, the initiatives, projects, and partnerships that have come to fruition through development have not been enough to bring improvements to the quality of life in the region. Fuuta communities find their capacity to develop hindered by three macro challenges: climate change, their marginalized status within the Mauritanian national community, and the region's unfavorable integration into the global economy by which the local markets act as backwaters that accumulate the detritus of global trade. Any headway that communities can make against any of these challenges tends to be swallowed up by the forces associated with the other challenges. -

Mauritania Annual Country Report 2020 Country Strategic Plan 2019 - 2022 Table of Contents
SAVING LIVES CHANGING LIVES Mauritania Annual Country Report 2020 Country Strategic Plan 2019 - 2022 Table of contents 2020 Overview 3 Context and operations & COVID-19 response 7 Risk Management 8 Partnerships 10 CSP Financial Overview 11 Programme Performance 13 Strategic outcome 01 13 Strategic outcome 02 16 Strategic outcome 03 19 Strategic outcome 04 21 Strategic outcome 05 23 Strategic outcome 06 25 Cross-cutting Results 27 Progress towards gender equality 27 Protection and accountability to affected populations 28 Environment 30 Data Notes 30 Figures and Indicators 37 WFP contribution to SDGs 37 Beneficiaries by Sex and Age Group 38 Beneficiaries by Residence Status 38 Beneficiaries by Programme Area 38 Annual Food Transfer 39 Annual Cash Based Transfer and Commodity Voucher 40 Strategic Outcome and Output Results 41 Cross-cutting Indicators 56 Mauritania | Annual Country Report 2020 2 2020 Overview In a context characterized by structural vulnerability and recurring drought-related shocks, often aggravated by sudden crises such as the COVID-19 pandemic and flooding, and in accordance with national priorities and its country strategy plan, WFP continued to play a leading role in supporting Mauritania in setting up an adaptive social protection system (ASP). The ASP is a key element in mitigating the impact of climate change and intense natural shocks. While keeping up addressing the most urgent humanitarian food and nutrition needs, WFP implemented a longer-term resilience approach which combines recovery and long-term productive interventions in a geographically focused, integrated and multi-year manner to reduce food insecurity and malnutrition, enhance education achievements, minimize gender inequalities, strengthen institutional capacities and help communities adapting to climate change hazards.